In addition to the article reviewed in this post, please carefully review:
What is the most current version of CAD-RADS (Google Search):
CAD-RADS 2.0, published in 2022. This expert consensus document was a collaborative effort by major cardiology and radiology societies to standardize the reporting of coronary CT angiography (CCTA) findings and guide patient management.
CAD-RADS™ 2.0 – 2022 Coronary Artery Disease-Reporting and Data System-An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI) [Full-Text HTML] [Full-Text PDF]. Journal Of Cardiovascular Computed Tomography (JCCT), Volume 16, Issue 6p536-557November-December, 2022
Coronary Artery Disease-Reporting and Data System 2.0: Examples for the different Cad-Rads categories. Radiology Assistant, Publication Update 2023-05
The PREVENT Risk Score Equation (Google Search)
- Comprehensive Outcomes: Estimates risk for total CVD (ASCVD + Heart Failure), ASCVD (heart attack/stroke), and Heart Failure separately.
- Broader Age Range: Usable for adults 30-79 years, earlier than older tools.
- Race-Free Model: Removes race from the calculation, recognizing it as a social construct, notes this JACC article and this AHA article.
- CKM Integration: Combines heart, kidney (eGFR, UACR), and metabolic (HbA1c) health.
- Social Determinants of Health (SDOH): Optionally includes a zip code-based Social Deprivation Index (SDI) for deeper personalization, notes this AHA article.
- Large Data Source: Developed and validated using data from over 6.5 million US adults.
Cardiovascular disease risk estimates using the new PREVENT Equation: The good, bad, and the ugly [PubMed Abstract] [Full-Text HDML] [Full-Text PDF]. Am J Prev Cardiol. 2025 Sep 11:24:101288. doi: 10.1016/j.ajpc.2025.101288. eCollection 2025 Dec.The above article is very important and worth reviewing frequently.Predicting Risk of Cardiovascular Disease EVENTs (PREVENT) MD+Calc Accessesed 12-17-2025.It is critical to apply the risk calculator keeping in mind the points made in Cardiovascular disease risk estimates using the new PREVENT Equation: The good, bad, and the ugly above.
______________________________________________________________
The following are two articles on the technique of coronary CT angiography.
- Abbara S, Blanke P, Maroules CD, Cheezum M, Choi AD, Han BK, Marwan M, Naoum C, Norgaard BL, Rubinshtein R, et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: a report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr. 2016;10:435–449.
2. Shaw LJ, Blankstein R, Bax JJ, Ferencik M, Bittencourt MS, Min JK, Berman DS, Leipsic J, Villines TC, Dey D, et al. Society of Cardiovascular Computed Tomography/North American Society of Cardiovascular Imaging—expert consensus document on coronary CT imaging of atherosclerotic plaque. J Cardiovasc Comput Tomogr. 2021;15:93–109.
PubMed Abstract There are 101 similar articles in PubMed The above article has been cited by 99 articles in PubMed
In today’s post, I review, and excerpt from reference 2: Society of Cardiovascular Computed Tomography/North American Society of Cardiovascular Imaging—expert consensus document on coronary CT imaging of atherosclerotic plaque. J Cardiovasc Comput Tomogr. 2021;15:93–109. Link is to the PDF.
All that follows is from the above resource.
Abstract
Coronary computed tomographic angiography (CCTA) provides a wealth of clinically meaningful information beyond anatomic stenosis alone, including the presence or absence of nonobstructive atherosclerosis and high-risk plaque features as precursors for incident coronary events. There is, however, no
uniform agreement on how to identify and quantify these features or their use in evidence-based clinical
decision-making. This statement from the Society of Cardiovascular Computed Tomography and North
American Society of Cardiovascular Imaging addresses this gap and provides a comprehensive review of
the available evidence on imaging of coronary atherosclerosis. In this statement, we provide standardized definitions for high-risk plaque (HRP) features and distill the evidence on the effectiveness of risk stratification into usable practice points. This statement outlines how this information should be communicated to referring physicians and patients by identifying critical elements to include in a structured CCTA report – the presence and severity of atherosclerotic plaque (descriptive statements, CAD-RADS™ categories), the segment involvement score, HRP features (e.g., low attenuation plaque, positive remodeling), and the coronary artery calcium score (when performed). Rigorous documentation of atherosclerosis on CCTA provides a vital opportunity to make recommendations for preventive care and to initiate and guide an effective care strategy for at-risk patients.
