In this post, I link to and excerpt from PedsCases‘ Asthma in Preschoolers: CPS Podcast. By dayae.jeong Jun 15, 2021.
All that follows is from the above resource.
This podcast presents an approach to asthma in preschoolers. Listeners will learn how asthma is defined, review the importance of early diagnosis, and master the diagnostic criteria of asthma in a preschooler in the setting of either an acute exacerbation or a non-acute care visit. Further, the recommended appropriate asthma treatment strategies in preschool children will be discussed, as well as when to consider a trial of cessation of asthma controller in preschool children. This podcast was developed by Dr. Dayae Jeong, a pediatrics resident at the University of Toronto, and Dr. Francine Ducharme, pediatrician and past co-chair of the Asthma Assembly of the Canadian Thoracic Society.
Related Content
- Podcast: Acute Asthma Exacerbations
- Podcast: Approach to a Child in Respiratory Distress
- Podcast: Acute Cough
- Case: Respiratory distress in a 4 year old male
DIAGNOSIS AND MANAGEMENT OF ASTHMA IN PRESCHOOLERS: A CANADIAN THORACIC SOCIETY AND CANADIAN PAEDIATRIC SOCIETY POSITION PAPER
CPS Criteria for Asthma Diagnoses in Preschoolers:
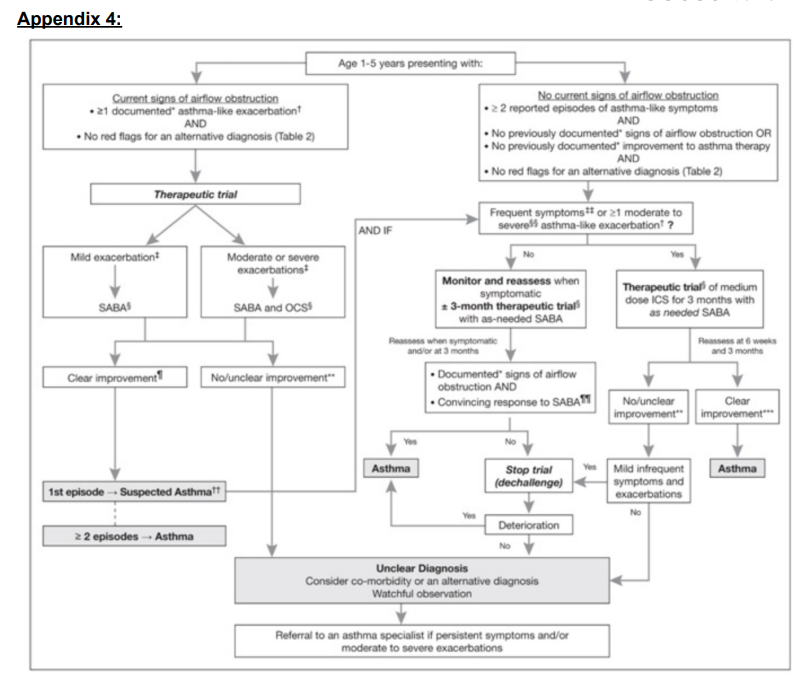
The CPS diagnostic criteria for asthma in preschoolers can be broken down into:1) Presence of airflow obstruction
2) Reversibility of airflow obstruction
3) Recurrent episodes (2 or more) of asthma-like symptoms
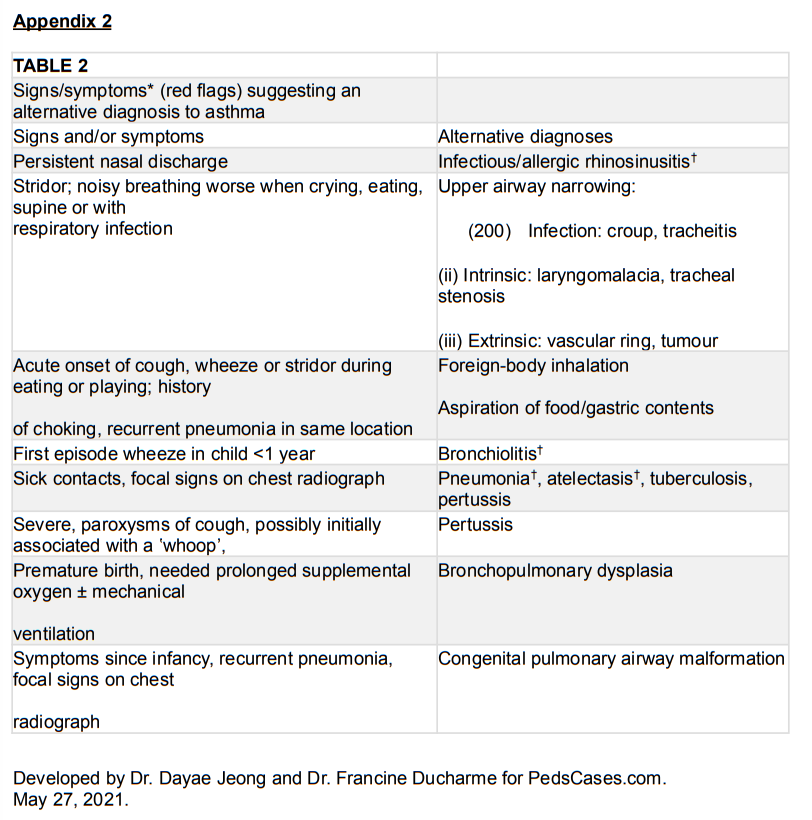
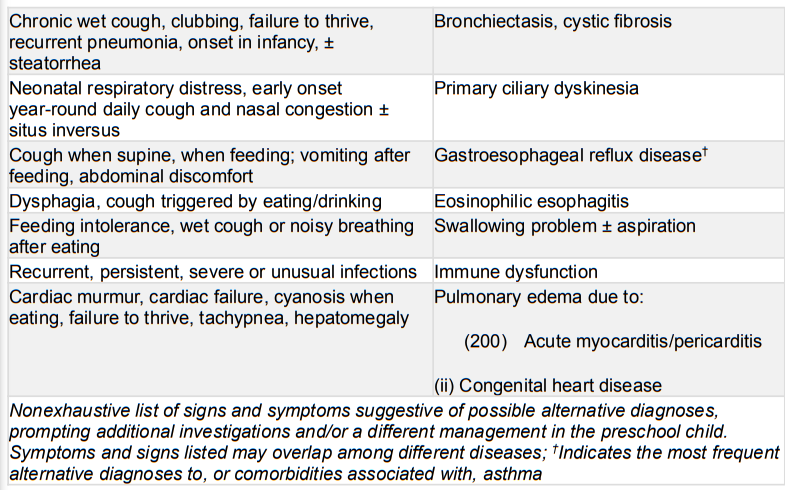
