Timing of Anticoagulation Reinitiation
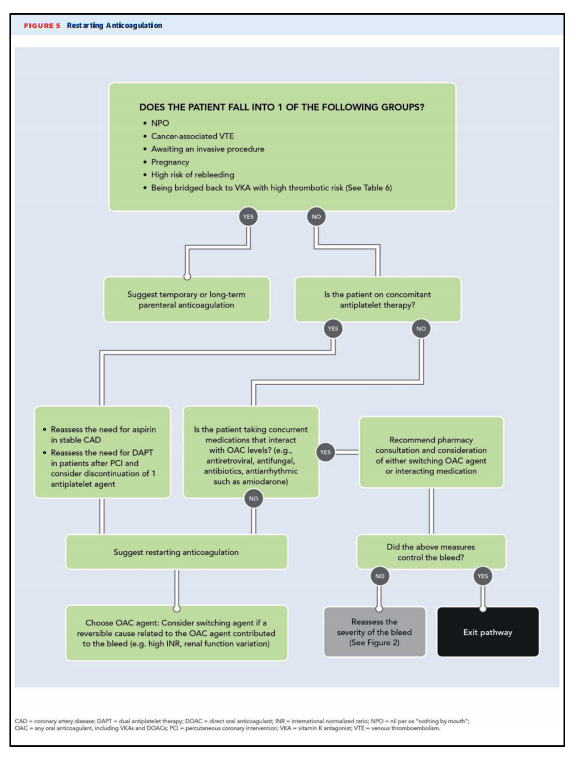
Figure 5 provides clinical guidance for situations in which it is recommended that the patient restart anticoagulation.
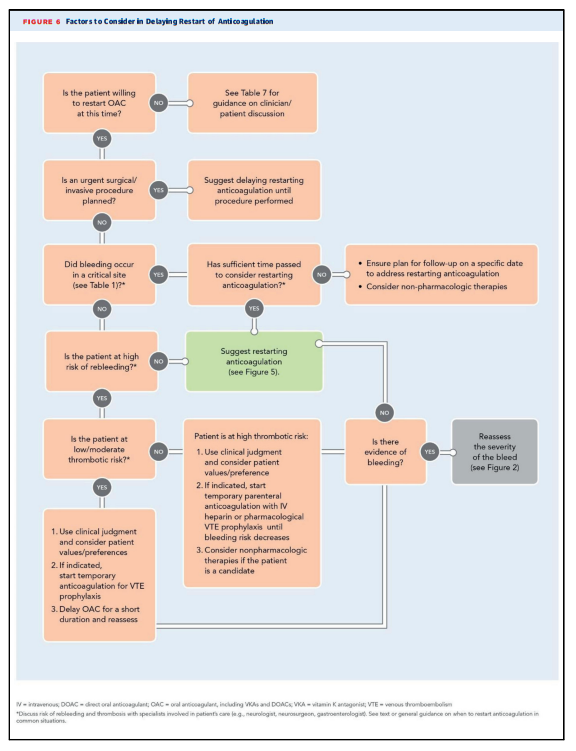
Figure 6 provides clinical guidance for situations where it is recommended that the patient delay restart of anticoagulation.
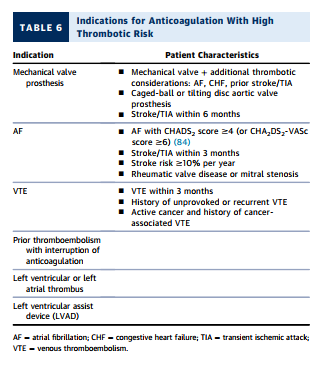
Determining the optimal timing for reinitiation of OAC has the dual therapeutic aim of preventing thrombotic events while minimizing rebleeding. In general, conditions with high thrombotic risk (see Table 6) [at the very top of this web page-TW] favor early reinitiation of anticoagulation once hemostasis is achieved and the patient is clinically stable. OAC may be reinitiated with close monitoring in patients with high thrombotic risk; for patients with moderate or high rebleeding risk, individualized strategies are appropriate. For example, parenteral anticoagulants can often be started with close monitoring within 1 to 3 days in most patients. For patients at high rebleeding risk for whom the thrombotic risk is unacceptably high and therapeutic anticoagulation is deemed necessary, it is suggested that unfractionated heparin be administered by intravenous infusion, due to its short half-life and an available reversal agent (protamine sulfate) that can rapidly stop and/or reverse anticoagulation in the event of rebleeding
The use of prophylactic doses of parenteral anticoagulants (e.g., subcutaneous unfractionated or low-molecular-weight heparin) at the bottom of p 15 and the top of p 18 of the pdf.
In patients with both a high thrombotic risk and high bleeding risk resulting in a relative or absolute contraindication to restarting anticoagulation, nonpharmacological therapies may be considered
In general, temporary interruption of OAC for a short duration is likely appropriate for most patients without high thrombotic risk as rebleeding may lead to further prolonged anticoagulant interruption and exposure to thrombotic risk. Changing the anticoagulant used may also be considered when restarting anticoagulation after a bleeding event. In cases where identifiable risk factors (e.g., impaired renal function) were associated with a bleeding event, it may be appropriate to consider alternative anticoagulants.