The following is from p S67 of Resource (2)
The following text is from pp S71 +S72
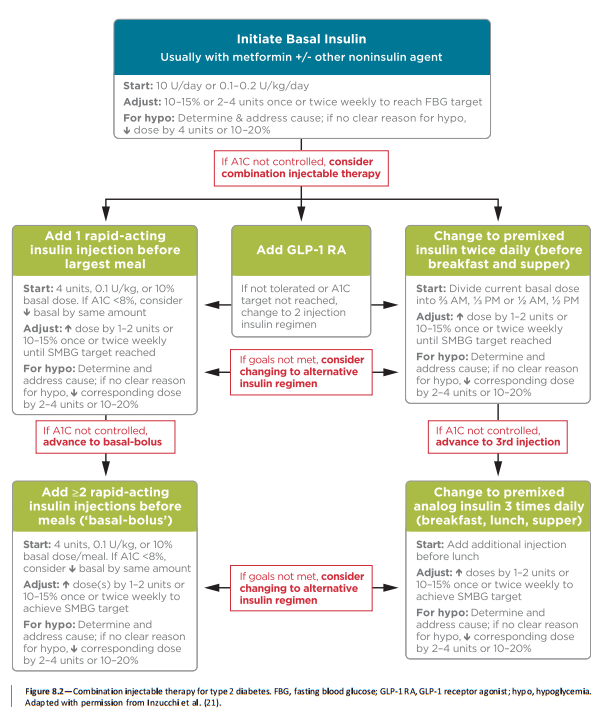
Insulin Therapy
Many patients with type 2 diabetes eventually require and benefit from insulin therapy. The progressive nature of type 2 diabetes should be regularly and objectively explained to patients. Providers should avoid using insulin as a threat or describing it as a sign of personal failure or punishment.
Equipping patients with an algorithm for self-titration of insulin doses based on self monitoring of blood glucose (SMBG) improves glycemic control in patients with type 2 diabetes initiating insulin (34)*. Comprehensive education regarding SMBG, diet, and the avoidance of and appropriate treatment of hypoglycemia are critically important in any patient using insulin.
*Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets – the TITRATETM study [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Diabetes Obes Metab. 2009 Jun;11(6):623-31. doi: 10.1111/j.1463-1326.2009.01060.x.
- The following text is from pp S72
Basal Insulin
Basal insulin alone is the most convenient initial insulin regimen, beginning at 10 units per day or 0.1–0.2 units/kg/day, depending on the degree of hyperglycemia. Basal insulin is usually prescribed in conjunction with metformin and sometimes one additional noninsulin agent. While there is evidence for reduced risk of hypoglycemia with newer, longer-acting basal insulin analogs, people with type 2 diabetes without a history of hypoglycemia may use NPH insulin safely and at much lower cost (27,35). Table 8.3 provides average wholesale price information (cost per 1,000 units) for currently available insulin products in the U.S. There have been substantial increases in the price of insulin over the past decade and the cost-effectiveness of different antihyperglycemic agents is an important consideration when selecting therapies (36). A follow-on U-100 (100 units/mL) glargine product (basaglar) is now available in the U.S. This product was approved through an abbreviated FDA approval pathway based, in part, on the FDA’s finding of safety and effectiveness for the reference U-100 glargine product.
Bolus Insulin
Many individuals with type 2 diabetes may require mealtime bolus insulin dosing in addition to basal insulin. Rapid-acting analogs are preferred due to their prompt onset of action after dosing. The recommended starting dose of mealtime insulin is 4 units, 0.1 U/kg, or 10% of the basal dose. If A1C is ,8% (64 mmol/mol) when starting mealtime bolus insulin, consideration should be given to decreasing the basal insulin dose.
Premixed Insulin
Premixed insulin products contain both a basal and prandial component, allowing coverage of both basal and prandial needs with a single injection. NPH/Regular 70/30 insulin, for example, is composed of 70% NPH insulin and 30% regular insulin. The use of premixed insulin products has its advantages and disadvantages, as discussed below in COMBINATION INJECTABLE THERAPY.
Resources:
(1) CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2017 EXECUTIVE SUMMARY [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Endocr Pract. 2017 Feb;23(2):207-238. doi: 10.4158/EP161682.CS. Epub 2017 Jan 17.
(2) AMERICAN DIABETES ASSOCIATION STANDARDS OF MEDICAL CARE IN DIABETES—2017 [Full Text PDF]. January 2017 Volume 40, Supplement 1.
(3) Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets – the TITRATETM study [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Diabetes Obes Metab. 2009 Jun;11(6):623-31. doi: 10.1111/j.1463-1326.2009.01060.x.




