“Birth asphyxia accounts for about 23% of the approximately 4 million neonatal deaths that occur each year worldwide (Lancet. 2010;375: 1969-1987).”* (p 2)
“Approximately 10% of newborns require some assistance to begin breathing at birth [supplemental oxygen, positive pressure ventilation, tracheal intubation]; fewer than 1% need extensive resuscitation measures to survive [chest compressions, medication administration]. In contrast, at least 90% of newly born babies make the transition from intrauterine to extrauterine life without difficulty.” (p 2)
In getting ready for the Neonatal Resuscitation Program course, I reviewed the 2011 Textbook of Neonatal Resuscitation, 6th ed. But the most valuable resource for me for the course is DVD that is included in every textbook. There are 6 outstanding detailed video resuscitation scenarios with questions for the learner. And there are 19 resuscitation skills videos to be reviewed [unfortunately the 6 resuscitation scenario videos and the 19 resuscitation skills videos are not on the internet, as far as I could tell]. There are excerpts from twelve of the skills videos available online at The Neonatal Resuscitation Website.
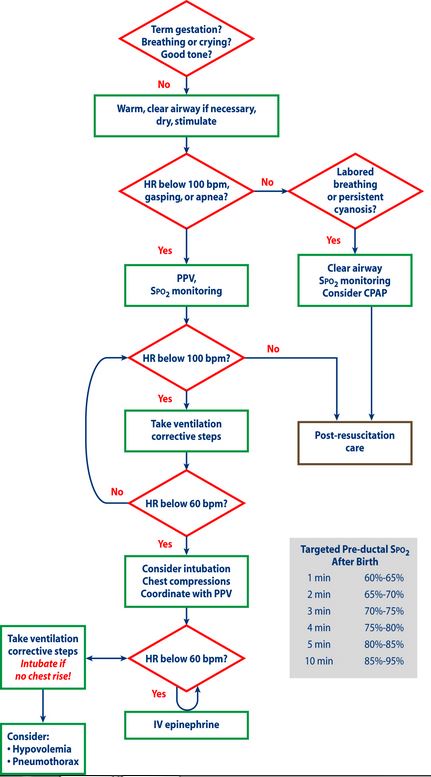
And at the end of the post, I have placed a copy of the NRP algorithm.
What follows are just some notes from the 2011 6th edition of the Neonatal Resuscitation Textbook, that I have reviewed in preparation for the upcoming Neonatal Resuscitation Program that I will be taking shortly (to remain an NRP provider you need to take the NRP every two years).
Every delivery needs to be attended by at least 1 person whose sole duty is to care for the infant. That person must be “capable of initiating resuscitation, including the administration of PPV and assisting with chest compressions.”
The Neonatal Resuscitation Program (NPR) Quick Pre-resuscitation Checklist * (p 34) is critical to successful neonatal resuscitation. The clinician responsible for care of the newborn needs to perform this checklist before each delivery. Doing so will ensure that all equipment needed is available and functioning correctly. [The above link is to a copy of the checklist on my blog post of 9-19-2014]
“What risk factors may be associated with the need for neonatal resuscitation?” * (p 16) [This link is to a copy of the risk factors chart on my blog post of December 1, 2012.]
If a high risk delivery is anticipated because of the presence of identified risk factors before birth [see link above], two skilled neonatal resuscitation providers should be present in the delivery room whose sole duty is to care for the newborn.* (p 17)
When the baby is born there are three questions to be asked and answered: (p 40)
- Was the baby born at term?
- Is the baby breathing or crying?
- Is there good muscle tone?
If the answer to all three questions is yes, then the baby needs Routine Care. (p 20)
“Routine Care: Nearly 90% of newborns are vigorous term babies with no risk factors.Similarly, babies who have prenatal or intrapartum risk factors, but have responded to the initial steps, will need close observation, but may not need to be separated from their mothers after birth to receive close monitoring and further stimulation. Thermoregulation can be provided by putting the baby directly on the mother’s chest, drying the baby, and covering her with dry linen. Warmth is maintained by direct skin-to-skin contact with the mother. Clearing of the upper airway can be provided as necessary by wiping the baby’s mouth and nose. It is recommended that suctioning following birth (including suctioning with a bulb syringe) should be reserved for babies who have obvious obstruction to spontaneous breathing or who require PPV. While the initial steps can be provided in modified form, ongoing observation of breathing, activity, and color must be carried out to determine any need for additional intervention.”* (p 20)
A “vigorous” meconium-stained baby is defined by: *(p 66)
- Strong respiratory efforts
- Good muscle tone
- Heart rate (HR) > 100 beats per minute (bpm) (Assume that a crying baby with good tone has HR > 100 bpm)
A “vigorous” meconium-stained baby is allowed to stay with his mother for routine care.
