Note: The show notes of this podcast are an outstanding summary of the systematic evaluation of chronic diarrhea.
In this post, I link to and excerpt from The Curbsiders‘ #267 Diarrhea Disemboweled Part 2: Chronic Diarrhea with Dr. Iris Wang. APRIL 7, 2021 By DR ELENA GIBSON.
All that follows is from the above outstanding resource.
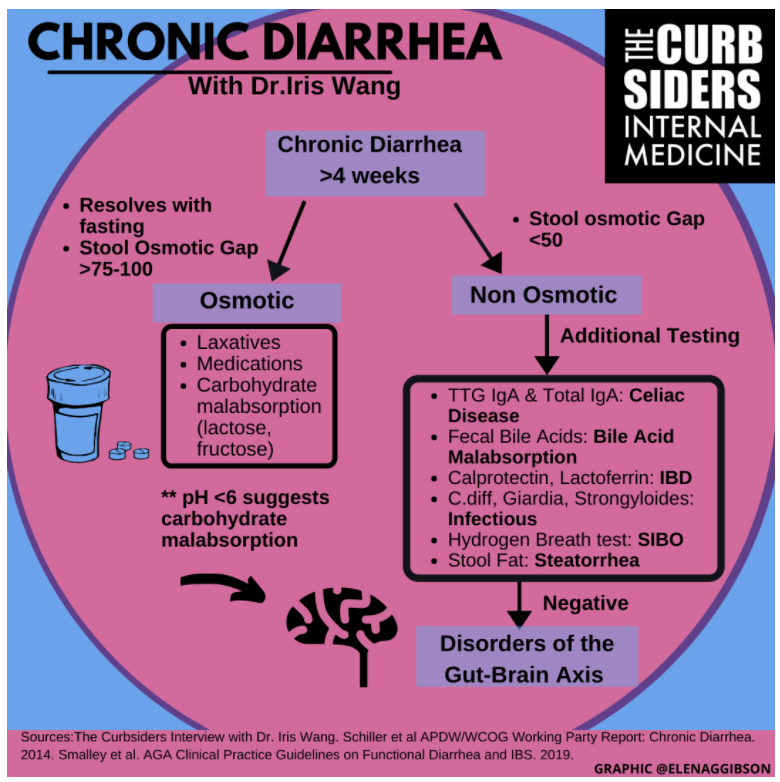
Flow with us through Diarrhea Disemboweled Part 2 as Dr. Xiao Jing (Iris) Wang @IrisWangMD walks us through the differential diagnosis and initial evaluation of chronic diarrhea.
Transcript-#267-Diarrhea-Disemboweled-Part-2-Chronic-Diarrhea
Show Segments
- Intro, disclaimer, guest bio
- Case from Kashlak
- Osmotic diarrhea & stool osmotic gap
- Causes of osmotic Diarrhea
- Algorithm for evaluating diarrhea workup
- Testing workup for chronic diarrhea
- Endoscopic evaluation indications
- Disorders of the Gut-Brain Axis
Chronic Diarrhea Pearls
- Chronic diarrhea is defined as diarrhea present for >4 weeks.
- Determine if chronic diarrhea is osmotic or not by 1) asking if the symptoms resolve with fasting and 2) calculating the stool osmotic gap.
- A stool osmotic gap of <50 is normal and >100 is elevated, suggesting the presence of unmeasured osmoles.
- In osmotic diarrhea, a stool pH <6 suggests carbohydrate malabsorption.
- Additional etiologies of non-osmotic diarrhea include 1) Celiac disease 2) Chronic infections 3) Inflammatory Bowel Disease 4) Small intestinal bacterial overgrowth 5) Bile Acid malabsorption 6) Fat malabsorption 7) Pancreatic exocrine insufficiency and 8) Disorders of the Gut-Brain Axis.
- Consider bile acid malabsorption in patients with prior small bowel resection of <100cm (liver overproduces bile acids) and fat malabsorption if small bowel resection >100cm (liver cannot compensate for loss in resorption).
- When using cholestyramine, remember to check for medication interactions.
- Fecal elastase-1 is a useful initial test for the evaluation of pancreatic exocrine insufficiency.
- If suspicion is high for bile acid malabsorption or pancreatic exocrine insufficiency, empiric treatment with a bile acid binder or pancreatic enzyme replacement respectively could be considered.
- When treating pancreatic exocrine insufficiency in a patient with reduced gastric acid production (eg after gastric surgery), the use of pre-activated enzymes should be considered.
Chronic Diarrhea Notes
Initial Evaluation
*Recap from Acute Diarrhea episode (Riddle 2016)
Diarrhea is defined as
- > 3 liquid or loose bowel movements in 24 hours (or more frequently than normal for an individual)
- More objective definition is stool weight >200g of stool per day
Categorize by Timing
- Acute: <2 weeks
- Persistent: 2-4 weeks
- Chronic: >4 weeks
Dr. Wang notes there is often overlap in the pathophysiology of chronic diarrhea (ie. secretory vs osmotic, non-inflammatory vs inflammatory), and fitting the diagnosis into one specific category is often more academic than clinically relevant. Therefore, Dr. Wang recommends categorizing chronic diarrhea by 1) osmotic diarrhea 2) non-osmotic diarrhea.
