In this post, I link to and excerpt from The Curbsiders‘ excellent episode, #387: Diabetes Updates with Dr. Marie McDonnell: New Tools for the New Rules.*
March 27, 2023 | By Isabel Valdez.
*Watto MF, Valdez I, McDonnell ME, Williams PN. “387: Diabetes Update: New Tools for the New Rules”. The Curbsiders Internal Medicine Podcast. https://thecurbsiders.com/category/curbsiders-podcast March 27, 2023.
All that follows is from the above resource.
Links
- American Diabetes Association Standards of Care in Diabetes—2023
- American Association of Clinical Endocrinology Practice Guidelines -2022
- National Diabetes Prevention Program
Diabetes Updates: New Tools for the New Rules Pearls
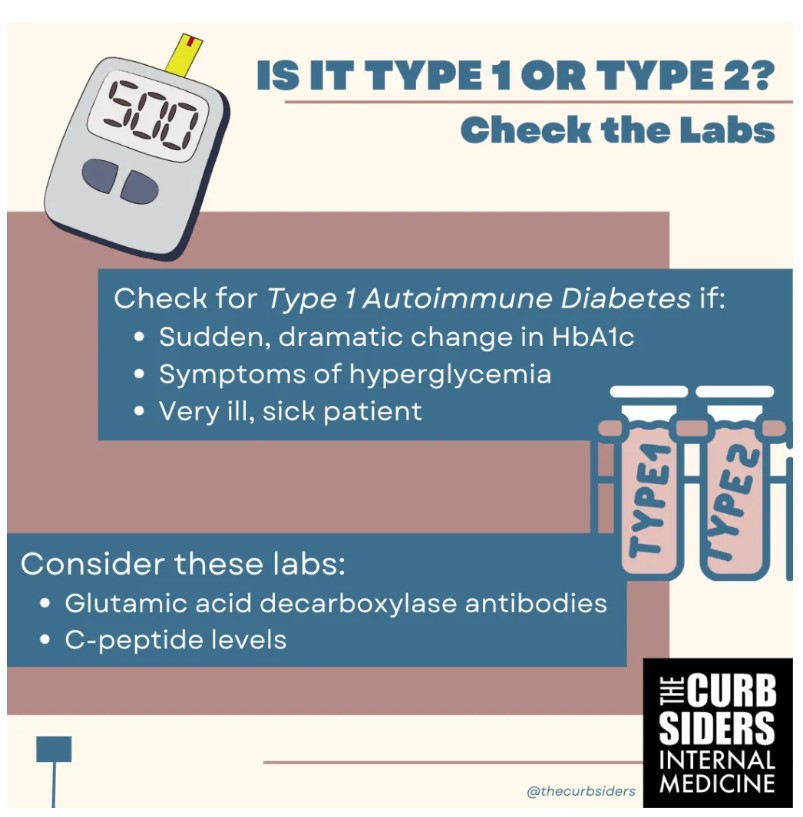
- Check what you are treating; easily distinguish between insulin deficiency and type 2 diabetes with labs before you start treatment.
- Updated guidelines focus not only on glucose control but also on helping patients with weight loss.
