The following are excerpts from 9. Treatment of heart failure with preserved ejection fraction and subsections [pp 919 + 920] from the 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure:
While there is clear agreement that the diagnosis of HFrEF requires an LVEF , 40%, the exact definition of HFpEF is less clear. Accord-ing to the definition provided in this document (see Section 3), thediagnosis of HFpEF requires an LVEF ≥50%, whereas patients with LVEF between 40 and 49% are considered to have HFmrEF (for details, please refer to Section 3). Patients with HFmrEF have generally been included in trials of HFpEF. Accordingly, the guidance in this section applies to patients with both HFmrEF and HFpEF. As new data and analyses become available, it might be possible to make re-commendations for each phenotype separately.
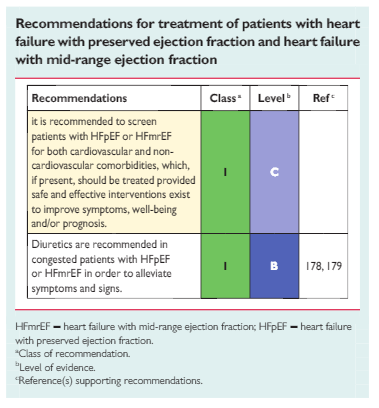
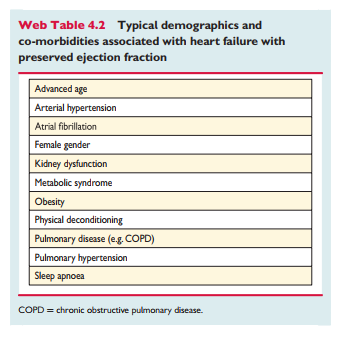
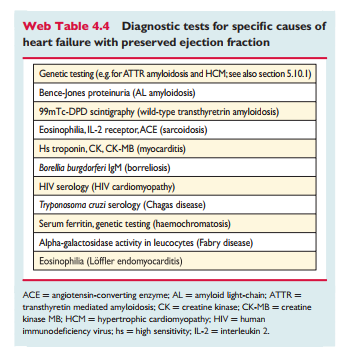
The pathophysiology underlying HFpEF and HFmrEF is heteroge-neous, and they are associated with different phenotypes including diverse concomitant cardiovascular diseases (e.g. AF, arterial hyper-tension, CAD, pulmonary hypertension) and non-cardiovasculardiseases [diabetes, chronic kidney disease (CKD), anaemia, iron de-ficiency, COPD and obesity].303,304 Compared with HFrEF patients,hospitalizations and deaths in patients with HFmrEF/HFpEF aremore likely to be non-cardiovascular.305,306 Therefore patients should be screened for cardiovascular and non-cardiovascular co-morbidities, which if present should be managed with interventions that have been shown to improve symptoms, well-being or out-come related to that co-morbidity and not to exacerbate HF (see Section 11).
No treatment has yet been shown, convincingly, to reduce mor-bidity or mortality in patients with HFpEF or HFmrEF. However, since these patients are often elderly and highly symptomatic, andoften have a poor quality of life, 307 an important aim of therapy may be to alleviate symptoms and improve well-being. 309
9.4 Other considerations
Patients in AF should receive an anticoagulant to reduce the risk of thromboembolic events (for details, see the ESC guidelines of AF316]. Antiplatelet agents are ineffective for this purpose. Renal dysfunction, which is common in this population, may contraindicate or increase the risk of haemorrhage with NOACs.
The optimal ventricular rate in patients with HFmrEF/HFpEF andAF is uncertain, and aggressive rate control might be deleterious.
Circumstantial evidence suggests that treating hypertension, of-ten predominantly systolic, is important in HFmrEF/HFpEF.127,31
The first-line oral hypoglycaemic drug for patients with HFpEF and HFmrEF should be metformin319 (see also Section 11.6). . . . However, aggressive manage-ment of dysglycaemia may be harmful. 153,320
Myocardial ischaemia may contribute to symptoms, morbidity and mortality and should be considered when assessing patients.
Patients with HFpEF and HFmrEF have impaired exercise toler-ance, commonly accompanied by an augmented blood pressure re-sponse to exercise and chronotropic incompetence. Combined endurance/resistance training appears safe for patients with HFpEF and HFmrEF and improves exercise capacity (as reflected by an increase in peak oxygen consumption), physical functioning score and diastolic function.307,321
Text
Resources:
2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. [PubMed Citation] [Full Text HTML] [Full Text PDF]. Eur J Heart Fail. 2016 Aug;18(8):891-975. doi: 10.1002/ejhf.592. Epub 2016 May 20.
2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart
failure – Web Addenda [Full Text PDF -you may need t register for a free ESC account to access this resource]