4) No other probable diagnosisA personal or family history of atopy can heighten the suspicion for asthma, but is not necessary for the diagnosis.
Lastly, there are times when a patient should be referred to an asthma specialist for consultation or co-management. These include:
1) Diagnostic uncertainty or suspicion of comorbidity
2) Repeated (at least 2) exacerbations requiring rescue oral steroids or hospitalization,
or frequent symptoms (at least 8 days a month) despite moderate daily doses of ICS
3) Life threatening events such as an ICU admission
4) Need for allergy testing to determine a role of environmental allergies
5) Other considerations like parental anxiety or need for further educationSummary:
And that’s it for our podcast on diagnosing and managing asthma in preschoolers. To recap, here are some take home points:
1) It is important to diagnose preschool asthma as it can be associated with significant morbidity and impact on long-term lung function
2) Asthma can be diagnosed in preschoolers if there are recurrent (>2) episodes of airflow obstruction, with reversibility of the obstruction, and no clinical suspicion for an alternative diagnosis. This can be done if:
a. There are at least 2 episodes where both obstruction and reversibility have been documented by healthcare providers or convincingly reported by the parents
b. There are only one documented or convincingly reported episode of obstruction, with a convincingly reported response to a therapeutic trial of a medium dose of daily inhaled corticosteroid or to as-needed SABA for at least 3 months.