© 2020 Published by Elsevier Inc. on behalf of Society of Cardiovascular Computed Tomography.The traditional approach to imaging of coronary anatomy with
coronary computed tomographic angiography (CCTA) has been
oriented toward the detection of obstructive coronary artery disease (CAD). Over the past decade, evidence has accumulated concerning the prognostic significance of nonobstructive and
obstructive atherosclerotic plaque including specific features that are associated with an elevated risk of major adverse CAD events (MACE). This evidence now supports that imaging of atherosclerotic plaque is important for estimating patient risk and guiding preventive care. This link between initiation and intensification of prevention with atherosclerotic imaging using CCTA is vital to improving patient outcome. In this statement from the Society of Cardiovascular CT (SCCT) and North American Society of Cardiovascular Imaging (NASCI), we provide a synthesis of evidence concerning CCTA imaging of atherosclerosis and propose data elements that radiologists and cardiologists can integrate into their CCTA interpretation. One vital part of this statement is to acknowledge the advantages and limitations of current methods used to assess atherosclerotic plaque and to identify future research in this area. In this SCCT/NASCI statement, we enlist thought leaders in the field of CCTA including experts from the field of radiology and cardiology who bring unparalleled experience to this subject of atherosclerotic imaging. This field is rapidly evolving and
further advancements, including fully automated quantification of atherosclerotic plaque will necessitate future updates to this
statement.This statement focuses on the following principal issues that will influence how we think about imaging coronary atherosclerotic plaque:
1. CT Imaging of Atherosclerotic Plaque: Risk prediction in stable and unstable chest pain syndromes
2. Evidence Gaps in Coronary Atherosclerotic Plaque Imaging and Future Research Needs
3. CT Plaque Imaging to Direct Risk-Reducing Preventive or Disease-Modifying Therapies: Observational evidence on CCTA guided preventive strategies
4. Minimum Data Elements for Structured Reporting For Coronary Atherosclerotic Plaque
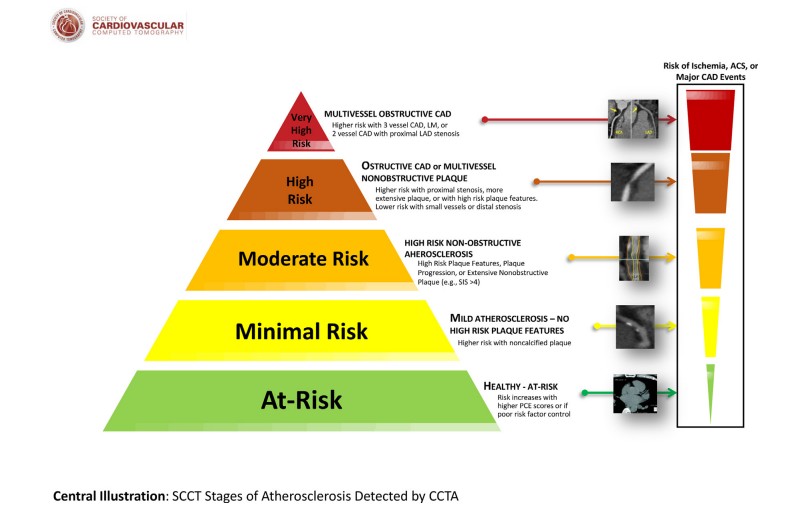
5. Consensus Summary and Recommendations1. Coronary atherosclerosis is the primary disease process
Imaging has traditionally focused on detecting flow limiting
stenosis or its surrogates. Detection of the presence and severity of
obstructive CAD by CCTA guide clinical decision making for secondary prevention including consideration of coronary revascularization. However, atherosclerosis is the primary disease process that mediates risk and stenosis is just one of its many subsets. Importantly, for risk assessment, patients with more extensive, multivessel CAD are at highest risk while those without any plaqueor stenosis comprise those at lowest risk (Central Illustration).This document focuses on the presence and extent of atherosclerotic plaque that elevates risk above that of patients
without any documented plaque. This ranking of disease presence and severity remains vital to providing a comprehensive assessment of patient risk.The evolving paradigm for CCTA imaging represented in this
document expands this viewpoint beyond detecting obstructive
lesions to imaging coronary vessel pathology itself: characterizing and providing measurement of the burden of atherosclerosis, identifying how its composition influences risk and outcomes, and potentially modifying risk with initiation or intensification of therapy. We propose that imaging of atherosclerotic plaque in order to target effective preventive care strategies reinforces the concept that early detection and intervention has the greatest potential for improved event-free life years for at-risk patients. However, current randomized trials are lacking and do not proscribe a detailed evaluation and treatment pathway. In this statement, we synthesize the observational evidence and patterns as they unfold about
the impact of treatment on atherosclerotic plaque.2. Targeting the appropriate patient population