What are the indications for positive-pressure ventilation?
- If a baby is apneic or if gasping
- If the heart rate is below 100 beats per minute even with [apparently adequate] breathing
- If the heart rate remains below target values despite free flow oxygen being increased to 100%
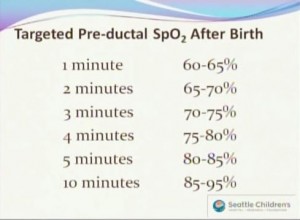 The normal intrauterine oxygen saturation is about 60%. p 52
The normal intrauterine oxygen saturation is about 60%. p 52
“[The oximeter] is considered to be most accurate when SP02 (oxygen saturation) values are between approximately 60% to 90%.
“During a neonatal resuscitation, it is recommended that the oximeter probe be placed on the newborn’s right hand or wrist so as to detect pre-ductal saturation.* (p 57) [Place the oximeter as soon as newborn is found to require resuscitation.]
The ET tubes as they come out of the package are too long. You should shorten the tube to 13 to 15 cm. A 15 cm length may be better to accommodate some ET tube securing devices. [See Resuscitation Skills Video 11 Endotracheal Tube: Emergency Tape Technique (on the DVD).]
Use an 0 blade for premature infants and for extremely premature infants an 00 blade. Use a 1 blade for the term infant.
Always check the laryngoscope blade bulb. Make sure it is tightly screwed in so that it will not flicker and fall out. And attach the blade to the laryngoscope handle to be sure it works when you are doing your equipment check.
A mnemonic to remember the usual tip to upper lip distance of the correctly inserted ET tube: 1 — 2 — 3 [kilograms] –> 7 — 8 — 9 [cm]
“Babies with congenital heart disease are seldom critically ill immediately following birth. Lack of response to resuscitation is almost always because of failure to ventilate the baby the baby effectively.”* (p 247)
“Chest compressions are indicated whenever the heart rate is below 60 beats per minute despite at least 30 seconds of effective positive pressure ventilation.”* (p 136)
“Although chest compressions can be delivered while ventilations are being administered with bag and mask, endotracheal intubation at this point will make ventilation more effective.”* (p 136) [So if you get to the point where you need to do cardiac compressions despite what you believe to be adequate bag mask ventilation, you should go ahead and perform intubation–maybe the problem causing the low heart rate is only a ventilation problem]
“Although you were told earlier [in the textbook] to reassess the effects of your actions approximately every 30 seconds, studies have shown that return of spontaneous circulation may take a minute or so after chest compressions are started. Also, any interruption of chest compressions required to check the heart rate may result in a decrease of perfusion pressure in the coronary arteries. Studies in adults and with animals suggest that there may be a delay of 45 seconds or longer after the compressions are resumed before the coronary artery perfusion pressure returns to its previous value. Therefore, you may want to wait at least 45 to 60 seconds after you have established well-cordinated chest compressions and ventilations before pausing briefly to determine the heart rate again. . . . You should stop administering chest compressions when the heart rate is greater than 60 bpm and concentrate on delivering effective ventilation at the higher rate of 40 to 60 breaths per minute.” [During chest compression, the sequence is 3 chest compressions followed by one breath–one and–two and–three and–breath and–. During chest compression, the goal is 120 events per minute (90 compressions and 30 breaths)]
“If a newborn requires PPV with a mask for longer than several minutes, consider placing an orogastric tube and leaving it in place [to mitigate gastric distension from PPV comprising ventilation].”* (p 99)
“If a baby who required resuscitation continues to show signs of respiratory distress, or has a requirement for supplemental oxygen, consider evaluating the baby for pneumonia or sepsis and consider beginning parenteral antibiotics.”* (p 250)
“If acute respiratory deterioration occurs during or after resuscitation, consider the possibility that the baby may have developed a pneumothorax; or, if the baby has remained intubated after resuscitation, consider the possibility of a misplaced or obstructed endotracheal tube.”* (p 250)
Resources:
*Textbook of Neonatal Resuscitation, 6th ed, 2011. American Academy of Pediatrics and American Heart Association.
See also the resources on this blog in the Neonatal Resuscitation and Neonatology categories.