Please be sure to review Linking To And Excerpting From Metabolic Mind CME’s “The Ketogenic Diet as a Treatment for Type II Diabetes”
Posted on January 2, 2026 by Tom Wade MD
Today, I link to and embed Metabolic Mind CME‘s Managing Major Mental Illness with Dietary Change: The New Science of Hope, Georgia Ede, M.D.
All that follows is from the above resource.
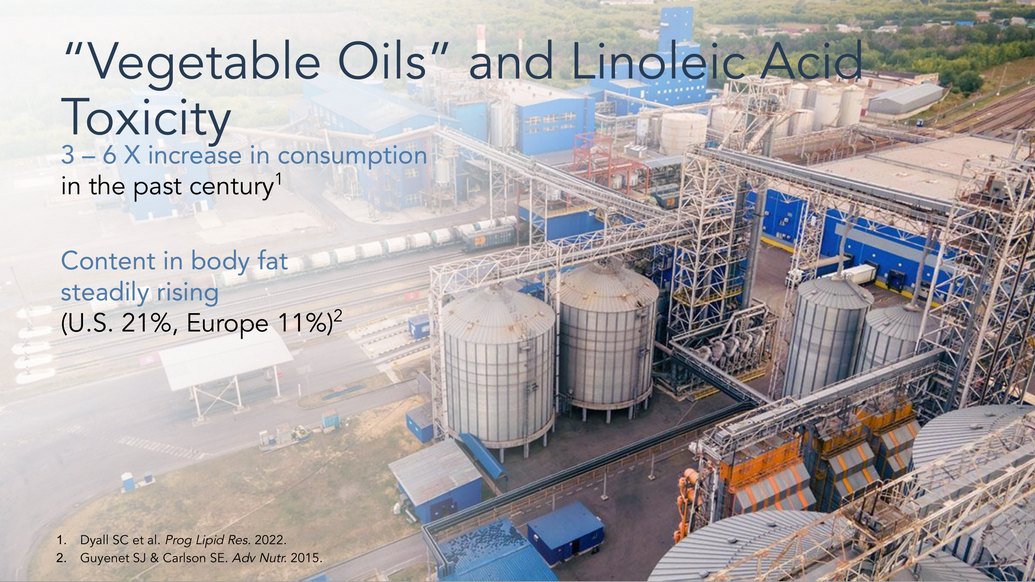
In her discussion of slide 16 Dr. Ede recommends avoiding refined vegetable oils and against linoleic acid toxicity.
Georgia Ede, M.D. – Figure 16
“Vegetable Oils” and Linoleic Acid
What about vegetable oils? We didn’t have the technology to create vegetable oils until about a hundred years ago, and they really didn’t start pouring into our food supply until about the 1960s, when the American Heart Association declared them heart-healthy. In many packaged foods, healthy fats from whole animal and plant foods have been replaced with vegetable oil. One of the many problems with vegetable oils is that they’re exceedingly high in a fragile omega-6 fatty acid called linoleic acid. Linoleic acid does exist normally in plant and animal foods in very, very small amounts. But products like soybean and safflower oil wrangle it out of a seed and concentrate it.While it is normal for the body to store saturated fat, it is not normal to store polyunsaturated linoleic acid. Before the industrialization of our diet, our fat cells contained at most 4% linoleic acid. Now, its about 11% in Europe and 21% in America. This can lead to a variety of problems in the rest of the body, which we won’t go into today. The brain absorbs linoleic acid just as well as it absorbs any other polyunsaturated fatty acid, so is this a problem?
The brain is supposed to burn small molecules like glucose and ketones. It’s not supposed to be burning fatty acids for energy, as that creates extra inflammation and oxidative stress. But the brain does burn almost all of the linoleic acid that enters for energy, and that’s not normal. Whether the inflammation and oxidative stress come from sugar and flour and cereals and vegetable oils, or whether they come from smoking or alcohol consumption, too much inflammation and oxidative stress can translate into mental illness.
I did a Google search “How do you remove refined vegetable oils from your diet?” Here is the link.
Georgia Ede, M.D. – Figure 26
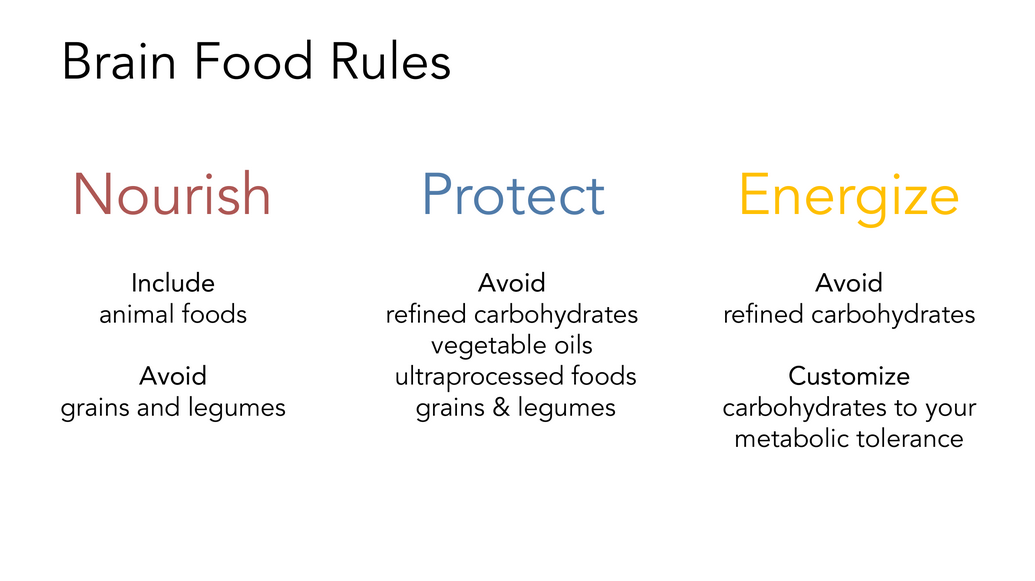
Brain Food Rules
Now we want to create a set of brain food rules that make biological sense. To summarize how best to nourish the brain, include some animal foods and avoid grains and legumes. To protect the brain, avoid refined carbohydrates, vegetable oils, and ultra-processed foods. To energize the brain, keep your blood sugar and insulin levels in a healthy range. To accomplish that, depending on how metabolically healthy or unhealthy you are, maybe all you have to do is avoid refined carbohydrates. But for many of us, we will need to reduce our overall carbohydrate intake because we no longer process carbohydrates properly. That might mean eating a low glycemic index diet, a moderately low carbohydrate diet, or a ketogenic diet.
