In this post, I link to and excerpt from The Cribsiders‘ #26: Neonatal HSV – Plain and Simplex. MAY 26, 2021 By DR JUSTIN BERK.
All that follows is from the above excellent podcast and show notes.
Neonatal HSV Pearls
- There are three well defined manifestations of postnatal HSV: mucocutaneous disease (Skin, eye, mouth disease), encephalitis, and disseminated HSV disease.
- HSV infection is treated with 20mg/kg acyclovir IV every 8 hours. For SEM disease, treatment course is 14 days. For disseminated disease or meningoencephalitis, treat for 21 days.
- After initial treatment, neurodevelopmental outcomes are improved if children are placed on long-term HSV prophylaxis to prevent recurrent disease.
- The consequences of perinatal HSV can be devastating. It is important to be vigilant for these infections.
What is Herpes Simplex Virus?
Herpes Simplex Virus (HSV) is a double stranded DNA virus. Two types: HSV1 and HSV2, which have different glycoproteins. Primary infection can lead to latent infection, where the virus is dormant in the dorsal root ganglion. Reactivation can occur during times of stress and is when the virus can be transmitted.
Why are we worried about newborns with HSV?
The first 30 days of life are a uniquely vulnerable time as neonates have a developing immune system. Neonates exposed to HSV during the first 30 days of life are at high risk of developing infection, however the infection acquired at this time can present up to about 6 weeks of age.
- 85% of infections arise from exposure during the delivery process
- 10% of infections arise from postnatal exposure (e.g. from kissing the baby with a cold sore or transmission by herpetic whitlow)
- Rarely, can be acquired as an intrauterine infection
3 Common Manifestations of Postnatal HSV
These three well defined manifestations of disease occur as a continuum:
- Mucocutaneous disease (Skin, eye, mouth disease) where findings are only related to the skin, eyes, or mucous membranes (45% of cases)
- Encephalitis (30% of cases)
- Disseminated HSV disease, this is the most severe (25% of cases)
How prevalent is HSV?
One in 6 adults is seropositive for HSV. This is consistent over time through multiple studies. One 2003 prospective study by Zane Brown et al looked at the incidence of disease in the neonate and found it to be 1/3,200 cases annually. This estimates 1200 – 1500 cases annually in the US.
Risks Factors for Peripartum Transmission
In pregnant patients who have been appropriately treated with prophylaxis, certain factors can increase and decrease the risk of vertical transmission.
Increased likelihood of vertical transmission:
- Pregnant/delivering patient having active lesions or asymptomatic shedding at the time of delivery (however, no indication from OB literature to routinely screening pregnant patients for shedding at the time of delivery)
- New (primary) HSV infection during pregnancy, especially in the third trimester. This is because of higher viral load and because the pregnant person does not have the ability to transfer protective antibodies to the baby
- Disruption of mucocutaneous barriers (like a fetal scalp electrode)
Decreased likelihood of vertical transmission:
If the pregnant patient has active lesions at the time of delivery, this is an indication for c-section for both primary and recurrent infection. The risk for vertical transmission of HSV is about 40-60% in primary infections and <5% in recurrent infection with active lesions.
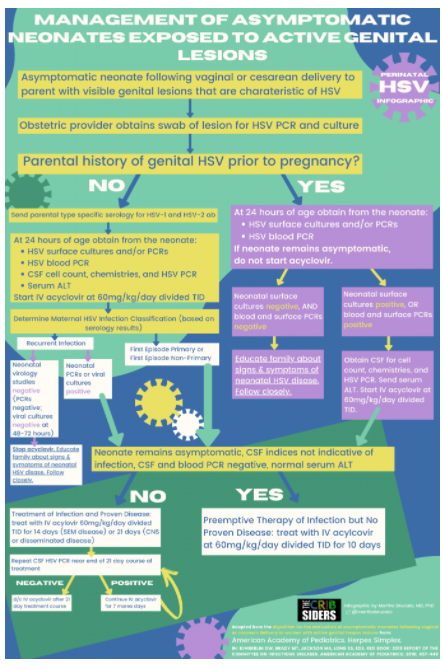
Caring for Asymptomatic Neonates
Pregnant patients with or without a history of HSV should have a speculum exam at time of presentation to look for vaginal lesions (algorithm based on the Red Book (2018) and the Guidance on management of asymptomatic neonates born to women with active genital herpes lesions). In laboring patients with active lesions during delivery (either vaginal or c-sections), obstetricians should get a swab of the lesion for either PCR or culture assay. PCR is a better test for HSV than culture (faster results) but it is not available at every hospital. Treatment algorithm breaks into 2 trees:
- If the parent had genital HSV prior to pregnancy, we assume lesions represent recurrent infection. The baby does not require a higher level of care and can remain in the newborn nursery or room-in with the parent. If the baby is asymptomatic at 24 hours of age, we obtain surface cultures and/or PCRs and blood PCR. No treatment and we wait on results.