This guideline will focus discussion on the use of imaging of
atherosclerosis with CCTA for symptomatic patients. Although evidence does exist with regards to the role of imaging in asymptomatic individuals, there are separate guidance documents from SCCT on the clinical indications for coronary artery calcium (CAC) scoring in asymptomatic patients1 and the CAC data and reporting system statement (CAC-DRS™).23. Methodologic considerations in atherosclerotic plaque imaging
This document will highlight evidence on both qualitative as
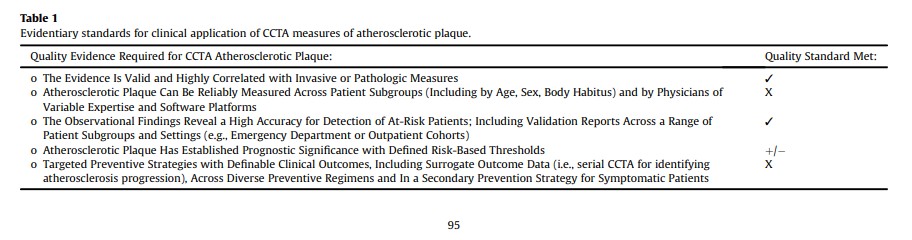
well as quantitative atherosclerotic plaque assessment. However, at present, in the absence of validated tools for quantitative assessment, we recommend integration only of semi-quantitative measures of atherosclerotic plaque into clinical reporting and propose data elements that radiologists and cardiologists can integrate into their CCTA interpretations today. While they remain incompletely defined at present, the field is evolving rapidly. The current quality standards for evidence are detailed in Table 1.
Provided limitations in spatial resolution and image quality,
plaque analysis should be restricted to epicardial vessels 2.0 mm in size and greater. Moreover, prior SCCT guidelines make recommendations for initial setting the window width and window levels (initial window width: 800 Hounsfield Unites [HU] and level: 300 HU) for accurate gray-scale differentiation between vessel wall and calcified and noncalified plaque.3,4 More recently, reports have applied varied approaches including: a) initial settings starting at a window width of 700 HU and window level of 200 HU; with subsequent changes determined by the imager,5 b) employing a fixed HU setting of 740/220, including a fixed 0.3 mm gap between vessel wall and lumen,6 and c) vessel wall thresholds adjusted to the lumen using a 155%/65% window width/level of the luminal intensity.5,7 Plaque analysis has been validated across recommended target heart rate (60e80 beats per minute) and standard tube voltage (100e120 kV).8 Whether or not to employ low kVp imaging is guided by the specific clinical question being evaluated as well as whether radiation saving techniques are desirable (e.g., young age). Lower tube voltage would impact HU ranges for plaque measurements.4. Importance of nonobstructive CAD and CAD event risk
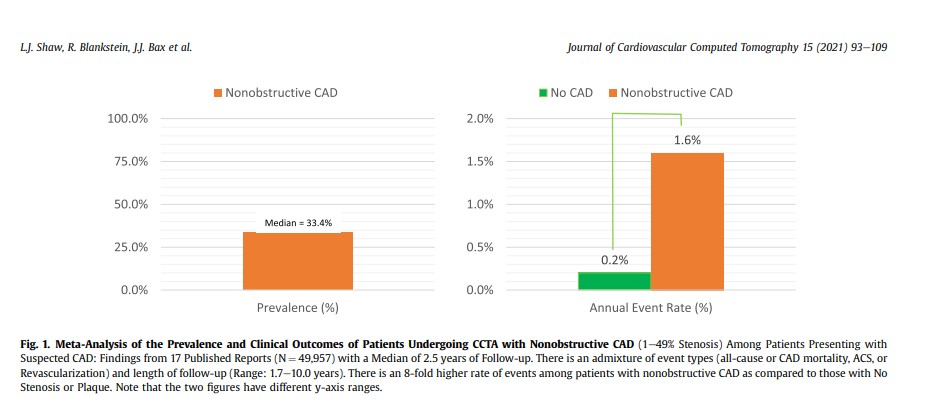
An emerging message from the published literature, over the
past decade, is that patients with nonobstructive CAD (i.e., 1-49% stenosis) have worse prognosis when compared to those without any stenosis or plaque (i.e., normal CCTA). Fig. 1 provides a synthesis of available evidence, noting that nearly 1 in 3 patients referred for CCTA for suspected CAD will have nonobstructive CAD.3,9e23 One-third of patients referred to CCTA have nonobstructive CAD while ~10-15% of patients have obstructive CAD.24 The annualized event rate for patients with nonobstructive CAD is ~1.6% as compared to 0.2% for those with a normal CCTA. The adjusted hazard for MACE for nonobstructive CAD as compared to a normal CCTA ranged from 1.5 to 7.2; when controlling for CAD risk factors or a risk score.3,9-23
Thus, a first step for all CT imagers to comprehend that identification of nonobstructive plaque is an important aspect of identifying at-risk patients. One commonly reported measure is the semiquantitative assessment of the number of coronary segments with plaque, independent of the stenosis severity, using the segment involvement score (SIS).25 The SIS provides an assessment of the extent of atherosclerosis and has higher reproducibility than descriptive terms. An SIS score >5 has been associated with an elevated event risk (p < 0.0001).26
______________________________________________________
What is the most current version of CAD-RADS (Google Search):
CAD-RADS 2.0, published in 2022. This expert consensus document was a collaborative effort by major cardiology and radiology societies to standardize the reporting of coronary CT angiography (CCTA) findings and guide patient management.