I did a Google search “How do you remove refined vegetable oils from your diet?” Here is the link.
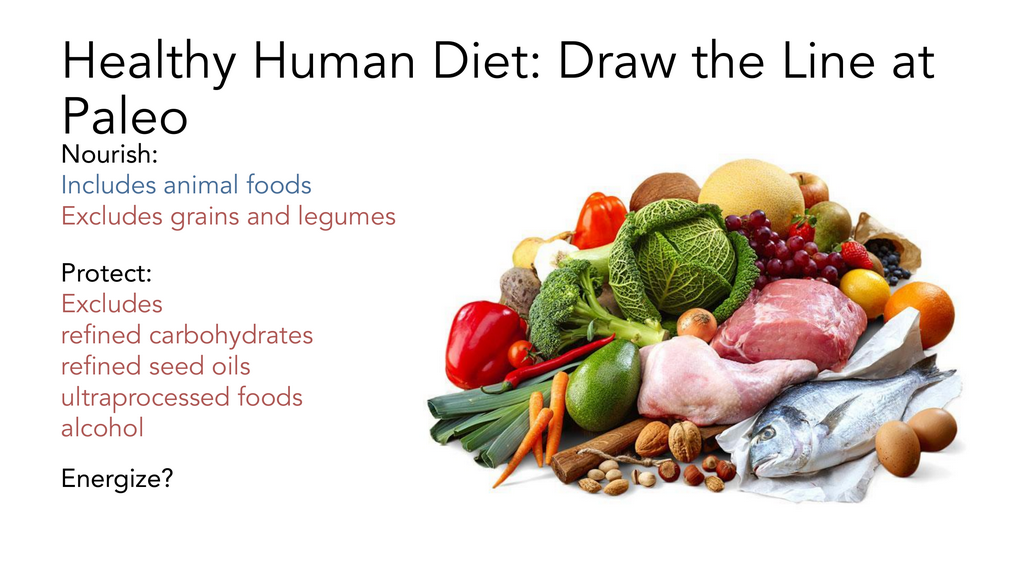
Georgia Ede, M.D. – Figure 28
This is why I recommend that we draw the line at Paleo, which excludes grains, legumes, and ultra-processed foods like refined carbohydrates and vegetable oils. Rather, it is based on animal foods and whole plant foods. So, Paleo nourishes and protects the brain relatively well. But in terms of energizing the brain, it allows as much carbohydrate from fruits and vegetables as you like. That’s going to be fine for some of you, and it’s not going to be fine for others.
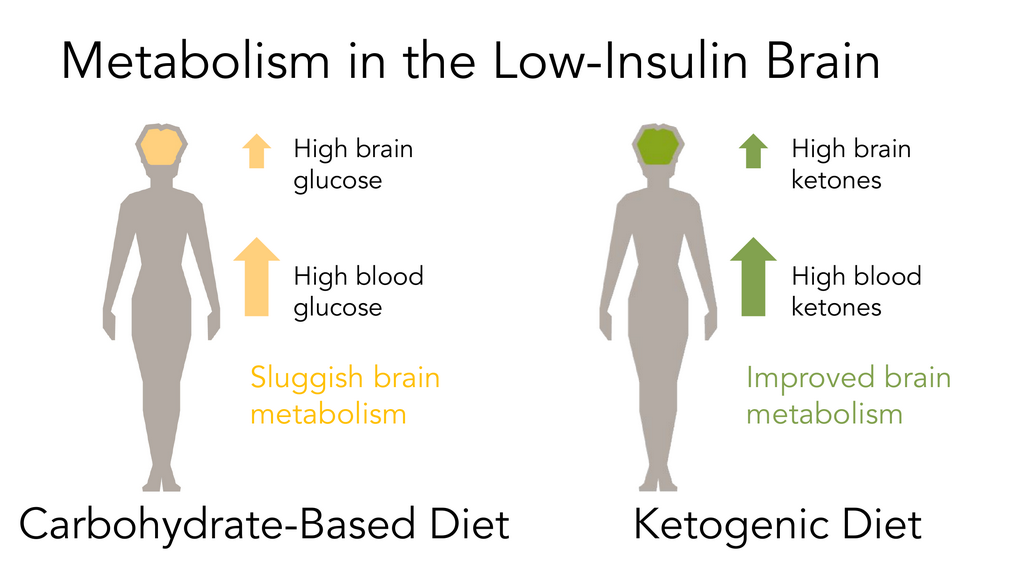
Georgia Ede, M.D. – Figure 29
The reason why metabolic psychiatrists like myself focus on the ketogenic diet is because insulin resistance and high insulin levels can be targeted beautifully with a ketogenic diet. In addition, a ketogenic diet leads to high levels of blood ketones. Ketones easily cross the blood-brain barrier and can be used by the brain as fuel, even in the setting of severe insulin resistance. The more ketones you have in the blood, the more that will enter the brain to help bridge the energy gap left by cerebral glucose hypometabolism.
Georgia Ede, M.D. – Figure 30
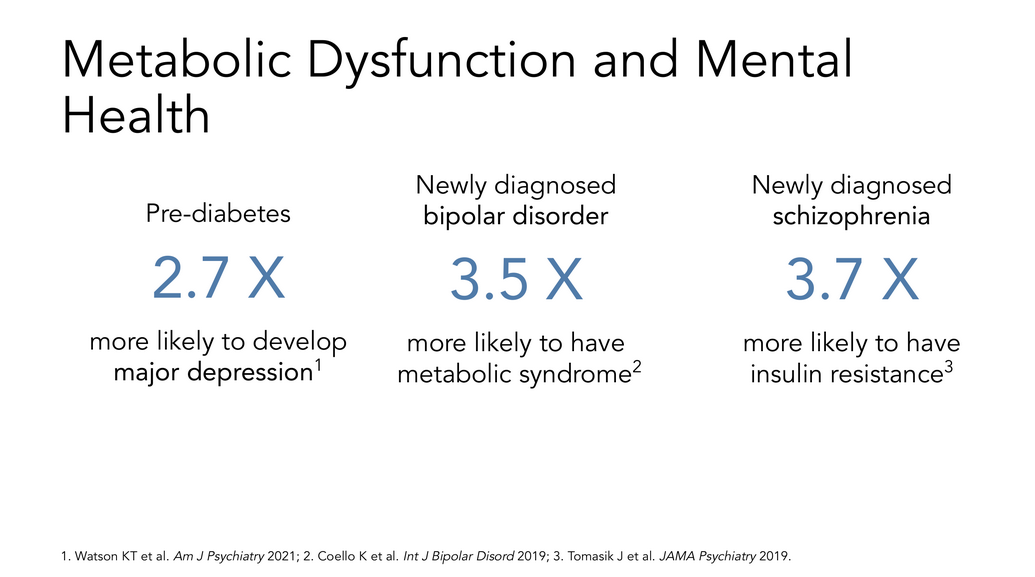
This is important because there’s a very strong association between these metabolic problems and mental illnesses. If you have any mental health condition, you are about 3x more likely to have a metabolic health condition, and vice versa. As to whether this relationship is association only, or if there is a causal component, we’re getting closer to determining that there is a causal component. Insulin resistance is playing a role, at least in the severity and course of certain mental illnesses, if not actually helping them to develop in the first place.
