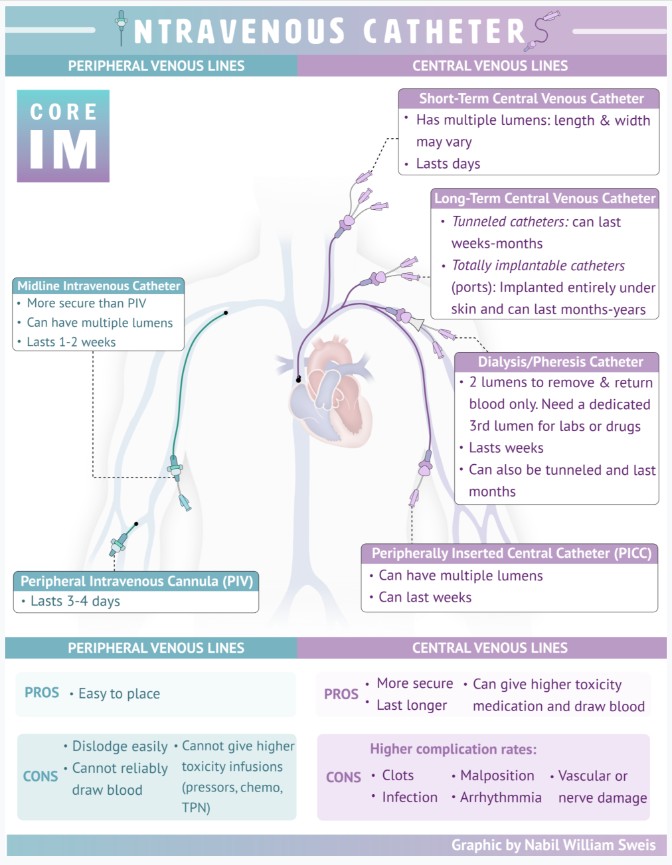
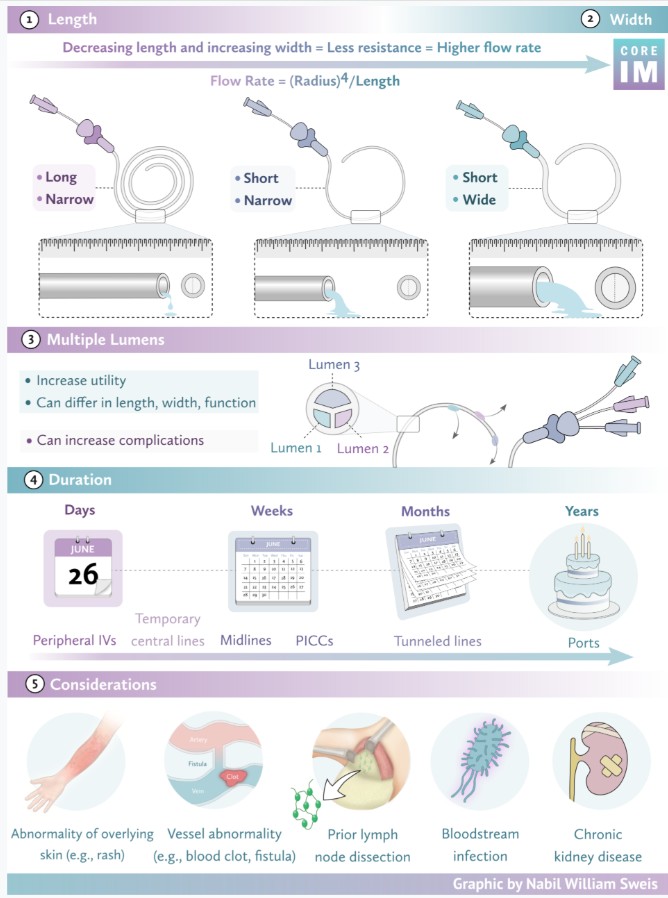
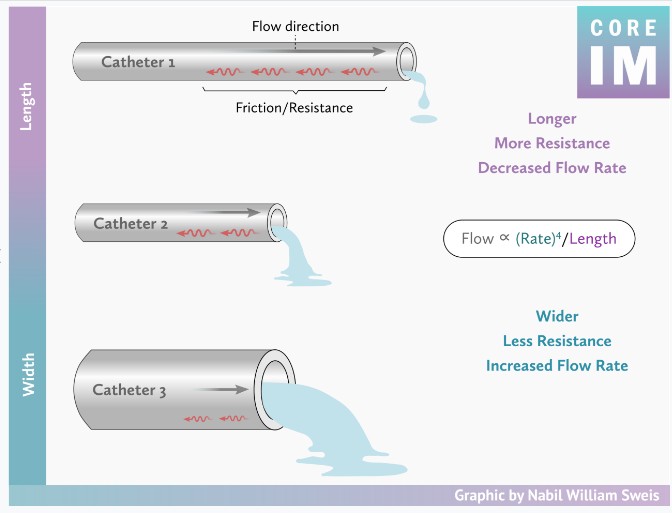
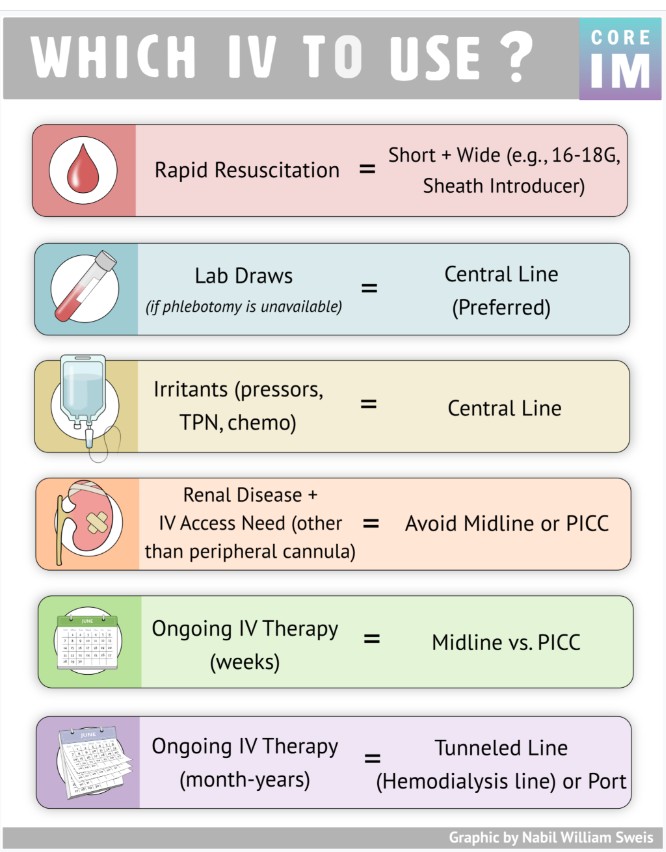
Today, I review, link to, and embed CORE IM‘s “Which IV should you use?”. Posted: February 4, 2026
By: Dr. Nick Villano
Graphic: Dr. Nabil Sweis
Audio: Dr. Marissa LoCastro
Be sure and review the outstanding Videos.
Be sure and review the outstanding Transcript.
All that follows is from the abovee resource.