CAD-RADS™ 2.0 – 2022 Coronary Artery Disease-Reporting and Data System-An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI) [Full-Text HTML] [Full-Text PDF]. Journal Of Cardiovascular Computed Tomography (JCCT), Volume 16, Issue 6p536-557November-December, 2022
Coronary Artery Disease-Reporting and Data System 2.0: Examples for the different Cad-Rads categories. Radiology Assistant, Publication Update 2023-05
The PREVENT Risk Score Equation (Google Search)
- Comprehensive Outcomes: Estimates risk for total CVD (ASCVD + Heart Failure), ASCVD (heart attack/stroke), and Heart Failure separately.
- Broader Age Range: Usable for adults 30-79 years, earlier than older tools.
- Race-Free Model: Removes race from the calculation, recognizing it as a social construct, notes this JACC article and this AHA article.
- CKM Integration: Combines heart, kidney (eGFR, UACR), and metabolic (HbA1c) health.
- Social Determinants of Health (SDOH): Optionally includes a zip code-based Social Deprivation Index (SDI) for deeper personalization, notes this AHA article.
- Large Data Source: Developed and validated using data from over 6.5 million US adults.
Cardiovascular disease risk estimates using the new PREVENT Equation: The good, bad, and the ugly [PubMed Abstract] [Full-Text HDML] [Full-Text PDF]. Am J Prev Cardiol. 2025 Sep 11:24:101288. doi: 10.1016/j.ajpc.2025.101288. eCollection 2025 Dec.The above article is very important and worth reviewing frequently.Predicting Risk of Cardiovascular Disease EVENTs (PREVENT) MD+Calc Accessesed 12-17-2025.It is critical to apply the risk calculator keeping in mind the points made in Cardiovascular disease risk estimates using the new PREVENT Equation: The good, bad, and the ugly above.
Resuming article Society of Cardiovascular Computed Tomography/North American Society of Cardiovascular Imaging—expert consensus document on coronary CT imaging of atherosclerotic plaque.5. High risk plaque (HRP) features on CCTA
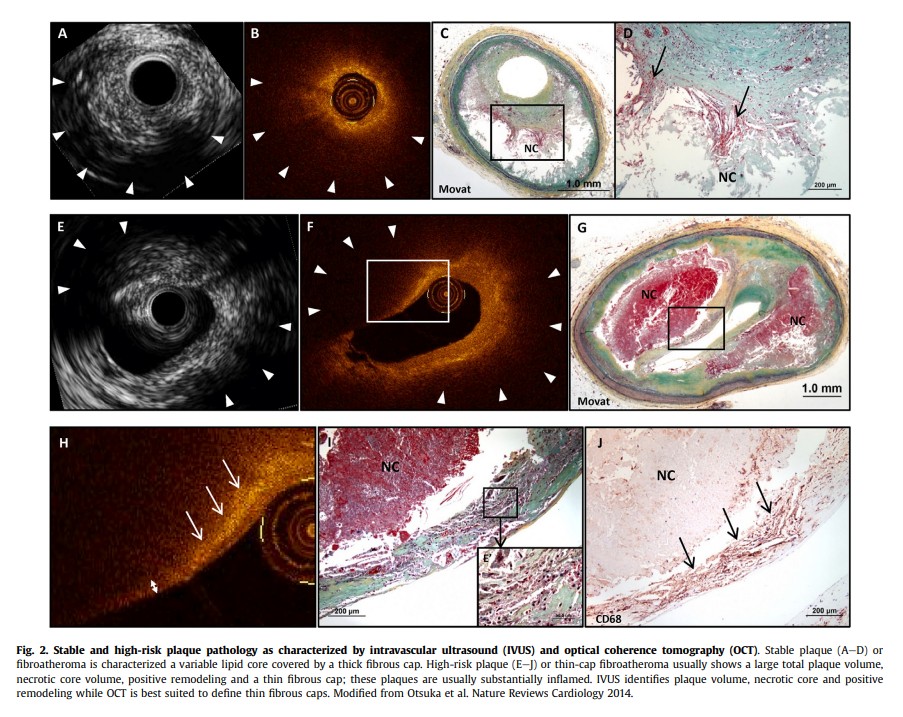
Histological assessment of coronary atherosclerosis has identified plaque features found in culprit lesions of patients who succumbed to sudden cardiac death, in particular, thin cap
fibroatheroma (TCFA).27e30 Beyond the thin cap, other features
comprising the TCFA are large plaque volume and necrotic core.