- Blood glucose control should be achieved with the least risk of hypoglycemia
- Semaglutide has been found to decrease stroke risk
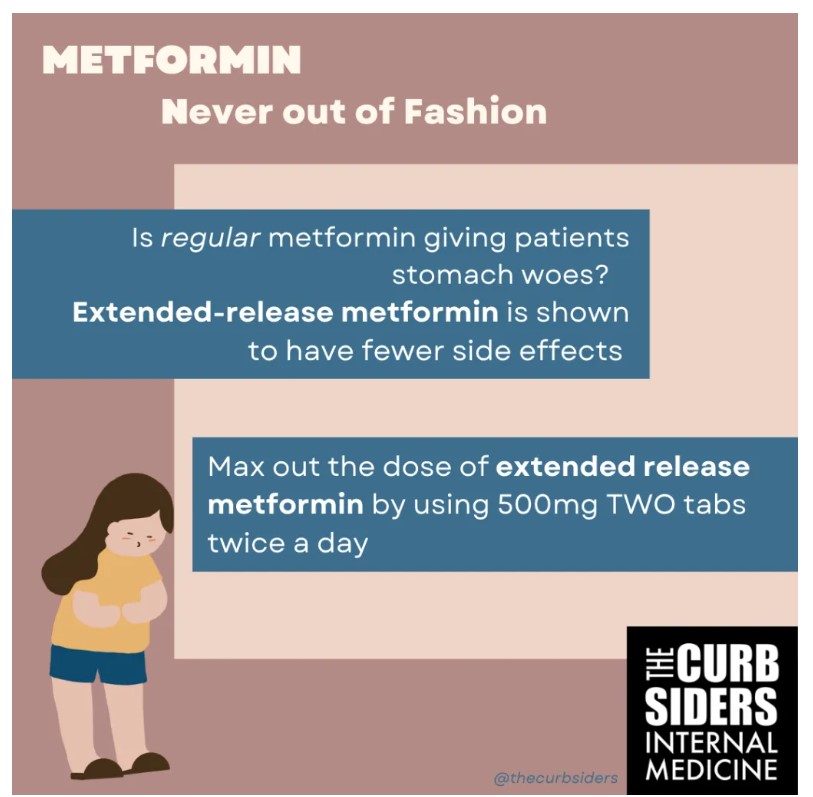
- Extended release metformin may be better tolerated and the highest tolerated dose should be split twice a day
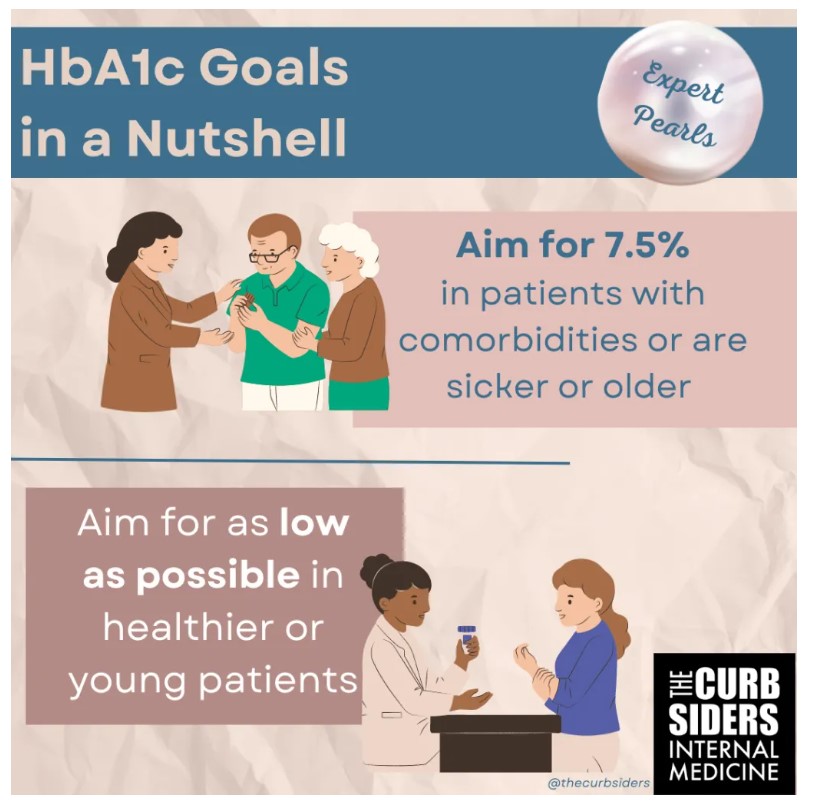
- Aim to attain the lowest A1c goal in younger healthier patients.
- Older, sicker patients or those with limited life expectancy should aim for an A1c goal of 7.5%
- To reduce the risk of yeast infections with SGLT2-i, try starting this drug when the A1c is less than 9%
- Pancreatitis incidence is low with GLP-1 but be aware of increased risk of thyroid cancer
- The GIP component in tirzepatide appears to enhance the effect of GLP-1 RA which could explain why this drug has less GI intolerance
Diabetes Updates: New Tools for the New Rules
Which is it? Distinguishing between Type 1 or Type 2 Diabetes
Type 1 diabetes, or otherwise called autoimmune diabetes progresses rapidly into insulin deficiency. Dr. McDonnell states there is a high incidence of type 1 diabetes in people over the age of 18 years (Thomas et al 2019). In a person who demonstrates a dramatic change in A1c, particularly at a young age, investigate further to determine if the patient has autoimmune diabetes. Glutamic acid decarboxylase antibodies, also known as GAD-65 is the most common islet cell antibody and should be checked to determine if the patient has autoimmune diabetes (Törn et al 2000). Checking a C-peptide level and a glucose level could also be checked initially but may be tested later if the patient is not responding to treatment (Lynam et al 2019). Dr. McDonnell reminds us to ask the patient about recent diet changes such as, drinking more juices, sodas or milk, or if they have received steroid injections because these could account for a dramatic rise in the A1c.
