I have been reviewing kidney disease starting with the outstanding Curbsiders Podcast #67 and #69 (Resources 1 and 2 below) . Like all of The Curbsiders podcasts, they are outstanding. On Episode #69 at timestamp 15:15, there is an excellent brief introduction to acute interstitial nephritis – a good place to start.
I have included the abstracts for Resources 3 and 4 below as each abstract is a great really brief review of acute interstitial nephritis – these abstracts are also a great place to start.
The following are excerpts from and comments on Resource (3) which is a good quick review acute interstitial nephritis:
Definition and Etiology
Acute interstitial nephritis (AIN) is characterized by the
presence of inflammatory infiltrates and edema within the
interstitium, usually associated with an acute deterioration in
renal function. AIN represented 1–3% of all renal biopsies in
some studies.1,2 However, when the analysis was restricted to
patients with acute kidney failure, AIN accounted for 15–27%
of lesions.3,4 These studies suggest that AIN is a common
cause of acute renal dysfunction, but its true incidence might
even be underestimated by several reasons. First, a significant
number of patients in whom AIN is suspected on clinical
grounds is not submitted to a confirmatory renal biopsy
because empirical treatment is preferred, particularly in
elderly and frail patients. Second, milder forms of AIN can be
underdetected, either because of the absence or vagueness of
clinical symptoms or because acute renal failure is attributed
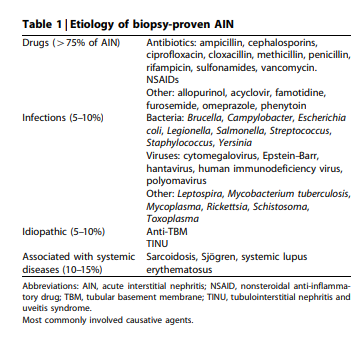
to other causes of renal injury.As shown in Table 1, the main causes of AIN can be
grouped as drug induced, infection related, idiopathic forms
(which would include tubulointerstitial nephritis and uveitis
syndrome (TINU) and anti-tubular basement membrane
(anti-TBM) disease), and AIN associated with sarcoidosis
and other systemic diseases (systemic lupus erythematosus,
Sjo¨gren, malignancies). Tubulointerstitial lesions that frequently accompany primary glomerulonephritis are usually
not included within AIN.A large and expanding number of drugs has been implicated in causing AIN and it can be stated that any drug can theoretically induce an episode of AIN. However, the majority of cases have been caused by antimicrobial agents and nonsteroidal anti-inflammatory drugs (NSAIDs). Table 1 lists those drugs most commonly involved in AIN.
Pathologenesis and Pathology is well discussed in the article on pp 956 – 958.
Clinical Features
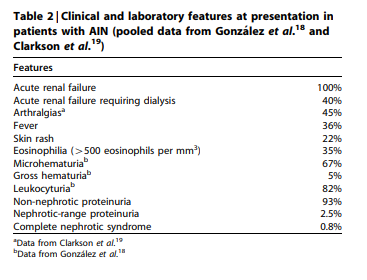
In patients with drug-induced AIN, mean delay between the
starting of the offending drug and the appearance of renal
manifestations is 10 days,11 although the latent period may be
as short as 1 day after some antibiotics or as long as several
months with NSAIDs. Table 2 shows the clinical and
laboratory features at presentation in two large and recently
published series of patients with AIN that included a total of
121 cases.18,19 Drug-induced AIN accounted for the majority
(91%) of the cases (of whom, 44% corresponded to NSAIDsinduced AIN). All the patients presented with an acute
worsening of renal function, whose severity led to dialysis
requirement in a significant proportion of cases. AIN-related
renal failure can be asymptomatic or accompanied by some
clinical or laboratory findings that, when present, are very
valuable to orientate the diagnosis.Treatment Of Drug Induced AIN
Conservative Treatment
Initial reports, most of them based on series of methicillin induced cases, depicted drug-induced AIN as a benign condition, with a rapid improvement of renal function after the removal of the inducing agent. However, later studieswith a larger number of patients and a longer follow-up revealed that a significant proportion of patients, ranging from 30 to 70%, did not fully recovered their baseline renal function.6,11,21,28–31 Duration of treatment with the offending drug or duration and severity of renal failure have not shown a clear correlation with the levels of serum creatinine at the end of follow-up. Whereas some studies found a predictive role of diffuse interstitial infiltrates in opposition to patchy ones,30 other ones have not corroborated these findings.6 Conversely, the extent of interstitial fibrosis has shown a clear impact on the risk of chronic renal impairment after a druginduced AIN in some studies.18,31
Regarding the withdrawal of the causative agent, it is