Some of these features have been identified using invasive imaging methods, including intravascular ultrasound (IVUS),31 optical coherence tomography (OCT)32 and near-infrared spectroscopy in patients with acute coronary syndromes. Each of these methods has its own limitations in providing a comprehensive picture of the vessel wall, extent of atheroma burden across the entire tree and stenosis.33 Fig. 2 depicts examples of stable and high-risk plaque pathology as characterized by IVUS and OCT.With the exception of the thin cap, these features of TCFA (i.e.,
the presence of a large lipid core, positive remodeling [PR], and
large plaque burden) can also be identified with CCTA with the
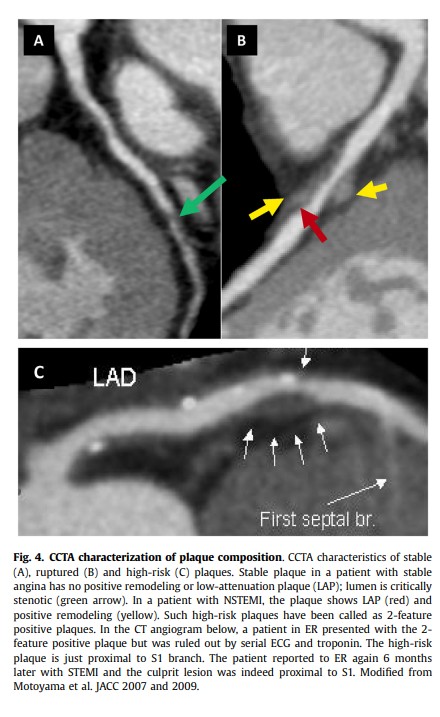
advantage that it is noninvasive. CCTA can characterize and identify abnormalities in the coronary artery wall itself across the entire coronary tree, rather than just the presence of luminal stenosis. This includes the identification of both calcified and noncalcified plaque,34 and further classification of plaque size and specific HRP features. These HRP features found on CCTA correlate with histological and invasive assessment of plaque vulnerability, and are more frequent in patients with an acute coronary syndrome (ACS) at the time of CCTA or for those who subsequently develop ACS or other major adverse CAD events (MACE) after CCTA. Fig. 3 details the hierarchical importance of morphological characteristics of plaque vulnerability.5.1. HU density and plaque compositionThe composition of atherosclerotic plaque is categorized using
HU density with lower to higher values correlating to necrotic core, fibro-fatty, fibrous, and calcified plaque by IVUS and histopathology.35 Several interpretive platforms are available that employ slightly different HU density ranges for categorization.5,35,36 The composition of plaque is categorized as follows: a) dense calcium for HU densities >350’ b) fibrous plaque for a range of values from
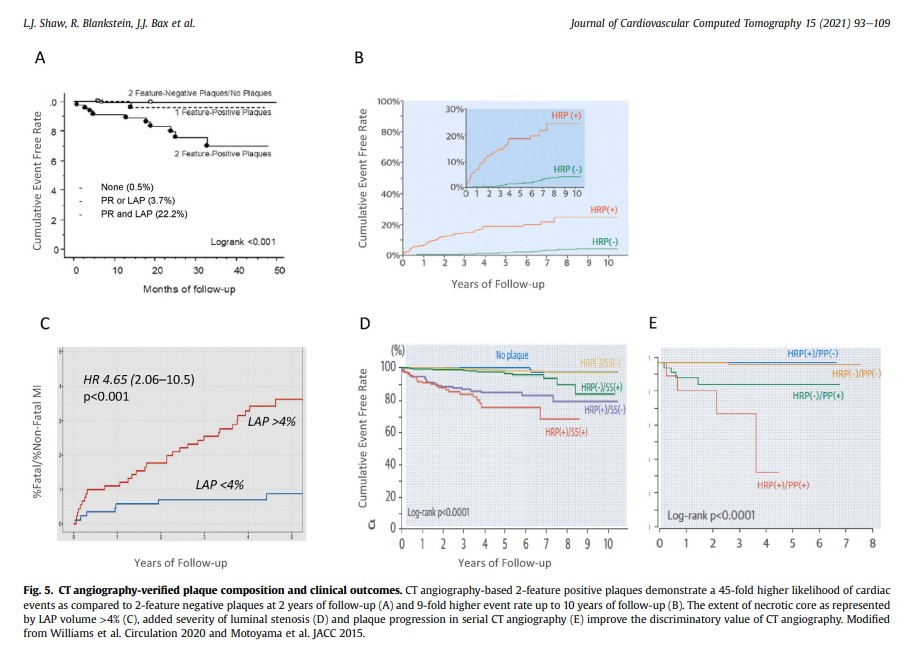
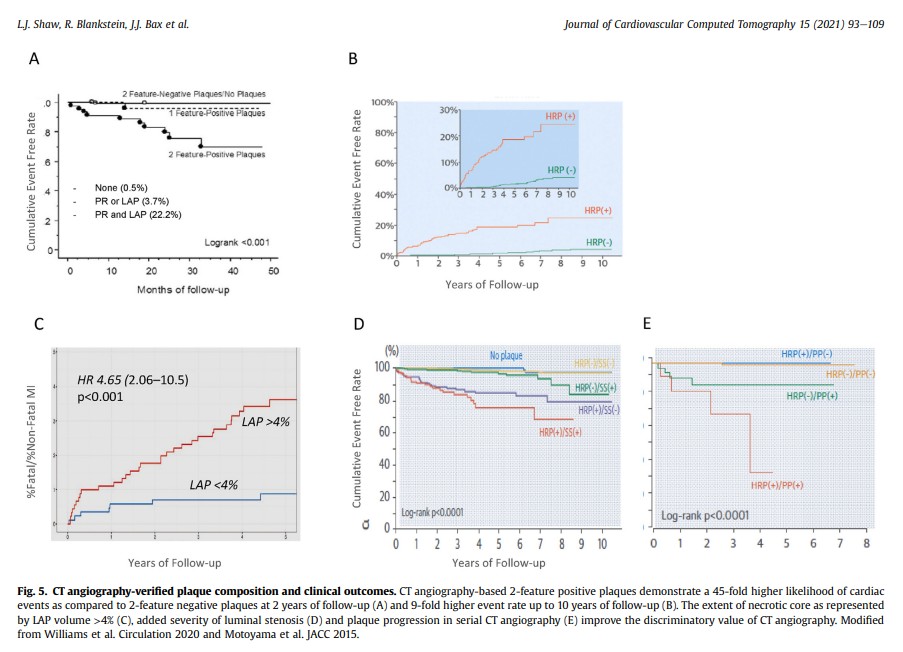
131 to 350 HU; c) fibro-fatty plaque for a range of values from 31 to 130 HU; and necrotic core for a range of values from 30 to 30 HU.36,37 Fig. 4 provides an example of CCTA characterization of plaque composition.Importantly, HU densities on CT overlap across
compositional subgroups on IVUS.8 Normalization of the luminal contrast attenuation (plaque/lumen HU ratio) or adaptive thresholds can improve categorization of lipid-rich versus fibrous plaque.8 Most of the software programs have been correlated with IVUS measurements, but data is not available directly comparing the accuracy of the varied programs. As such, CT imagers should realize that variations in plaque measurements may result from different programs. Fig. 5 includes the results from several published reports detailing CCTA-verified plaque composition and clinical outcomes.38,395.2. HRP and culprit ACS lesionsSeveral CCTA characteristics associated with these histological