- If the parent did not have a history of HSV prior to pregnancy, we obtain serologies for HSV1 and HSV2 to help us determine if this is a recurrent or a primary infection. Then (even if asymptomatic), at 24 hours, the baby gets cultures, blood PCR, CSF analysis, serum transaminase analysis. We start the baby on antiviral treatment with acyclovir.
We wait until 24 hours of life in the above cases to obtain cultures because we don’t want the interpretation of results to be confused by the presence of parental secretions at the time of collection (by 24 hours, vernix likely wiped off).
Natural history of Untreated HSV
If a pregnant parent has antibodies prior to delivery, there is a possibility of a milder course for neonatal disease. If a patient developed a third trimester infection without time to develop antibodies, there is a risk of more severe disease.
Disease does not always occur in the immediate newborn period! The average onset of neonatal HSV disease (both SEM and disseminated disease) is 10-12 days. The average onset of HSV encephalitis is 16-19 days of age.
In neonates with risk factors, there are no pathognomonic symptoms. For example: there are neonates who get HSV who never develop a rash! In a Kimberlin and colleagues 2001 study, in all patients with symptomatic HSV disease, 68% of neonates had evidence of skin vesicles at the time of presentation, so 32% of children did not have a rash! With the most severe disease (disseminated HSV), 40% may not show any obvious signs of disease except that they are ill-appearing. Babies with HSV can present with fever, lethargy, poor PO intake, tachycardia, and anything that indicates the infant is not well appearing.
How to counsel parents
Provide anticipatory guidance at the time of discharge: if your child is not eating well, not well appearing, feels hot or cold, is difficult to wake up, has unusual movements, bring them to the emergency room. If that happens, please tell the ED physicians that there is a parental history of HSV and whether or not they were treated for HSV.
Who’s at highest risk?
In one study from 1997, 1-2% of pregnant patients seroconverted (developed HSV antibodies) during pregnancy. 64% of individuals in that cohort converted asymptomatically, meaning they never knew they had HSV. Known personal history of HSV prior to pregnancy may actually be protective, since the patient would have antibodies during pregnancy to confer protection via placental transfer; whereas asymptomatic seroconversion or third trimester seroconversion actually confers increased risk for neonatal HSV.
HSV1 and HSV2 are equally virulent and able to cause disease in neonates. There has been a change over time in the infection patterns of HSV1 with an increasing frequency of HSV1 genital infections.
The immune system in preterm infants is immature and they have a decreased immune response. Preterm infants also have less effective barriers (skin and lung) to protect against pathogens. For example, preterm infants have skin that is not yet normally keratinized and is very gelatinous. Prematurity is a risk factor for more invasive disease because (1) preterm infants have a decreased immune response and (2) pregnant patients are not routinely started on valacyclovir suppression until 36 weeks gestation.
Symptomatic Patients
In the case of a symptomatic infant (trouble latching, hypothermic, irritable) prior to 24 hours of life: start evaluation for HSV and for bacterial infections (Group B strep, E.coli, listeria—always consider these in the differential even if the parent has a history of HSV and we’re suspicious for HSV infection).
Evaluation for a sick infant consists of:
Start here.