In this post, I link to and excerpt from Dr. Josh Farkas‘ chapter, Meningitis & Encephalitis, from his outstanding Internet Book Of Critical Care [Link is to the Table Of Contents].
All that follows is from the above Meningitis & Encephalitis:
CONTENTS
- Rapid Reference
- Background: meningitis vs. encephalitis
- When to suspect CNS infection
- Imaging
- Lumbar puncture
- Management
- Additional discussion of specific pathogens
- Podcast
- Questions & discussion
- Pitfalls
rapid reference
approach to obtunded patient with suspected meningitis/encephalitis
labs
- Fingerstick glucose STAT.
- Electrolytes, complete blood count with differential, coagulation studies.
- Blood cultures x2.
- HIV screen as appropriate.
initial empiric therapy (more)
- 2 grams ceftriaxone IV
- 10 mg dexamethasone IV.
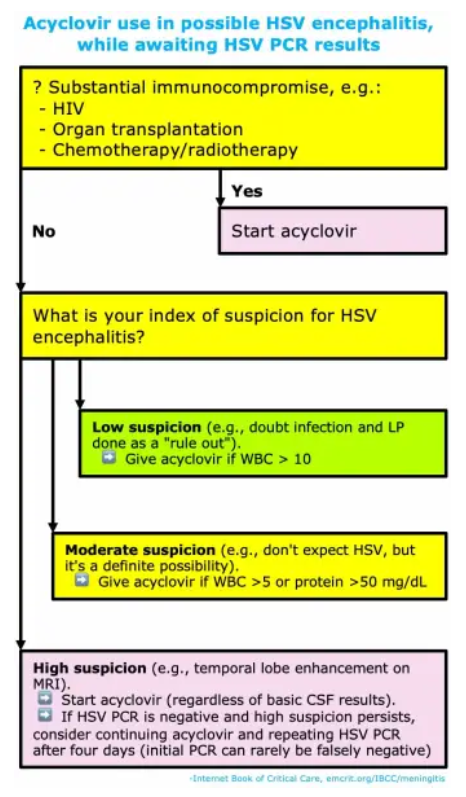
- 10 mg/kg acyclovir IV.
diagnostics
- Discontinue DVT prophylaxis to facilitate lumbar puncture.
- Head CT scan.
- Lumbar Puncture:
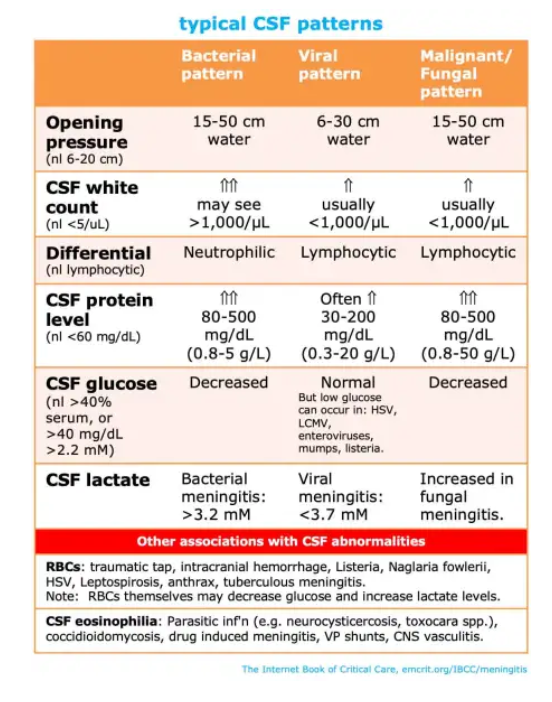
- Measure opening pressure & LP labs.
- Target MAP > [60 + 0.7(Opening Pressure in cm)]
- MRI/MRV if possible (for the obtunded patient, this will generally require intubation).
fever prevention
- Scheduled acetaminophen (1,000 mg PO q6hr for most patients).
- External cooling if needed to achieve normothermia.
seizure control (more)
- If concern for seizures, obtain EEG.
- Consider levetiracetam for seizure prophylaxis.
PITFALLS
- Failure to give steroid along with antibiotic. Steroid is recommended by both US and European guidelines, based on prospective RCTs proving reduction in long-term neurologic disability.
- Under-utilization of ultrasound-guided lumbar puncture for morbidly obese patients (if you’re sending patients for IR-guided lumbar puncture, consider ultrasound).
- Delaying steroid/antibiotic therapy (e.g. for lumbar puncture, blood cultures, etc.).
- Failing to check VZV PCR (this is seen occasionally, so if you’re going to get HSV PCR it’s worth getting VZV also).(23566589)
- Keep in mind that antibiotics often require higher doses to penetrate the meninges (“meningeal dose”). Thus, simply because the patient is on an antibiotic doesn’t mean that meningitis is necessarily covered adequately.
- Recognize that a patient with meningitis/encephalitis and obtundation is critically ill, and should usually receive care in an ICU.