Georgia Ede, M.D. – Figure 31
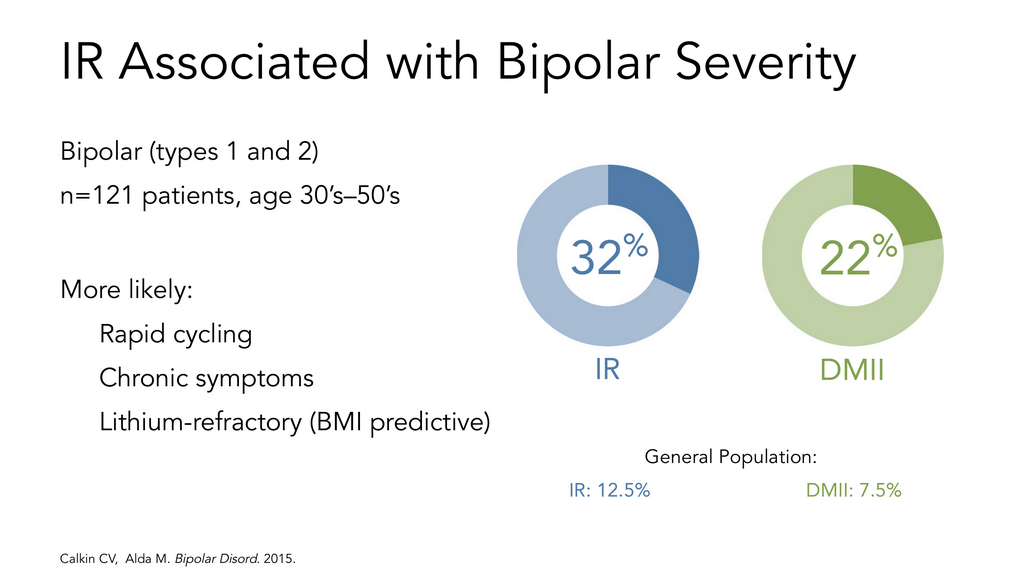
Some of the best information we have that points to a causal relationship comes from Dr. Cynthia Calkin, a metabolic psychiatrist specializing in bipolar disorder at Dalhousie University in Nova Scotia. She’s found that her patients with bipolar disorder are 3x more likely to have insulin resistance or type 2 diabetes. In those same patients, those with insulin resistance or type two diabetes and bipolar disorder are more likely to have rapid-cycling mood. They’re also more likely to have chronic symptoms and less likely to respond to the mood-stabilizing drug lithium.
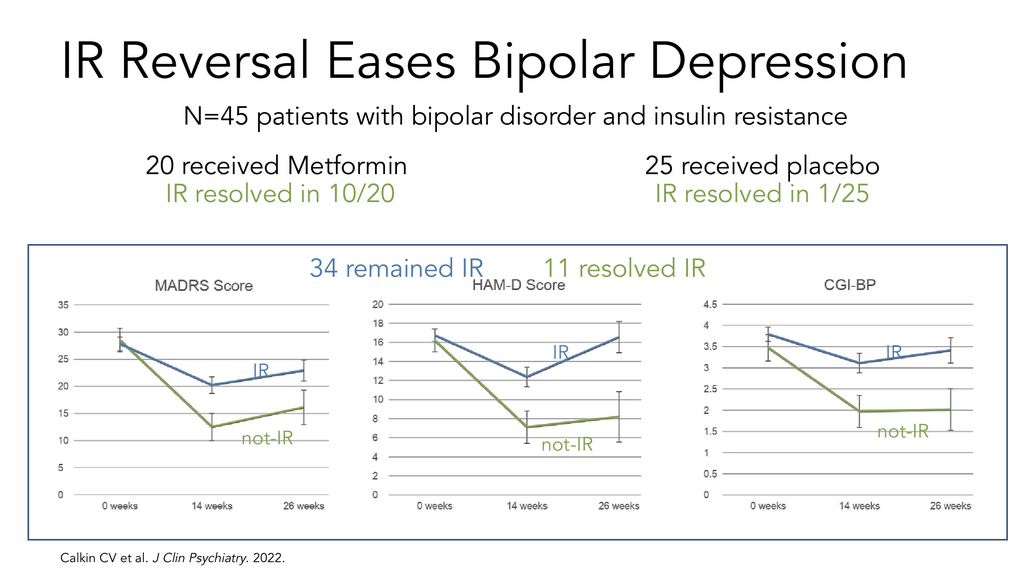
Georgia Ede, M.D. – Figure 32
She went one step further and supported this very well with a meticulously conducted, quadruple-masked, randomized controlled trial. She tested treating insulin resistance with medication to see what would happen to mood. Dr. Calkin used metformin, a common generic medication for type 2 diabetes, which works in part by improving insulin resistance. She found that the subjects with the greatest improvements in insulin resistance were the same patients who had substantial reductions in their depression symptoms. In subjects with no change in their insulin resistance, there was virtually no change in depression symptoms.
Georgia Ede, M.D. – Figure 33
90% Remission Free
I asked Dr. Calkin what it meant to her, to see such a striking result. She told me that almost 90% of the patients in her study had not had a single remission in 25 years.
“It has been a relief to discover a mechanism-based treatment that can get these patients better.”
