Pediatric Trauma is always stress-inducing. Here are two great resources from Emergency Medicine Cases:
- Pediatric Trauama – Rapid Video Review
- This 7:48 video is an a quick review of EMC Episode 95
- Episode 95 Pediatric Trauma
- This outstanding podcast is 1:40:01 and worth every second of your time.
_________________________________________________________
Here are some excerpts from Pediatric Trauama – Rapid Video Review:
Pediatric Trauma is stressful because of all the below:
 The most important thing you need to be good at – is the Primary Survey and in a small emergency department, you may be responsible for performing all these roles:
The most important thing you need to be good at – is the Primary Survey and in a small emergency department, you may be responsible for performing all these roles:
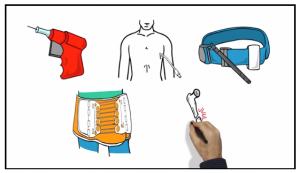
No doctor or nurse can know everything. But every doctor and nurse who works in an emergency department and may see pediatric (or adult) trauma needs to know how to to do five things:
- Place an Intraosseous Line
- Place a Chest Tube
- Place a Tourniquet
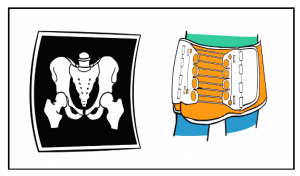
- Place a Pelvic Binder
- Reduce a Long Bone Fracture
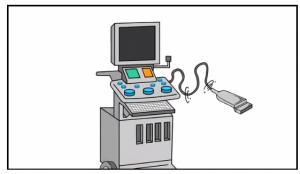
And you need to learn how to do a FAST exam*. But remember that a positive FAST is helpful but a negative FAST does NOT rule out intra-abdominal injury.
*Here are some links to my blog posts on learning the FAST and other emergency ultrasound exam:
- The eFAST Ultrasound Exam by Critical Care Specialist Dr. Liz Turner
- Fastest Way To Learn Point Of Care Ultrasound and Best Book For Getting Started In Point Of Care Ultrasound
- The RUSH Ultrasound Exam by Critical Care Specialist Liz Turner, MD
Know your hospital’s blood availability and how to get it.
Checkout U of T’s Trauma App for implementing or updating your site’s massive trauma protocol and other trauma related guidelines. [Download from iTunes or from Google Play]
Adult Trauma Resuscitation 2:33 – 3:06]
In the adult world . . . damage control resuscitation can help prevent severe downstream pathology and coagulopathy that potentially worsens patient outcomes.
Being comfortable with minimizing saline, with a palpable pulse, and being comfortable with a person who is coherent is stressful but ultimately best for hemostasis.
Giving TXA as early as possible and keeping the patient warm support clot stability.
But ultimately blood should be given to achieve a perfusing pressure. The key indications [for blood] include a systolic blood pressure of less than 90 systolic or an altered level of consciousness.
Childhood Trauma Resuscitation 3:07 – 3:44
This remains a controversial topic in pediatric resuscitation. Giving 10 to 40 ml per kilo of warmed crystalloid prior to blood is reasonable in pediatric polytrauma patients who present in compensated shock.
But early administration of blood components is absolutely vital in patients who present in decompensated shock.
Remember that hypotension is a late finding in pediatric shock that you want to avoid as it truly signifies a peri-arrest situation.
Remember if a kid is adult in size, treat them like an adult. But permissive hypotension is not an accepted principle in young children. And TXA is a consideration.
We encourage calling pediatric trauma doctor early.
There are so many elements to consider. Careful attention to basic airway management is critical. And if intubation is indicated have your backup plan ready.
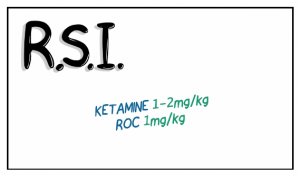
If an R.S.I is indicated we recommend keeping things simple. Ketamine at 1 – 2 mg per kg and rocuronium at 1 mg per kg is a good place to start.
We don’t routinely pretreat with atropine anymore but having it available in case of a bradycardic response to intubation is not a bad idea when you’re managing the airway of an infant or a toddler.
Definitely remember post intubation sedation and analgesia. It is best to have a plan upfront for ongoing needs.
