In this post I link to and excerpt from The Curbsiders‘ January 28, 2021 Episode #251: Preventive Medicine Updates with Dr. Amber-Nicole Bird.
Here is the podcast embedded below:
Here are excerpts:
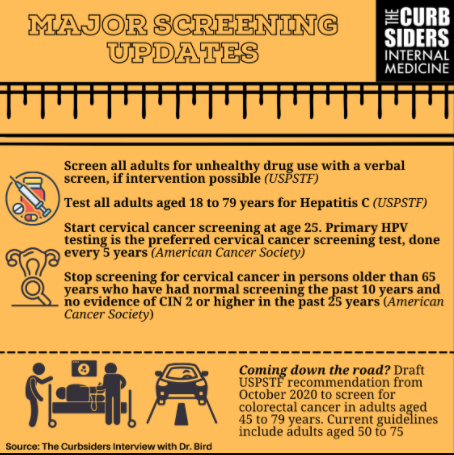
Screening for Unhealthy Drug Use
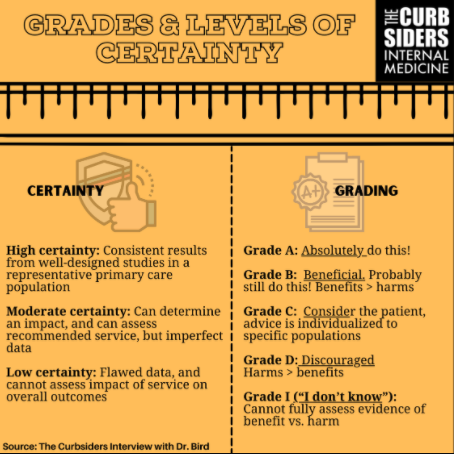
- USPSTF recommends screening for unhealthy drug use in adults age 18 years or older (Grade B, moderate certainty)
- Different from screening for tobacco and alcohol use, which are addressed in different guidelines
- Per USPSTF, data show net benefit to screening for unhealthy drug use, IF you can effectively offer treatment directly or via referral
- Driven in part by data for medications for opioid use disorder, as well as some behavioral health interventions
- Guideline is specifically for VERBAL screening
- No indication for laboratory-based screening
- Dr. Bird favors the NIDA screening tool for unhealthy drug use
- Includes screening for alcohol and tobacco use as well
- Links to the ASSIST tool, which can provide recommendations for management
Screening for Hepatitis C
- USPSTF recommends screening everybody aged 18-79 years at least once for hepatitis C infection
- Upper age limit based on existing safety data of treatment
- Grade B recommendation, with moderate certainty of substantial net benefit
- Based on availability of effective, low harm treatments and increased prevalence of hepatitis C infection in adults
- Screen with antibody testing as initial test, with reflex to RNA testing
Cervical Cancer Screening
- As with much in preventive care, there are multiple screening guidelines from different societies and organizations
- USPSTF guidelines, updated in 2018 (Grade A, high certainty)
- Added on the option of primary high risk HPV testing every 5 years in ages 30-65 (alone or co-testing with cytology).
- Cytology alone every 3 years is still an option in age 30-65, and the recommended method for age 21-29.
- American Cancer Society updated their guidelines in 2020
- Increased age to initiate screening to 25 years
- Incidence of cervical cancer in women ages 21-24 is low
- Accounts for less than one percent of patients with cervical cancer
- Primary HPV testing every 5 years until the age of 65 years is preferred testing for all women undergoing cervical cancer screening
- If not available, co-testing every 5 years or cytology only every 3 years (this is a transitional recommendation; will be removed from future guidelines)
- Provides clear recommendations to stop screening after the age of 65 years
- Requires adequate and normal screening for the 10 years prior
- No CIN 2 or higher in past 25 years
- Recommendation to phase out cytology probably based in part on impact of HPV vaccination
- Incidence of cervical cancer is declining following routine HPV vaccination
- Cytology less efficient in vaccinated populations
- Disproportionately detects minor abnormalities associated with HPV types that are at lower risk of causing cancer
Colorectal Cancer Screening
- USPSTF released draft recommendation for colorectal cancer screening in October of 2020
- Part of a process to put up recommendations for public comments
- Insurance may not cover screening recommendation changes until they are finalized
- Draft recommendation recommends screening for colorectal cancer in adults aged 45 to 79 years (Grade B, moderate certainty) and adults aged 50 to 75 years (Grade A, high certainty)
- Screening modalities can be stool-based (high-sensitivity guaiac-based FOBT, fecal immunochemical test, and stool DNA test) or direct visualization (colonoscopy, CT colonography, and flexible sigmoidoscopy).
- USPSTF also recommends selectively offering colorectal cancer screening in adults aged 76 to 85 years (Grade C, moderate certainty)