Georgia Ede, M.D. – Figure 34
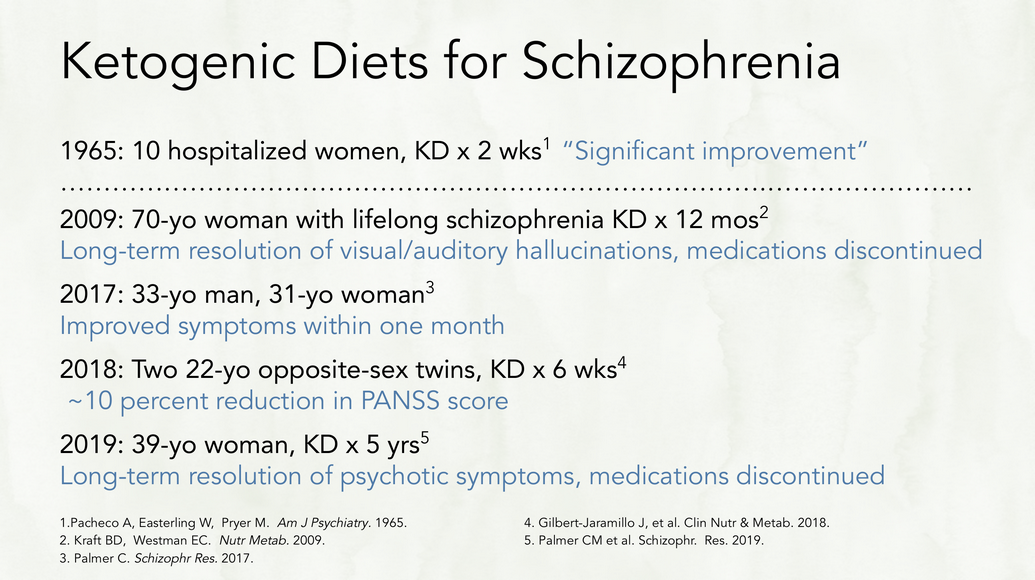
I want to briefly walk you through the scientific evidence for the use of ketogenic diets in various psychiatric conditions. There have been six case reports published in the literature, largely thanks to Dr. Chris Palmer, of patients with schizophrenia improving on a ketogenic diet. In two cases, patients achieved long standing resolution of symptoms with the ability to completely discontinue antipsychotic medications, which is just remarkable.
Georgia Ede, M.D. – Figure 43
[Dr. Albert Danan] invited 31 of his patients to try a ketogenic diet in the hospital under his supervision, completely voluntarily. We published the description of his clinical experience with these patients a couple of summers ago with Dr. Eric Westman and Dr. Laura Saslow.
Georgia Ede, M.D. – Figure 44
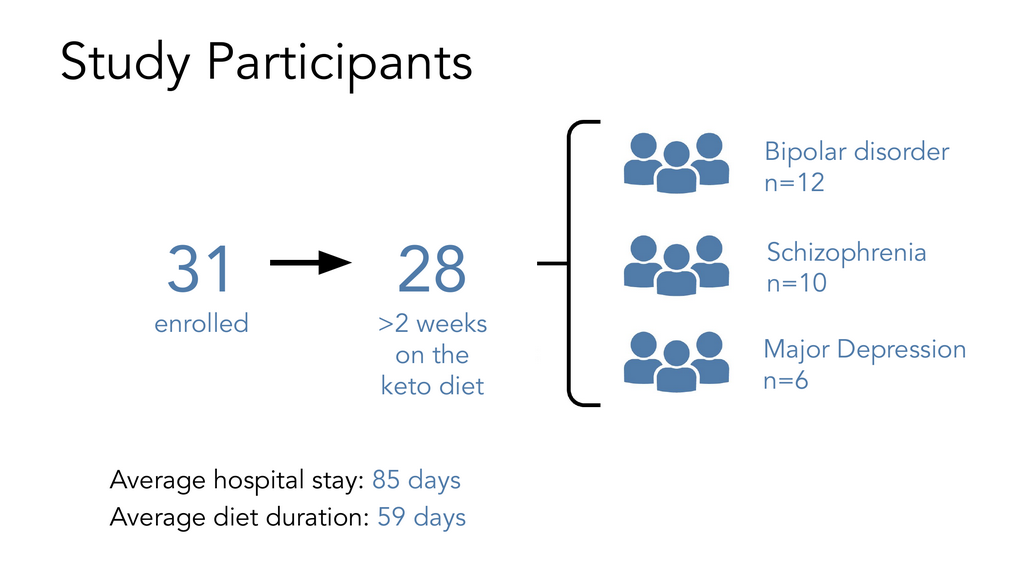
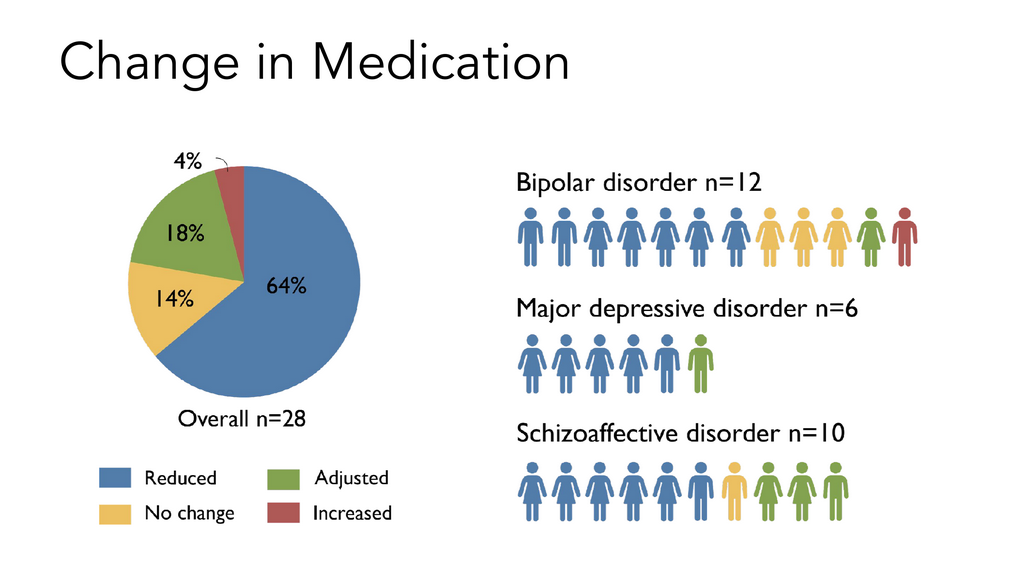
Of the 31 patients, 28 of them adhered to the diet long enough for us to analyze the results – at least two weeks. 12 patients had bipolar disorder, 10 patients had schizophrenia, and 6 had major depression.