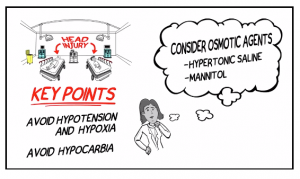
In head injury in a child or adult:
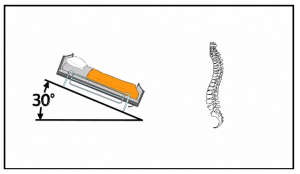
Elevate the head of the bead by 30 degrees but be mindful of your potentially spine injured patients.
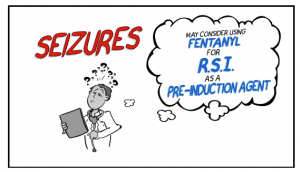
Sedate and treat seizures aggressively.
Lastly avoid hypoglycemia and check this early in the altered child.
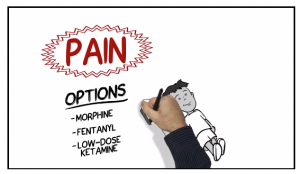
Do not neglect to treat pain in children.
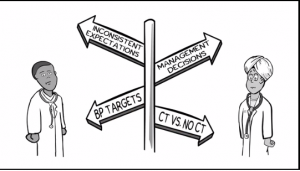
Sending physicians are often given mixed messages on when to image and when to simply package and send. This can be frustrating and can lead to delays at both ends.
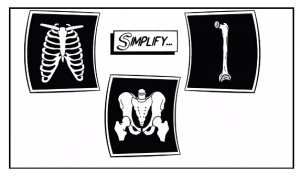
To simplify, in the potentially sick patient, do imaging that you can act on like a chest x-ray to guide chest tubes, long bone x-rays to identify fractures that can and should be reduced, pelvic xrays if you are suspicious for fracture.
But if your patient is unstable, just bind the pelvis.
Contact a trauma physician when ever you have questions and for support in these very uncommon and very stressful pediatric trauma patients.
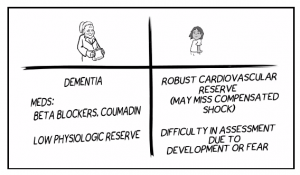
The extremes of age should lower your threshold to transfer. A serious injury may be much more subtle in these patients as their physiologies and co-morbidities may present unique challenges to diagnosis and treatment.
Don let your patient lay around upon a backboard [because complications occur]. Get them off of it as soon as possible.
Having a transport checklist provides a tool for ensuring that your patient has everything they need to be moved out of your department.
___________________________________________________________
Here are some excerpts from the show notes of Episode 95 Pediatric Trauma:
Common pitfalls leading to bad pediatric trauma outcomes
Failure to:
Manage the airway – indicated for almost all severe TBI, any hypoxia
Appreciate and treat shock – do not wait for hypotension which is a sign of pre-arrest
Prioritize management of injuries – see “CABC” below
Check bedside sugar if altered LOC – ABCDEFG “Don’t Ever Forget the Glucose”
Keep the child warm
Preparation before the pediatric trauma patient arrives:
Use a Broselow tape to draw up all anticipated medications in advance of patient arrival: ketamine 2mg/kg or etomidate 0.3mg/kg, rocuronium 1mg/kg or succinylcholine 1-2mg/kg, fentanyl 2-5mcg/kg, atropine 0.02 mg/kg etc., and to size airway equipment (have one size larger and one size smaller ready as well).
Venous access: Prime lines, have IOs ready, central line kit.
Warm the room, turn on the overhead warmer (for infants) or Bair hugger (for older children), warm crystalloids, set the rapid infuser.
Have pelvic binder or sheet laid out on stretcher with clamps ready.
Team huddle: see Andrew Petrosoniak’s approach to team-based preparation for a critical event.
PRIMARY SURVEY PEARLS
C-A-B-C: A new paradigm in pediatric traumaATLS has revently moved from the ABC approach to the CAB for trauma resuscitation. Our experts suggest the “CABC” approach: First, identify any catastrophic bleeding, then move on to airway and breathing with a plan to return to circulation assessment.
In general, respect the range of vital signs in the pediatric population. 90th percentile normal pediatric vital signs HERE
Disability: AVPU (Alert, Voice, Pain, Unresponsive) is adequate. Pediatric GCS is also acceptable but not always practical as it is difficult to remember.
Exposure: Important in any trauma patient, but keep in mind increased heat loss in children
Family Presence: Evidence suggests that family presence reduces stress on families and the patient without compromising team dynamics or medical care.