and invasive features of plaque vulnerability40 were confirmed as plaque features associated with culprit ACS lesions.27,31e33,40,41 The presence of HRP [High Risk Plaque] features on CCTA are common in culprit lesions of ACS.27,31,33,40e43 The major plaque characteristics included in HRP definitions are low attenuation plaque (LAP), and positive remodeling (PR) and have conveniently been termed as 2-feature positive plaques.38,44,45 PR is the presence of an outer vessel diameter which is 10% greater than the mean of the diameter of the normal adjoining segments, also labelled as the remodeling index (RI) > 1.1.34,46 Measurement of an RI > 1.1 can be challenging in smaller diameter vessels where limitations in spatial resolution may impair detection. LAP is conventionally defined as the presence of a central focal area within the plaque which has a low CT attenuation which is usually defined as at least 1 voxel with <30 HU47,48; although other thresholds (e.g., <60 HU and <90HU) have also been used.49e51 This definition based on a single voxel
threshold can be impacted by image noise. Other less studied features include the napkin-ring sign (NRS) which suggests the presence of circumferential necrotic core33,41,52 and spotty calcification (SC) as compared to more dense and plate-like calcification.53 The NRS is described as a central area of low CT attenuation that abuts the lumen and a ring like higher attenuation plaque tissue surrounds this low attenuation area.27,33,40,54e56 A NRS is associated with advanced atherosclerotic lesions by histology, including a large lipid core or thrombus. Several definitions of SC are used in the literature, the most commonly applied is the presence of small focal calcifications <3 mm diameter in any direction. Another definition includes calcium length (in the longitudinal direction of the vessel) < 1.5 times the vessel diameter and width (calcification extent perpendicular to the longitudinal direction of the vessel) < 2/3 of the vessel diameter.32,57,58 These HRP features are easy to identify when combined with simple manual measurement (e.g., distance, region of interest) on standard workstations.In a secondary analysis from the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) II trial, the presence of HRP was associated with an increased risk of ACS during the index hospitalization; independent of stenosis severity.59 A metaanalysis of 18 smaller studies confirm the association between HRP features and the culprit ACS lesion.60The CAD-RADS™ classification defines HRP as the presence of a
minimum of two of the four HRP features in the same coronary
plaque.61 Although ACS risk increases when two or more HRP
features are present, any of the four measures correlate with event risk. However, some studies have not included SC in the definition of HRP50,51,62 and others have suggested that the presence of SC was not associated with an elevated risk when compared to high risk, LAP and the NRS.636. Prognostic value of HRP in patients with stable chest painHRP is a frequent finding on CCTA, occurring in 15e34% of patients with stable chest pain.64,65 Studies of symptomatic patients followed after CCTA have shown that the presence of HRP was associated with an increased risk of subsequent MACE. In a large study of 1,059 patients followed for a mean of 27 months, the presence of both PR and LAP was associated with ~22-fold increase in ACS risk.45 In