Georgia Ede, M.D. – Figure 45
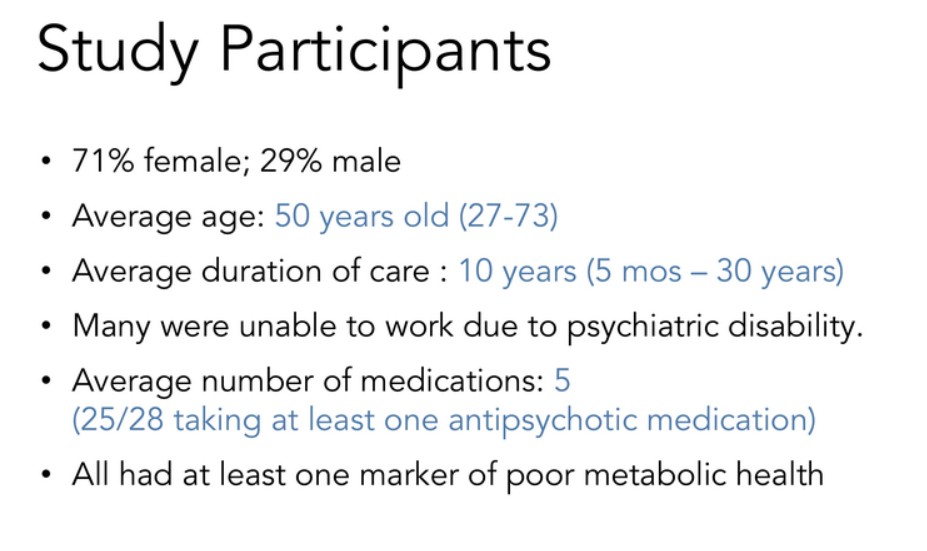
These were seriously ill, treatment-resistant patients on multiple medications. There were more females than males, with an age range from twenties to seventies, under his care for an average of 10 years but up to 30 years. He knew these patients very well, and many of them were psychiatrically disabled, on an average of five psychiatric medications. All of them had at least one marker of poor metabolic health.
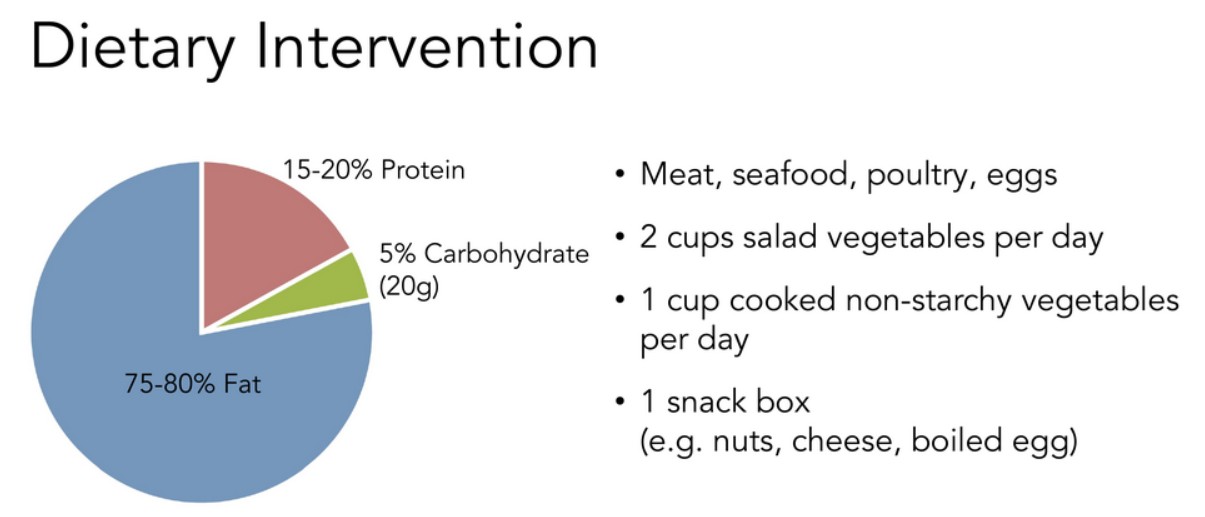
Georgia Ede, M.D. – Figure 46
This was the dietary intervention, a modified ketogenic diet based on whole foods, meat, seafood, poultry, eggs, some vegetables cooked and raw, and one keto-friendly snack per day. The diet was 75- 80% fat, 15 to 20% protein, and 5% carbohydrate – about 20 grams of carbohydrate per day.
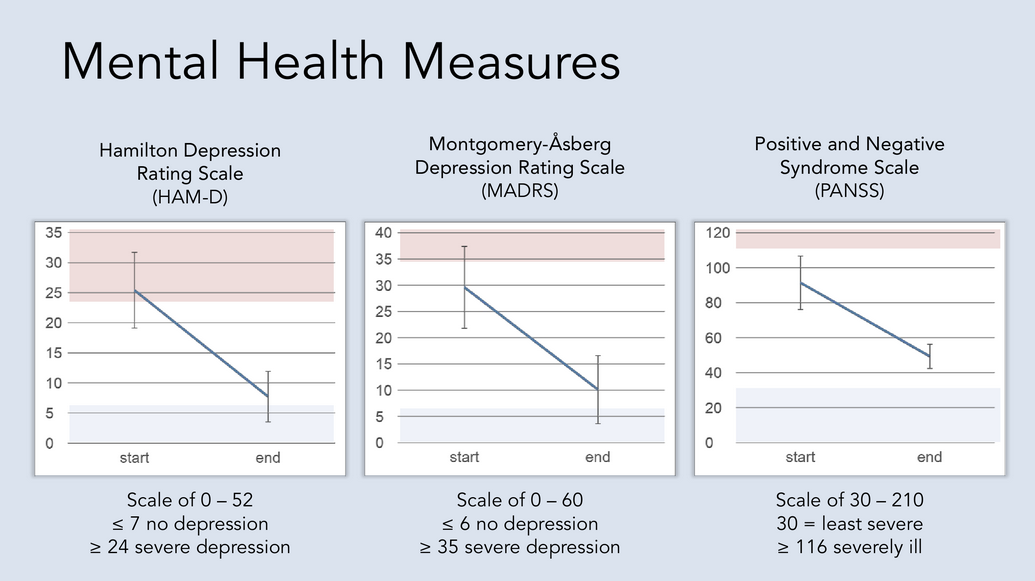
Georgia Ede, M.D. – Figure 47
Dr. Danan saw dramatic improvements in mental health measures across the board. Everyone improved – regardless of their duration of illness, regardless of the medications they were taking, regardless of their diagnosis.
