In this post I link to and excerpt from A Game Plan for the Resumption of Sport and Exercise After Coronavirus Disease 2019 (COVID-19) Infection [Link is to the full text]. HTML JAMA Cardiology, May 13, 2020.
Here are excerpts:
Coronavirus disease 2019 (COVID-19) is associated with significant mortality and morbidity, including adverse cardiovascular sequelae.1 As public health policy begins to guide the resumption of recreational and competitive sport, clinicians are charged with determining when competitive athletes and highly active individuals who have been infected with COVID-19 and recovered are medically appropriate to return to play. There are limited data establishing the epidemiologic and clinical metrics required to facilitate this process. Specifically, the prevalence of asymptomatic COVID-19 cases in the community, the prevalence of cardiac injury among nonhospitalized individuals with COVID-19, and long-term outcomes attributable to COVID-19 cardiac injury remain unknown. Recognizing these limitations, members of the American College of Cardiology’s Sports & Exercise Cardiology Council, with input from national leaders in sports cardiology, provide a consensus expert opinion clinical framework on return to play in the era of COVID-19.
Significant cardiac morbidity has been observed among hospitalized patients with COVID-19. Acute cardiac injury, defined as troponin levels more than the 99th percentile, electrocardiographic and/or echocardiographic abnormalities, occur in up to 22% of hospitalized patients with COVID-19,2 which is significantly higher compared with the approximately 1% prevalence in non–COVID-19 acute viral infections. Myocarditis from myocyte invasion by the virus could result in cardiac dysfunction, arrhythmias, and death. In the acute phase, exercise could result in accelerated viral replication, increased inflammation and cellular necrosis, and a proarrhythmic myocardial substrate. Return to play after myocarditis is predicated on normalization of ventricular function, absence of biomarker evidence of inflammation, and absence of inducible arrhythmias. Risk stratification may occur after 3 to 6 months of exercise restrictions3 and is based on extensive testing including echocardiography, stress testing, and rhythm monitoring.
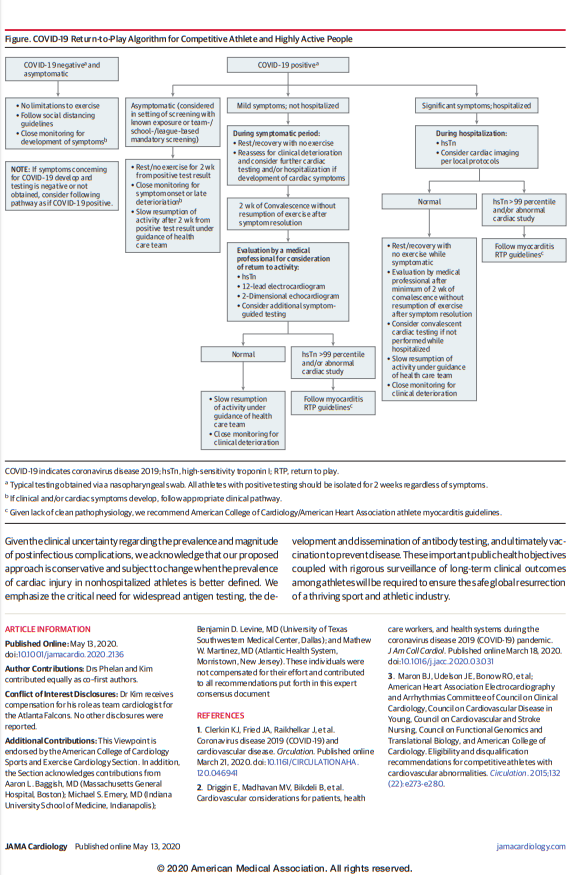
Evidenced-based recommendations for return-to-play guidelines are currently limited and clearly subject to change as further data are obtained in concert with improved COVID-19 case identification. Acknowledging these imperfections, our recommendations are exclusive to cardiovascular considerations and concomitant pulmonary limitations also require consideration. The duration of illness has proved critical in the clinical course of patients infected with COVID-19, with increased risk of clinical deterioration after the first week of symptoms. As such, we recommend an emphasis on the temporal progression of confirmed infection and have incorporated time-based benchmarks in our recommendations
For athletes who remain asymptomatic and are negative for COVID-19, return to exercise training is permissible without additional testing. However, asymptomatic athletes who test positive for COVID-19 antigen (active infection) should refrain from exercise training for at least 2 weeks from the date of positive test result and follow strict isolation guidelines. If athletes remain asymptomatic, slow resumption of activity should be guided under direction from their medical professional. For those asymptomatic individuals with detected COVID-19 antibodies in response to prior infection, we recommend similar evaluation as the asymptomatic athlete with positive COVID-19 test results, and cardiac testing should be considered if there is concern for cardiac involvement.
For athletes who are positive for COVID-19 and develop mild or moderate symptoms, we recommend a minimum of 2 weeks’ cessation of any exercise training from symptom resolution. Whether the increased risk of myocardial injury in hospitalized patients with COVID-19 translates to mildly ill nonhospitalized patients is unknown1 but underscores the need to carefully consider the possibility of cardiac injury among nonhospitalized patients with COVID-19. For recovered individuals ready to resume training after temporal restrictions, we recommend a careful, clinical cardiovascular evaluation in combination with cardiac biomarkers and imaging. Further adjunctive testing with cardiac magnetic resonance imaging, exercise testing, or ambulatory rhythm monitoring should be based on the clinical course and initial testing. With no symptoms and no objective evidence of cardiac involvement, a return-to-exercise training with close clinical follow-up would be reasonable. If testing suggests cardiac involvement, return to play should be based on myocarditis return-to-play guidelines.
Previously hospitalized or more severely ill patients with COVID-19 represent a higher-risk cohort. Acknowledging that myocarditis might not represent the underlying etiology for all hospitalized patients with COVID-19–associated cardiac injury, we recommend following myocarditis return-to-play recommendations.3 For those who were hospitalized with COVID-19 but whose cardiac biomarkers and imaging studies were normal, we recommend a minimum of 2 weeks’ rest after symptom resolution before they undergo careful clinical cardiovascular evaluation with consideration of repeated cardiac testing, followed by a graded resumption of exercise.
Recommendations regarding resumption of intense exercise training and competition requires careful consideration of the severity of prior infection and the likelihood of cardiovascular involvement. The approach provided in this Viewpoint is intended to assist clinicians in this process. Given the clinical uncertainty regarding the prevalence and magnitude of postinfectious complications, we acknowledge that our proposed approach is conservative and subject to change when the prevalence of cardiac injury in nonhospitalized athletes is better defined. We emphasize the critical need for widespread antigen testing, the development and dissemination of antibody testing, and ultimately vaccination to prevent disease. These important public health objectives coupled with rigorous surveillance of long-term clinical outcomes among athletes will be required to ensure the safe global resurrection of a thriving sport and athletic industry.
References
- Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. Published online March 21, 2020. doi:10.1161/CIRCULATIONAHA.120.046941PubMedGoogle Scholar
- Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. Published online March 18, 2020. doi:10.1016/j.jacc.2020.03.031Google Scholar
- Maron BJ, Udelson JE, Bonow RO, et al; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology, Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and American College of Cardiology. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities. Circulation. 2015;132(22):e273-e280.PubMedGoogle Scholar