Osmotic diarrhea is defined by the presence of a stool osmotic gap. To determine if diarrhea is osmotic (Schiller 2014)
- Ask, “what happens when you stop eating?”. Osmotic diarrhea should resolve with fasting. Other causes of diarrhea might improve with fasting, but they will not resolve.
- Send stool electrolytes to calculate the stool osmotic gap.
Stool Osmotic Gap
Stool osmotic gap= 290-(2*Na+K).
Stool electrolytes (Na, K) are used to calculate the stool osmotic gap. The function of the bowel is to maintain stool osmolality=serum osmolality. If measurable stool osmoles don’t add up to ~290 (serum osmolality) then unmeasured osmoles are present (Schiller 2014). A stool osmotic gap of <50 is normal and >100 is elevated, suggesting the presence of unmeasured osmoles. Stool osmolality is rarely ordered because to ensure accuracy it would need to be measured before any bacteria in the stool have a chance to perform fermentation (ie. immediately). One of the only indications for measuring osmolality is factitious diarrhea (Schiller 2014).
Etiologies of Osmotic Diarrhea
The differential for osmotic diarrhea includes ingestion of unmeasured osmoles including magnesium-based laxatives (eg in sleep aids), phosphorous, carbohydrate malabsorption, and sugar alcohols (hard candies) (Schiller 2014). Stool pH <6 suggests carbohydrate malabsorption as bacteria in the colon ferment the carbohydrate and decrease stool pH (Schiller 2014). Fructose can also lead to osmotic diarrhea. Glucose and other single sugars are transferred across our gut by GLUT transporters, and most of them are facilitative transporters. However, fructose is a diffusion transporter. When fructose is ingested with glucose it can be facilitated, but fructose in excess of glucose needs to go through its own transporter and that is only a diffusion transporter. So, if ingested fructose >> glucose, the excess fructose can cause diarrhea.
Non-Osmotic Chronic Diarrhea
First, differentiate if the diarrhea is osmotic or not. Then, look into the following:
- Red flags: blood in stool, weight loss
- Surgical history: prior cholecystectomy, pancreatic resection, etc.
- Take a thorough medication history. Make sure to ask about potential common culprits: metformin, SSRIs.
Additional Testing
After evaluating for osmotic diarrhea and asking about red flags, surgical history, and medication use, an additional workup for other causes of diarrhea should include (Smalley 2019):
- Infectious testing for organisms that can cause chronic diarrhea: Giardia, Strongyloides, C. diff
- Celiac testing -TTG IgA and total IgA for screening to make sure not missing celiac
- Fecal calprotectin or lactoferrin– to evaluate for inflammatory causes of diarrhea
- Bile Acid Testing- fecal bile acid secretion
- SIBO testing- carbohydrate breath test
- Stool Fat – lipophilic stain (Sudan stain), quantitative fecal fat
- Lactose Hydrogen Breath Test
Fecal calprotectin or lactoferrin are specific to the colon, so they can rule out UC but not Crohn’s. Compared to CRP, they are better markers for the evaluation of colitis. CRP has a sensitivity of ~50% and 73% specificity for IBD where fecal calprotectin has a 92% sensitivity and 82% specificity.
Bile Acid Malabsorption (BAM)
BAM is classically seen in patients with malabsorption from a prior cholecystectomy or ileal Crohn’s disease. Bile acid reabsorption is impaired so the acids make it into the colon and cause secretory diarrhea due to colonic irritation (Camilleri 2020). Gold standard testing for bile acid malabsorption is 48-hour stool testing and fat collection. From this, total bile acids and the percentage of primary bile acids are quantitated (Smalley 2019). If suspicion for bile acid malabsorption is high enough, empiric treatment with cholestyramine or another bile acid binder is reasonable. However, testing to ensure the diagnosis is recommended as these medications will not help if BAM is not present and they 1) interact with the absorption of other medications 2) taste bad 3) and require frequent dosing.
Small bowel resection can also lead to significant bile acid malabsorption. When <100cm of small bowel is resected, a reduction in bile acid reabsorption sends feedback to the liver leading to net overproduction of bile acids that enter the colon. If a patient with <100cm resected is having diarrhea, there is a high likelihood they are not absorbing bile acids and an empiric trial of a binder is reasonable. When >100cm is resected, the liver is not able to keep up and there is a net loss of bile acids ultimately leading to fat malabsorption. This is important because if patients with fat malabsorption take a bile acid binder, their diarrhea will worsen (Parrish 2020)!