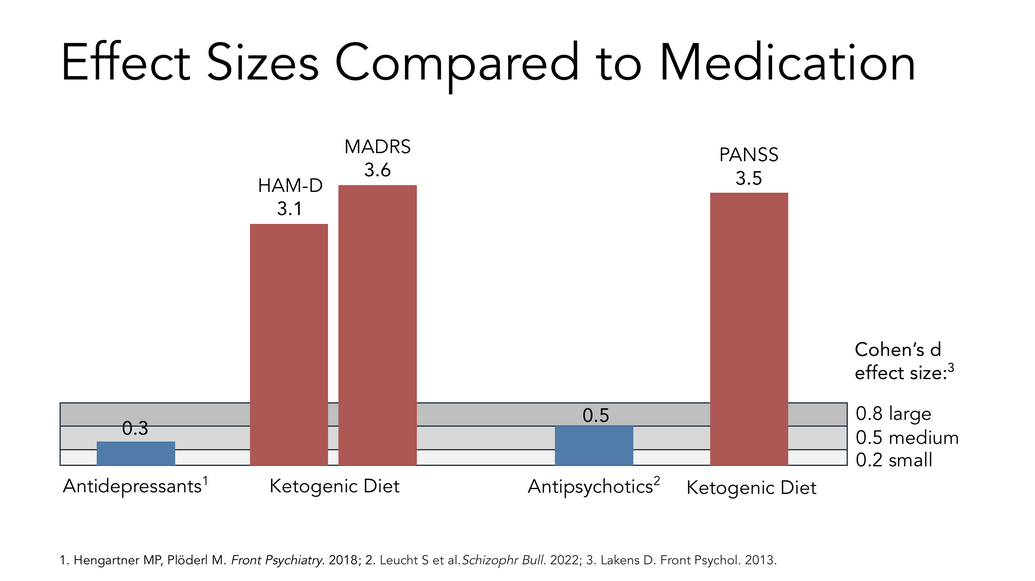
Georgia Ede, M.D. – Figure 48
To give you a sense of how dramatic these reductions were: In order for a pharmaceutical company to claim that their medication works, they have to describe something called the “effect size,” or “Cohen’s d effect size.” A typical antidepressant trial will show a Cohen’s d of about 0.3, which is considered a small effect. Antipsychotics fare a little better in randomized controlled trials, with a medium Cohen’s d effect of about 0.5. The ketogenic diet in Dr. Danan’s hands was 10x more effective, not a subtle difference.
References
1 Hengartner MP, Plöderl M. Front Psychiatry. 2018
2 Leucht S et al.Schizophr Bull. 2022
3 Lakens D. Front Psychol. 2013.
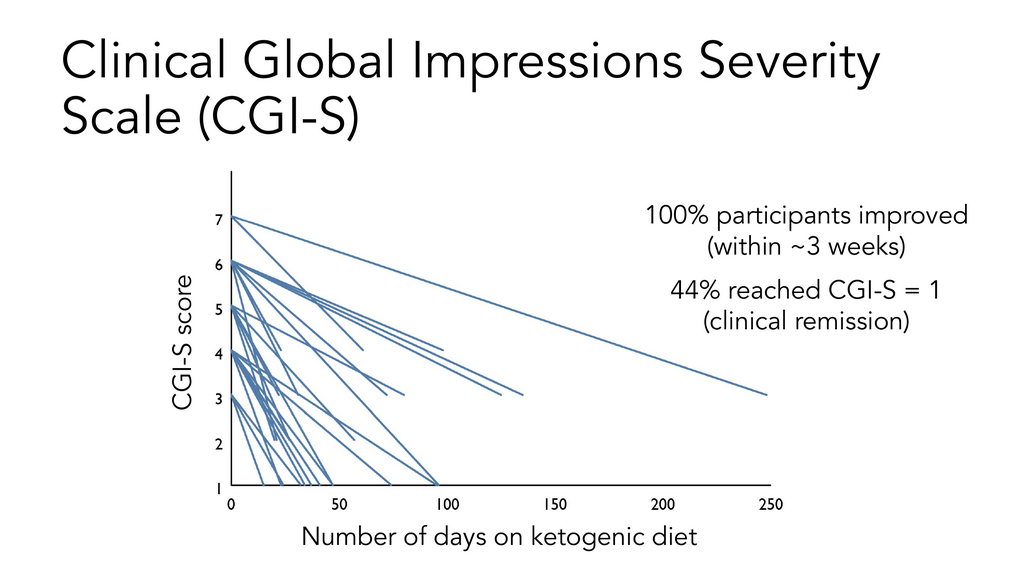
Georgia Ede, M.D. – Figure 49
100% of the patients improved within about three weeks, and 44% of them reached clinical remission. These were people with very severe chronic mental illnesses.
Georgia Ede, M.D. – Figure 50
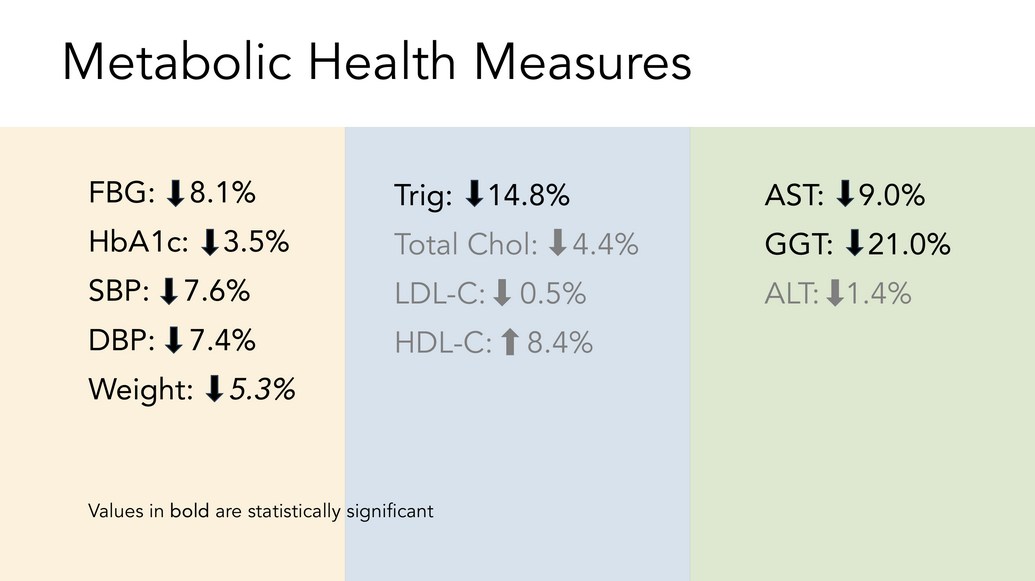
Ketogenic diets affect multiple markers of metabolic health. In our paper, the LDL didn’t change significantly, as is typical. Also typical, we saw dramatic drops in triglycerides. There was a nice lowering of serum glucose and significant weight loss, even though most of these patients were taking antipsychotic medications, which are notorious for causing stubborn and significant weight gain.