a larger study of 3,158 patients followed for ~4 years, Motoyama et al. reported that the presence of HRP (i.e., PR and LAP) was associated with 8-fold increase of subsequent ACS.38 Several other studies54,55,57,58,66 as well as a metaanalysis54,55,57,58,66 found similar results from a large number of patients undergoing CCTA for stable chest pain.Recently, investigators in the PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) trial performed an assessment of HRP (defined as the presence of PR, LAP, or the NRS) in patients randomized to CCTA.64 The presence of HRP was associated with a ~70% increased risk of MACE (death, myocardial infarction [MI], or hospitalization for unstable angina) at ~2 years of follow-up. The predictive value of HRP was strongest in younger patients, women, and in those with nonobstructive CAD.In the SCOT-HEART (Scottish Computed Tomography of the
HEART) trial, the presence of HRP (defined as the presence of PR and/or LAP) was associated with an increased risk of coronary heart disease (CHD) death or MI at 5 years.65 Interestingly, HRP did not retain independent prognostic value when the CAC score was included as a covariate. The lack of improvement in risk prediction by HRP is likely the result of the CAC score as a measure of overall coronary plaque burden, while the HRP assesses the specific features of individual plaques. This secondary analysis reveals an important consideration that HRP are but one of many risk markers
and that the overall plaque burden, as measured by CAC, provide additional information to guide risk stratification.Challenges with prognostication using HRP including a high
prevalence (e.g., in the PROMISE trial, HRP identified in 40% of
patients with nonobstructive plaque and 75% of patients with
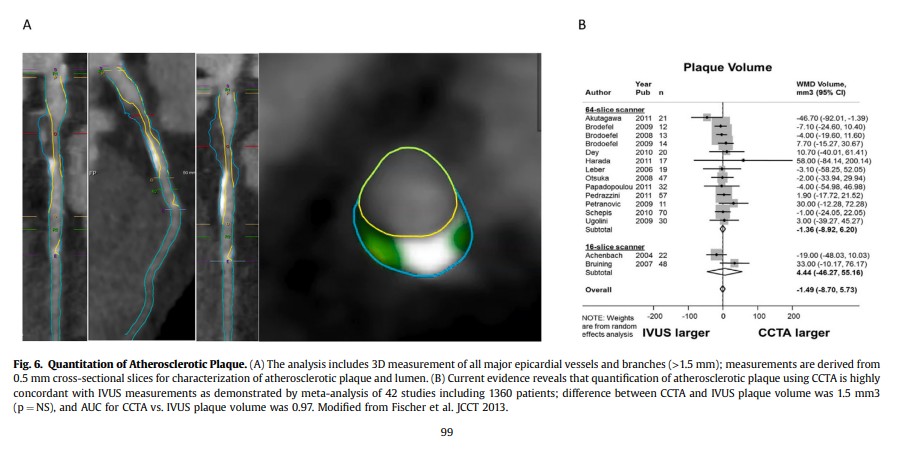
obstructive CAD) and a reduced positive predictive value; similar to invasive testing for identification of HRP. In part, the overall low risk observed in most studies is plausible given that plaque characteristics are dynamic and can change over time, particularly following initiation or intensification of medical therapies.65 It appears that the presence of HRP may best predict near as compared to longterm risk.657. Quantitative measurement of atherosclerotic plaqueTechnological developments in CCTA now allow semiautomated/automated software solutions for quantitative assessment of atherosclerotic plaque characteristics.57e60,62,63,67e87
Currently available semi-automated plaque assessment is time consuming, and fully automated quantification of atherosclerotic plaque based largely on artificial intelligence methods for image segmentation may be available in the near future for investigational purposes. Fig. 6 illustrates an example of the quantitative measurement of atherosclerotic plaque, along with a Forrest plot of the results of studies correlating CCTA and IVUS measurements of plaque volume.747.1. Quantitative plaque assessment and prognostic value for major CAD eventsSeveral studies have shown the feasibility of quantitative