Small intestinal bacterial overgrowth (SIBO)
SIBO occurs when bacteria in the small bowel ferment products that would otherwise be absorbed leading to symptoms of bloating, diarrhea, and malabsorption (Schiller 2014). The gold standard for diagnostics is a culture of luminal fluid from the small intestine, but breath tests of carbohydrate fermentation are more commonly used (ie hydrogen breath with lactulose or glucose substrates). The results of these tests should be interpreted with caution given risk of inaccuracies, particularly with lactulose testing. Risk factors for SIBO include things that increase bacterial presence or decrease gut motility allowing increased bacterial growth.
- Increase bacteria: PPI, DM, cirrhosis, immunosuppression
- Stasis: diverticula, Roux-en-Y, DM, scleroderma, radiation
The ileocecal valve is responsible for decreased bacteria in the small bowel compared to the colon. Surgical removal or pathologic damage to the valve leads to an increased risk of bacterial reflux. In some people, the valve becomes more incompetent with age causing increased bacterial reflux into the small bowel.
Fat Malabsorption
Testing for fecal fat: a spot fecal fat is a useful test with good correlation to quantitative fecal fat (via a 72 hour stool collection) (Schiller 2014). Spot fecal fat testing is completed with a Sudan stain, which has an approximate sensitivity of 76% and a specificity of 99% for fat being present in the stool. If the lab can quantify the fat present, the sensitivity is approximately 94% and specificity is 95% specificity. The caveat about measuring fecal fat: speed, motility, and absorption time matter. If diarrhea is present due to rapid transit time from another etiology, fat malabsorption will often occur. So, just because fecal fat is present, it does not mean it is the driving etiology of diarrhea unless you quantify the fat. For example, following laxative use, 35% of healthy adults will meet the criteria for mild steatorrhea based on fecal fat testing. This is why quantifying the fecal fat provides a more specific diagnosis. The cut-off for steatorrhea is 14g of fat per 24h.
Pancreatic Exocrine Insufficiency
Fecal elastase-1 testing is a fairly sensitive and specific test for pancreatic insufficiency (Lindkvist 2013). The diagnostic “gold standard” is a secretin stimulation test where secretin is administered and then bicarbonate response is measured in the duodenum. However, this is rarely done given the need for endoscopic coordination. If suspicion is high, empiric treatment with pancreatic enzyme replacement is often completed to see how patients respond. Things to remember about enzyme replacement: 1) one must give adequate doses of enzyme replacement (this depends on the specific formulation) and 2) most of the pancreatic enzymes depend on gastric acid to break through the pill coating and activate the enzymes. If someone is on a chronic PPI or has another reason for decreased gastric acid (gastric surgery), then prescribe a pre-activated formula (eg Viokase).
When is Endoscopy Needed?
If a patient is not up to date on colorectal cancer screening and has diarrhea with weight loss, iron deficiency anemia, or other red flags a colonoscopy should be completed as CRC can cause obstruction with overflow diarrhea. If there is evidence of malabsorption (iron deficiency, decreased vitamin B12, weight loss, fat malabsorption, or vitamin D deficiency) an EGD with duodenal biopsies to evaluate for causes of malabsorption should be completed (looking for celiac, Whipple’s disease, CVID, SIBO). If a patient is up to date on CRC screening but all initial screening for the source of chronic diarrhea is negative consider a flex sig to obtain random biopsies for microscopic colitis.*
*See Microscopic Colitis: A Challenging Disorder [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Dig Dis. 2020;38(2):117-121.
Disorders of the Gut-Brain Axis
Chronic diarrhea from disorders of the Gut-Brain Axis, or Gut-Brain Interaction (ie irritable bowel syndrome (IBS)) is common. There is not a serologic or imaging test to diagnose them. If the workup for organic etiologies of diarrhea is negative, the Rome IV criteria can be used to diagnose IBS (Lacy 2021). When diagnosing disorders of the Gut-Brain Axis, Dr. Wang recommends starting with validation and explanation of the condition. If patients are interested in a trial of diet therapy to aid with symptoms the low FODMAP diet can be helpful. If the patient has access to a dietician, Dr. Wang recommends referral to help with the initiation of the low FODMAP diet to avoid malnutrition from elimination and to help with reintroduction as the low-FODMAP diet should NOT be for life. If dietician access is not available, serial elimination is recommended with the elimination of one common offending food group at a time (instead of removing all at once and adding them back at once) to avoid nutritional deficiency. Loperamide, Diphenoxylate/Atropine, tincture of opium, and octreotide can be used as anti-diarrheal medications (Lacy 2021). Additional complementary therapies to trial include yoga (D’Silva 2019) and hypnotherapy (Peters 2016).
Links
Link for Acute diarrhea episode
RELEVANT PRIOR CURBSIDERS EPISODES
#27 Conquer Irritable Bowel Syndrome
#95 Food Intolerance & Celiac Disease
#138 Inflammatory Bowel Disease
OTHER MEDIA