Georgia Ede, M.D. – Figure 51
64% of patients were able to leave the hospital on less medication. As any of you know who work in this field, you do not see that in conventional inpatient psychiatric care. It’s usually exactly the opposite.
Georgia Ede, M.D. – Figure 53
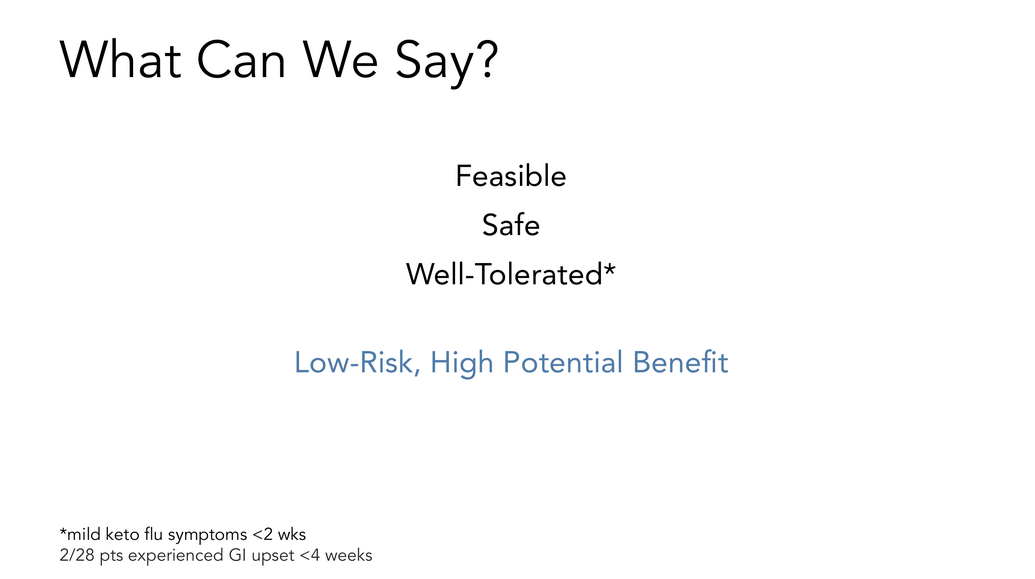
What we can say is it was feasible to administer this diet in a hospital setting. It was safe and well-tolerated. It’s a low-risk, high potential benefit intervention.
Georgia Ede, M.D. – Figure 54
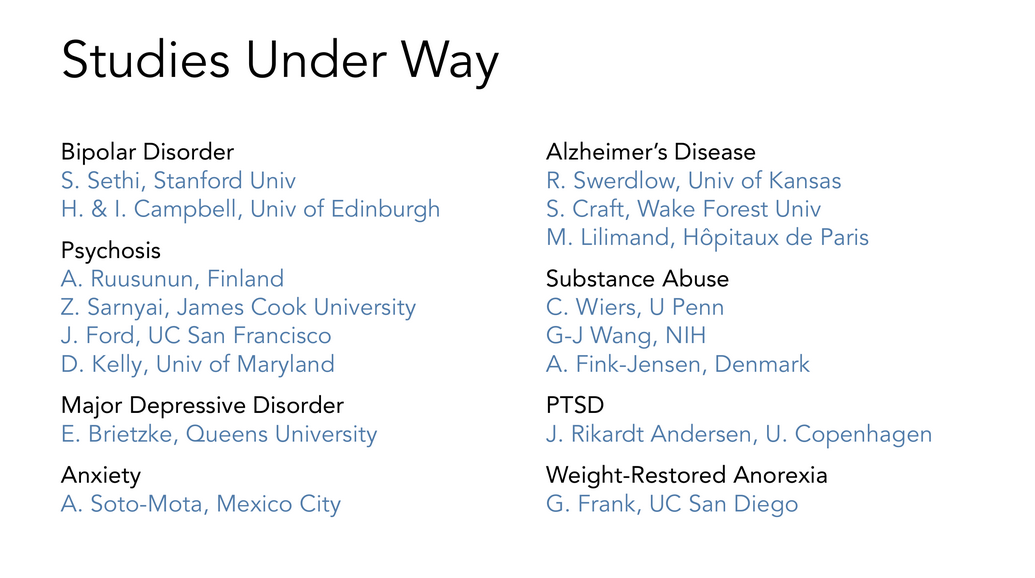
There are many more studies underway. This field is exploding, largely thanks to the Baszucki Group. So how does all of this information translate into everyday clinical care? We don’t have a lot of randomized controlled trials, which is the benchmark for many psychiatrists. They’re not going to use a new intervention unless there are randomized controlled trials. I think that bar is too high. Frankly, we have 100 years of evidence showing this is safe and effective in other brain conditions, and we’ve got very little to lose by trying it.
Georgia Ede, M.D. – Figure 55
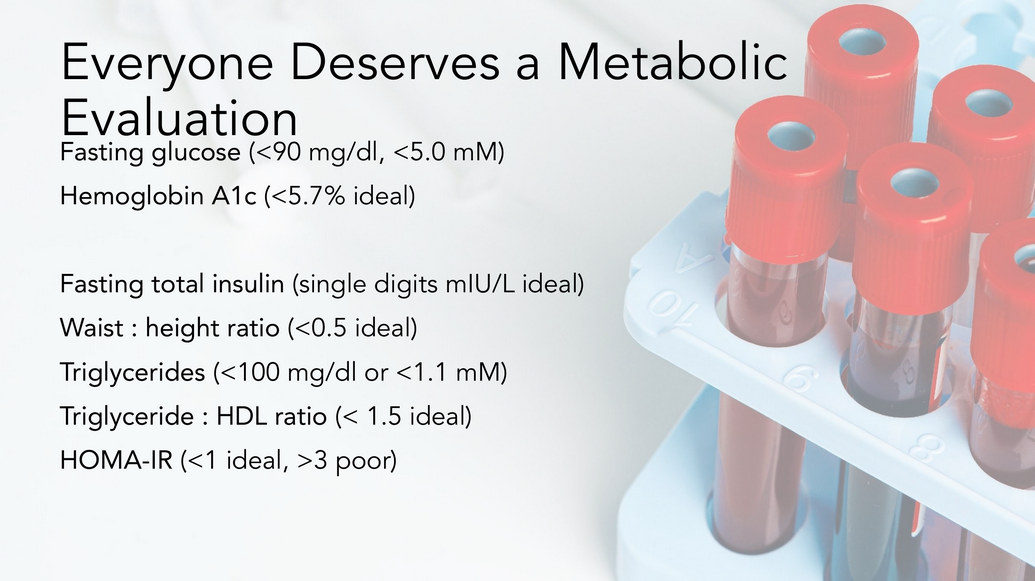
I think that everybody with a mental health condition deserves a metabolic evaluation. Look for and measure insulin resistance. Have a conversation with your patient about what this could mean for their mental health. Even if you do nothing else, recommend that they take the junk out of their diet – the refined carbohydrates. Not everybody needs a ketogenic diet, but at least teach them about some of the fundamental nutritional principles that they can use in their life to improve their health.