assessment of plaque and established plaque volume as a predictor of future CAD events.72,88e90 In acute chest pain populations matched case and control pairs) to evaluate quantitative CCTA precursors of ACS. In ICONIC, both HRP features and quantitative assessment of fibrofatty and necrotic core plaque volume was more often associated with incident ACS; independent of coronary stenosis.36 HRP and quantitative LAP and SC were also predictors of future ACS culprit lesions in a population of patients with diabetes mellitus.93 Feuchtner et al. observed that LAP (<60 HU) and the NRS were the strongest predictors of MACE in a follow-up study of 1,469 patients.63 Similarly, Nadjiri et al. observed similar results, while
LAP, NRS, and total plaque volume were all predictive of MACE; LAP had prognostic information beyond traditional assessment of coronary stenosis.77From the SCOT-HEART trial, quantitative analysis revealed that low-attenuation plaque burden (% plaque to vessel volume) was the single greatest predictor of incident MI.39 Moreover, the presence of low attenuation plaque burden >4% was associated with a nearly 5- fold increase in the hazard for MI (Fig. 5). Among patients with nonobstructive CAD, a low attenuation plaque burden >4% was significantly predictive of incident MI but no increase in risk was noted for those with nonobstructive CAD and a low attenuation plaque burden <4% (p ¼ 0.81).7.2. Summary statement on risk assessment with CCTA findings of HRP
1. HRP characteristics are associated with ACS and future MACE: These lesions with HRP may be viewed as precursors to ACS, with the CCTA findings consistent with the invasive literature.
2. Reproducibility and Interobserver agreement for measurement of HRP requires additional investigation and improvement. Interobserver agreement for HRP remains moderate, with kappa values from 0.56 to 0.69 in research studies.94,95 This is suboptimal at present when compared to the detection of a high grade stenosis or the presence of any atherosclerotic plaque (yes/no) or characterization as calcified, noncalcified, and partially calcified.
3. There are differences in inter-observer variability in the visual identification of individual HRP features, with PR [Positive Remodelling] having the best overall agreement.8
4. Automated quantification of atherosclerotic plaque is available but, at this time, is investigational.
5. Importantly, although we can risk stratify with HRP, directed
interventions are not yet defined. Moreover, additional data are
required as the positive predictive value for HRP is variable when compared to comprehensive plaque burden measures,
such as CAC.
6. HRP is a dynamic process and likely to change over time- newer HRP may appear or the existing HRP could heal in response to lipid-lowering therapy without reaching a clinical threshold of disruption. Thus, routine use in clinical practice, especially in the presence of easy to quantify technology in future, will have to await robust clinical outcome data.8. Minimum Data Elements for structured reporting of
coronary atherosclerotic plaque[See CAD-RADS™ 2.0 – 2022 Coronary Artery Disease-Reporting and Data System-An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI) [Full-Text HTML] [Full-Text PDF]. Journal Of Cardiovascular Computed Tomography (JCCT), Volume 16, Issue 6p536-557November-December, 2022]