Physicians are often asked to assess the ability to fly on an airliner safely in a patient with one or more chronic medical conditions. See the post “Managing passengers with stable respiratory disease planning air travel” – Links To The Full BTS Recommendations and To The Primary Care Summary Posted on July 28, 2017
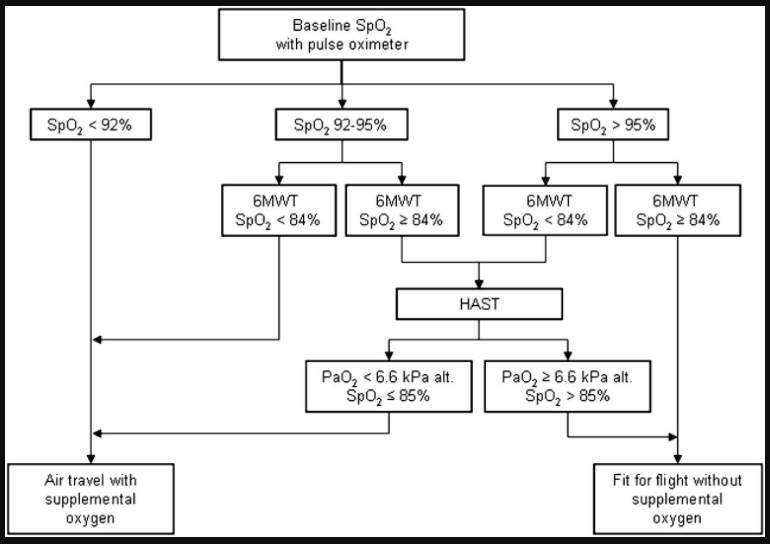
This post discusses a 2012 algorithm involving the use of rest and exercise oximetry with the 6 Minute Walk Test to predict the need for in flight oxygen supplementation. See Resources (1), (2), and (3) below.
Patients with moderately severe or severe COPD can become severely hypoxic on an airline flight. The following excerpts on how to perform a preflight evaluation for potential hypoxia is from Resource (1):
The reduced atmospheric pressure in the aircraft cabin may cause severe in-flight hypoxaemia and respiratory symptoms in patients with lung disease, for example, chronic obstructive pulmonary disease (COPD).1e9 With the growing prevalence of COPD10 and a large proportion of patients with COPD travelling by air,1 9 simple and practical methods for pre-flight evaluation of the patients’ fitness to air travel have been requested.1 3 11
Current air travel statements1 2 12 recommend supplemental oxygen when the arterial oxygen pressure (PaO2) is expected to fall below 6.6 or 7.3 kPa (50 or 55 mm Hg).
The gold standard for evaluation for inflight hypoxia prediction is the preflight hypoxia-altitude simulation test (HAST). Existing prediction equations and rules have not proved adequate for the prediction of inflight hypoxia.
Even though HAST is increasingly used in pre-flight assessment,32 33 it is not widely available.11 21 HAST has been shown to be a good predictor of in-flight PaO2 18 32 34 35 and the results obtained are reproducible.32
The authors of Resource (1) constructed an algorithm to predict inflight hypoxia that was found to be very sensitive and specific.
The sensitivity and specificity for the algorithm in this
independent sample of patients were 100% (95% CI 90% to
100%) and 80% (95% CI 60% to 95%), respectively.
The authors warn that the key to using the algorithm is to perform the six minute walk test accurately:
However, it is important that the 6MWT is performed according to guidelines, and it must be stressed that shortcuts must be avoided.29
Here is the algorithm:
By adding a 6MWT, including measurement of SpO2, the current study shows that the number of patients needing referral to HAST was markedly reduced. The 6MWT is a widely used test to assess exercise performance in patients with COPD, and is much more available than HAST. However, it is important that the 6MWT is performed according to guidelines, and it must be stressed that shortcuts must be avoided.29 The suggested algorithm has a high sensitivity, which was reproduced when applying it prospectively on a separate group of patients with COPD. None of these study subjects were misclassified as fit to fly without supplemental oxygen. Due to somewhat lower specificity, the algorithm overestimated the risk of in-flight hypoxaemia, resulting in unnecessary use of supplemental oxygen in 8% of the patients.According to our results, patients with COPD who have SpO2 SL >95% and without severe exertional desaturation (SpO2 $84%) can travel safely by air without further pre-flight assessment. In addition, further pre-flight assessment is not necessary in patients with SpO2 SL <92%13 23 or in patients with SpO2 SL 92e95% and SpO2 6MWT <84%. These patients should, according to our results, be equipped with supplemental oxygen during the flight.
Thus, extended pre-flight assessment with HAST might be limited to patients with either the combination of resting SpO2 SL >95% and severe exercise desaturation (SpO2 <84%) and to patients with SpO2 SL between 92% and 95% without severe exercise desaturation (> or = 84%). In these two groups of patients, the level of in-flight hypoxaemia was difficult to predict, underlining the need for pre-flight testing with HAST.
Even though HAST is increasingly used in pre-flight assessment,32 33 it is not widely available.11 21 HAST has been shown to be a good predictor of in-flight PaO2. 18 32 34 35
Resources:
(1) Air Travel and Chronic Obstructive Pulmonary Disease: A New Algorithm for Pre-flight Evaluation [PubMed Abstract] [Full Text HTML] [Full Text PDF] Edvardsen A, Akerø A, Christensen CC, Ryg M, Skjønsberg OH Thorax. 2012;67:964-969
(2) COMMENTARY from medscape.com
Evaluating the Safety of Air Travel for COPD Patients Nicholas Gross, MD, PhD
DISCLOSURES January 31, 2013
Dr. Gross comments on Reference (1) above
(3) Air travel for patients with chronic obstructive pulmonary disease: a case report [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Br J Gen Pract. 2012 Feb;62(595):107-8. doi: 10.3399/bjgp12X625328.
(4) Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Thorax. 2011 Sep;66 Suppl 1:i1-30. doi: 10.1136/thoraxjnl-2011-200295.
(5) ATS statement: guidelines for the six-minute walk test [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am J Respir Crit Care Med. 2002 Jul 1;166(1):111-7.
(6) Erratum: ATS Statement: Guidelines for the Six-Minute Walk Test [PubMed Citation] [Full Text HTML] [Full Text PDF]. Am J Respir Crit Care Med. 2016 May 15;193(10):1185. doi: 10.1164/rccm.19310erratum.