Google search result: How is insulin resistance diagnosed?
Google search result: HOMA-IR calculation
Georgia Ede, M.D. – Figure 56
If you’re going to use a ketogenic diet in clinical practice, there are some things you need to be aware of to use these diets safely. There are a few contraindications, including things like underweight, anorexia, pregnancy, and SGLT-2 inhibitors.* There are many blood glucose, blood pressure, and psychiatric medications that often need to be adjusted/weaned on a ketogenic diet, and this can be tricky. You also have to safely navigate the keto adaptation phase** in the first couple of weeks of the diet; a lot of this can be mitigated or avoided by easing into the diet slowly rather than starting it all at once.
*Google Search: SGLT2 Inhibitors are contraindicated with the ketogenic diet
Yes, the combination of SGLT2 inhibitors (like Jardiance, Farxiga, Invokana) and a ketogenic (very low-carb) diet is generally contraindicated or strongly discouraged due to significantly increased risk of a severe, potentially fatal condition called euglycemic diabetic ketoacidosis (euDKA), where the body produces excess ketones despite normal or near-normal blood sugar levels. Both the drugs and the diet independently increase ketones, creating a dangerous synergistic effect, so patients on SGLT2 inhibitors should avoid ketogenic diets and consult their doctor before starting any low-carb plan.
**Google Search: The keto adaptation phase of the ketogenic diet
Keto-adaptation is the metabolic shift where your body transitions from burning carbs to using fat and ketones for fuel, a process taking weeks to months, not days. It involves increased fat burning (fat oxidation), reduced glucose reliance, and improved cellular machinery for ketone use, leading to sustained energy, mental clarity, and reduced cravings, though initial “keto flu” symptoms like fatigue and brain fog (days 2-4) occur as your body adjusts.
The Stages & Timeline
- Days 1-7 (Keto Flu): Initial carb withdrawal causes headaches, fatigue, brain fog, irritability as your body adjusts.
- Weeks 2-4 (Early Adaptation): Symptoms lessen as ketone levels rise and your body starts using them more effectively.
- Months 1-3+ (Full Adaptation): Complete metabolic shift; you feel steady energy, reduced hunger, and better focus.
Georgia Ede, M.D. – Figure 57
There are many resources now for additional information. At the Baszucki Group’s metabolicmind.org, Dr. Brett Scher has some wonderful interviews with researchers, clinicians, families, and patients. There is a lot of free information there. It can be hard to find clinicians who offer these services; please help me grow the free directory on my website, diagnosis.com. It’s free to post your practice there so people can network and find practitioners who use ketogenic diets specifically to treat mental health conditions.
References
Georgia Ede, M.D. – Figure 58
I was thinking the other day about why I do this work. It’s not only that it’s joyful and empowering and that I see better results than with medication. It’s because I think we need to grow this movement and have more conferences like this. I’m really tired of people having to accidentally stumble their way into a ketogenic diet after trying 10 or 15 years of other treatments and dozens of medications. It’s really sad to hear people say they accidentally discovered it when they tried to lose weight or heard somebody else’s story. These need to be presented as options from day one by everyone who treats people with mental health conditions. Thank you very much for your attention.
______________________________________________________________
Managing Major Mental Illness with Dietary Change: The New Science of Hope, Georgia Ede, M.D.
Program Description
New clinical trial evidence suggests that dietary changes can be powerful tools in the treatment of psychiatric conditions – but which dietary changes are most worth making, and why? In the past decade, two relatively new subspecialties within the field of psychiatry have emerged: nutritional psychiatry, which focuses primarily on the therapeutic potential of the Mediterranean diet, and metabolic psychiatry, which focuses primarily on the therapeutic potential of the ketogenic diet. This discussion will examine the existing clinical evidence in support of both dietary philosophies, and then measure these (and other) nutrition interventions against newly proposed brain-healthy diet criteria. We will consider findings from a recently published paper out of France, in which 31 people with serious, chronic, treatment-refractory mental illnesses were placed on a whole-foods ketogenic diet in a supervised inpatient setting. We will then discuss how the improvements in metabolic and mental health observed in this study suggest that this approach is worth considering as an adjunctive strategy in the management of mental illnesses, particularly in those with poor metabolic health.
Educational Objectives
Upon completion of the educational activity, participants should be able to:
- Summarize the scientific basis for Metabolic Psychiatry.
- Identify at least three neurophysiological derangements common to major mental illnesses that can be addressed with a ketogenic diet.
- Explain where the clinical trial evidence currently stands with respect to ketogenic diets for psychiatric disorders.
- Summarize the key findings of the paper by Danan et al., in which 31 inpatients with treatment-refractory mental illness were placed on a ketogenic diet.
Accredited Provider
This activity is provided by Dane Garvin, Ltd.
AMA PRA Category 1 CreditsTM
Accreditation Statement
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of McLean Hospital and Dane Garvin Ltd. McLean Hospital is accredited by the ACCME to provide continuing medical education for physicians.
Physician Credit Designation Statement
McLean Hospital designates this enduring material for a maximum of 1.00 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Faculty
Georgia Ede, MD
Nutritional and Metabolic Psychiatry
Psychiatrist, Speaker, Clinical Educator, Researcher, Author
Amesbury, MassachusettsDr. Georgia Ede has no relevant financial information to disclose.
Instructions
In order to receive credit, participants must complete all of the course lessons. Participants must also score at least a 70% on each chapter quiz. Upon completion of lessons and quizzes, you must also complete the evaluation form. Your certificate will be available to download upon completion of the evaluation.
Your online certificate will be saved on Dane Garvin’s website and cannot be accessed in your myCME Dashboard or Transcript.
McLean Hospital Contact Information
For information about the accreditation of this program, please contact Marjorie Overhiser at 617-855-3151 or moverhiser@mgb.org.