A New Focus: Weight Loss and Glucose Control
Weight Loss
GLP-1 RA are similar in potency to insulin and can give patients the added benefits of weight loss (Porcellati et al, 2015). New guidelines support starting the patient on a GLP-1 RA if they have obesity with lifestyle changes; metformin can still be used in this setting (El Sayed et al, 2022). Our expert would recommend starting a patient on a GLP-1 RA over metformin if they are very ill or sick from the hyperglycemia.
Glucose Control
A subset of patients are very sensitive to glucose exposure over time and develop neuropathy (Rajabally 2011; Kirthi et al 2021). In this population, she reminds us to evaluate for B12 deficiency or alcohol use disorder as potential sources of neuropathy as well.
Cardiovascular Risk Reduction
Newer guidelines emphasize the importance of cardiovascular risk in patients with diabetes. Older GLP-1 RA that were modeled from the saliva of the Gila monster were not found to have the cardiovascular benefits of the newer agents in this family of drugs. Dr. McDonnell points out that guidelines support the use of GLP-1 RA in any patient with an ASCVD (El Sayed et al, 2023). In particular, the reduction of stroke risk has been seen in semaglutide (Strain et al. 2022). She reminds us to ensure that patients also adhere to the use of statins for cardiovascular risk reduction.
COVID-19 and Diabetes
The effect of COVID-19 on glucose metabolism is being seen more and more (Khunti, et al 2021). Dr. McDonnell encourages treating the new diagnosis of diabetes. While some patients can recover from their illness and the new onset of diabetes, lifestyle changes and medications, including metformin should be initiated.
Metformin: Never Out of Fashion
In her opinion, Dr. McDonnell suggests metformin can also be an effective tool when a potent drug is needed in diabetes management. As a reminder, metformin should not be started in a patient with an eGFR at or below 30. Metformin compliance could be impacted by GI side effects so in these situations, Dr. McDonnell recommends using an extended-release version of metformin, which is available as metformin XR or metformin ER. This version is available in 500mg strength and can be dosed the same as regular metformin up to the maximally tolerated dose such as two pills twice a day or four pills once a day. In her personal experience, Dr. McDonnell the effect of metformin XR is not truly 24-hours long and she prefers to split the dose to twice a day by starting metformin at night time to slowly titrate the dose up. While metformin can be dosed up to 2550mg, there may not be much more of an impact at that dose (Garber et al, 1997).
But is metformin ER truly better than regular metformin?
Extended release metformin is a different, micronized formulation; studies done with the brand-name counterpart of this drug found that it was better tolerated than regular metformin (Schwartz et al, 2006). While studies have not been conducted using the generic version of extended release metformin, Dr. McDonnell shares that in her personal experience with patients, it can really make a difference in whether or not it is tolerated.
Goals for A1c
The Diabetes Prevention Program, which followed individuals for 15 years, showed that the more time that patients were in a normal range of an A1c less than 6%, the less likely they were to have complications (2015). The UKPDS trial endorsed a goal of 7.5%. Along those lines, the ACP set an A1c goal between 7% and 8% which was heavily based on the ACCORD trial which found an increased mortality rate in older individuals with a tight A1c control (Genuth and Ismail Beiji, 2012). With this evidence in mind, our expert’s preferred A1c goal is 7.5%, which she coined the “safe place,” because patients are less likely to have rapid progression of heart or kidney disease or retinopathy. Our expert believes we do not know the best goal for patients over 65 years with comorbidities, such as heart disease. Her advice is that we should not aggressively aim to achieve an A1c below 7% in this population seeing as how it is not always feasible from a cost or treatment burden perspective.
Expert Tips Before Using Insulin
In Dr. McDonnell’s opinion, insulin is not always the right medicine for type 2 diabetes but she employs it in patients with signs of severe hyperglycemia such as weight loss and polyuria. Insulin is beneficial in those in whom insulin deficiency is very advanced or transient.