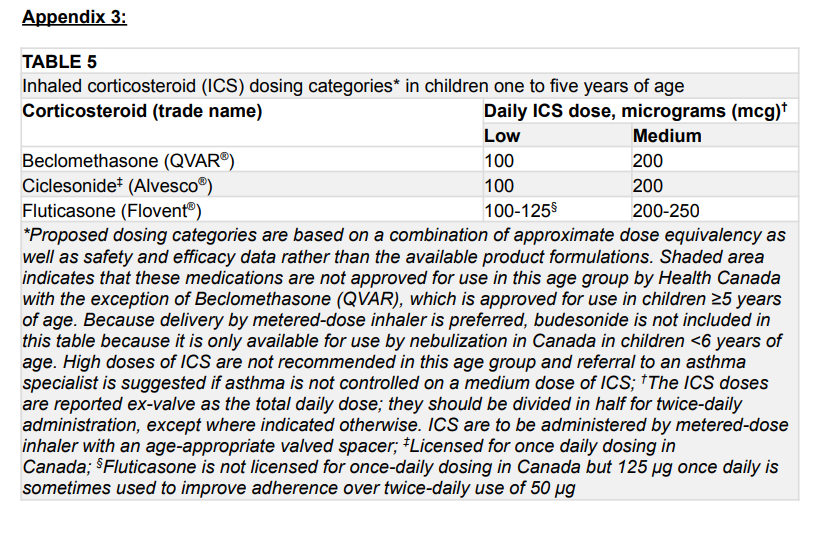
3) For the therapeutic trial, the choice of treatment depends on both the frequency and
severity of symptoms:
a. If the symptoms are mild and infrequent, the trial could be started with an
as-needed SABA only
b. If the symptoms are moderate to severe or frequent, the trial should be started
with a daily ICS at the medium dose, as well as an as needed SABA
c. Emphasizing the importance of adherence to daily ICS (without stopping until the trial is completed), good inhalation technique and close monitoring of symptoms
are keys to adequately interpreting a therapeutic trial.
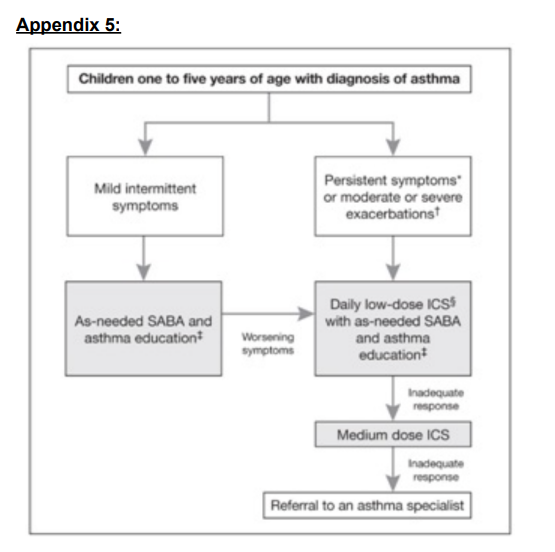
4) After a diagnosis of asthma is confirmed, the choice of treatment to start depends on both the frequency and severity of symptoms while the patient was not on daily ICS:
a. If the symptoms are mild and infrequent, treatment can be started with an
as-needed SABA only
b. If the symptoms are moderate to severe or frequent, treatment with a daily ICS is recommended, with as needed SABA. If satisfactory control has been achieved, a decrease to a low dose of ICS should be considered, aiming for the minimal effective dose. In case of suboptimal control after the dose reduction (assuming good adherence and inhalation technique, no co-morbidity mimicking asthma symptoms and no suspected environmental trigger), increasing to a medium ICS dose should be considered. c. Non-pharmacological strategies such as education on proper spacer technique,
maintaining good adherence, and avoidance of environmental triggers is also
important
5) Frequent follow up is important. 60% of preschoolers outgrow their symptoms by age 6-8
years, so the need for maintenance ICS dosing should be reassessed when symptoms seem to have disappeared particularly despite exposure to a child’s usual unavoidable triggers.References:
Ducharme, F. M. et al. Diagnosis and management of asthma in preschoolers: A Canadian
Thoracic Society and Canadian Paediatric Society position paper. Paediatrics & Child Health
20,353–361 (2015).
Chalut, D. S., Ducharme, F. M. & Davis, G. M. The Preschool Respiratory Assessment Measure
(PRAM): A responsive index of acute asthma severity. The Journal of Pediatrics 137,762–768
(2000).