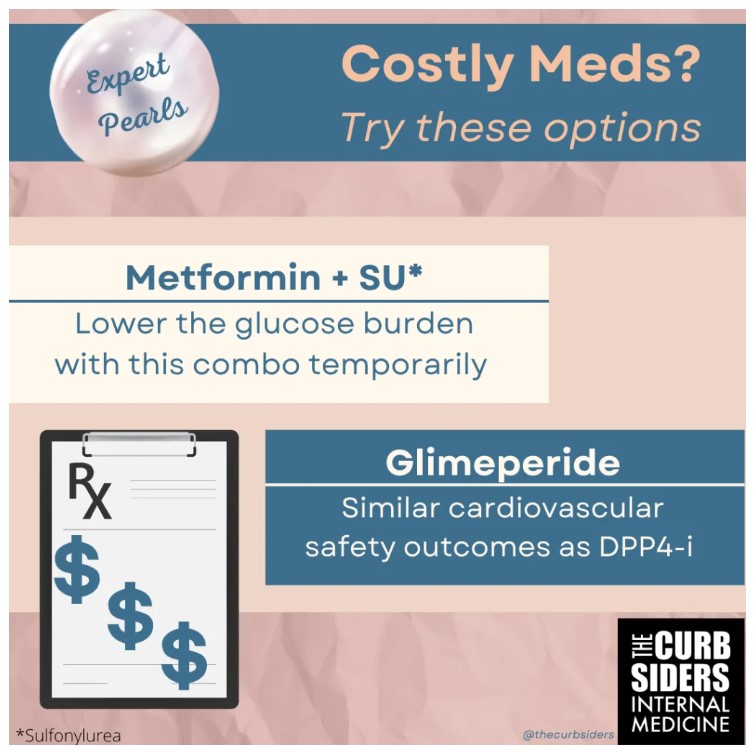
Our expert points out that cardiovascular safety outcomes of linagliptan and glimeperide are similar but we have to be cautious of hypoglycemia with sulfonylureas (Espeland et al, 2020). Before using insulin, she recommends a DPP4-i or low-dose sulfonylurea such as low-dose glimepiride, to protect from advancing into hyperglycemia.
Hyperglycemia and SGLT2i
At first, SGLT2i may not be the not ideal treatment choice in patients with hyperglycemia because they may experience more side effects related to the glucose such as yeast infections, tinea or glycosuria/polyuria (Yokoyama et al 2019). A good tip mentioned by our expert is to ask patients if they are already experiencing yeast infections from their diabetes ahead of considering SGLT2i. Many patients may be “suffering in silence” with yeast infections which can worsen when this class of drugs is used. Dr. McDonnell suggests starting medications in this class once the A1c is below 9%.
GLP-1 RA and Pancreatitis
Pancreatitis in the patient with diabetes is most likely seen due to gallstone disease or hypertriglyceridemia; the incidence of pancreatitis from the use of GLP-1 therapies is small (Zhang et al, 2022; Cao et al, 2020). Dr. McDonnell reassures the use of GLP-1 RA in patients who have had a cholecystectomy or recovered from gallbladder-induced cholecystitis. Patients with hypertriglyceridemia can be treated with GLP-1 therapies (Iqbal et al, 2022) and Dr. McDonnel suggests slow titration with these medications. She cautions against the use of GLP-1 medications in patients with active alcohol use disorder or pancreatic divisum. Dr. McDonnell suggests asking for a family history of pancreatitis as this could be a sign for CFTR gene mutation; she does not recommend using GLP-1 in this group.
GLP-1 RA and Cancer
While it may be due to a detection bias, studies have supported the higher risk of finding thyroid cancer in patients on GLP-1 therapies (Bezin et al, 2023). These medications should not be prescribed to a patient with a history of a pancreatic cancer or neuroendocrine tumor in the pancreas but can be considered in patients with a family history of pancreatic cancer.
Tirzepatide: New combination tool
Dr. McDonnell finds tirzepatide to be a patient-centered drug dosing modeling that allows the user to effectively “start low and go slow” and with fewer GI side effects. The latter is still not well understood but as Dr McDonnell explains it, the GIP agonism allows the GLP-1 RA to work with fewer GI side effects (Willard et al 2020). Weight loss with both diet counseling and the use of this drug has been found to be about 20% (Jastreboff et al 2022). As of this recording, the cardiovascular benefits of this drug class are still being studied.
Take-home points
- While insulin deficiency is rare, recognize it early
- Consider the goals for patients to select the right agent
- Aim for an A1c goal of 7.5% or lower if it is safe for the patient
Links
- American Diabetes Association Standards of Care in Diabetes—2023
- American Association of Clinical Endocrinology Practice Guidelines -2022
- National Diabetes Prevention Program