important to remark that in some patients with biopsy proven AIN and in whom clinical and pathological findings
strongly point out to a drug-induced form, the offending
drug cannot be identified even after meticulous investigations. Reasons for such failure include self-treatment with antibiotic mixtures, polymedication, and the huge and largely uncontrolled consumption of NSAIDs among the general population, the two latter issues being particularly relevant among elderly people.Steroid Treatment
The role of steroids in the treatment of drug-induced AIN
remains controversial. Several studies reported a significantly better outcome in patients who were treated with steroids.6,21,28 In some cases, the response to steroids was dramatic, with a rapid recovery of diuresis and serum
creatinine decrease. However, the number of patients
included in such positive studies was short and other studies
failed to found a beneficial influence of steroids in comparison with conservative measures.11,32Treatment of Other Types of AIN
Steroids are the mainstay of treatment in idiopathic AIN,
TINU, and AIN associated with systemic diseases, including
the recently reported association of AIN with autoimmune
pancreatitis.11,12,26,27 Plasmapheresis and cytotoxics have
been used in anti-TBM disease. In patients with idiopathic
AIN resistant to steroids, anecdotal reports suggest benefit
from cyclophosphamide and cyclosporine.33 A recent report
of eight patients with steroid-dependent, recurrent AIN
documented an interesting beneficial effect of mycophenolate
mofetil.34 In patients with NSAID-induced AIN and
nephrotic syndrome, withdrawal of the offending drug has
proved to be the most effective treatment, whereas the
addition of steroids does not alter the clinical course.17Conclusions
AIN represents a frequent cause of acute kidney injury. Druginduced AIN is currently the commonest etiology of AIN,
antimicrobials and NSAIDs being the most frequent offending
agents. Pathogenesis is based on a cell-mediated immune
response in most patients and removal of the offending drug
is the mainstay of the treatment. However, a significant
proportion of patients, ranging from 30 to 70%, did not fully
recovered their baseline renal function, likely because of the
rapid transformation of interstitial cellular infiltrates into
large areas of fibrosis. Although prospective randomized
trials in AIN are lacking, recent retrospective studies suggest
that early steroid treatment (within 7 days after diagnosis)
improves the recovery of renal function.
Resources:
(1) #67: Chronic Kidney Disease Pearls with @kidney_boy, Joel Topf
NOVEMBER 13 from The Curbsiders Internal Medicine Podcasts [Link is to the episodes list page].
(2) #69: CKD Prescribing Do’s and Don’ts with @kidney_boy, Joel Topf
NOVEMBER 27, 2017 from The Curbsiders Internal Medicine Podcasts [Link is to the episodes list page].
- 15:15 Acute Interstitial Nephritis, Beta Lactam Antibiotics, and the risk of Acute kidney injury +/- CKD with Proton Pump Inhibitors
(3) Acute interstitial nephritis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Kidney Int. 2010 Jun;77(11):956-61. doi: 10.1038/ki.2010.89. Epub 2010 Mar 24.
Abstract
Acute interstitial nephritis (AIN) represents a frequent cause of acute kidney injury, accounting for 15-27% of renal biopsies performed because of this condition. By and large, drug-induced AIN is currently the commonest etiology of AIN, with antimicrobials and nonsteroidal anti-inflammatory drugs being the most frequent offending agents. Pathogenesis is based on an immunologic reaction against endogenous nephritogenic antigens or exogenous antigens processed by tubular cells, with cell-mediated immunity having a major pathogenic role. The characteristic interstitial infiltrates, mostly composed of lymphocytes, macrophages, eosinophils, and plasma cells, experience a rapid transformation into areas of interstitial fibrosis. A significant proportion of AIN has nowadays an oligosymptomatic presentation, although the presence of specific extrarenal symptoms such as fever, skin rash, arthralgias, and peripheral eosinophilia has an important role to orientate clinical diagnosis. Identification and removal of the offending drug are the mainstay of the treatment, but recent studies strongly suggest that early steroid administration (within 7 days after diagnosis) improves the recovery of renal function, decreasing the risk of chronic renal impairment. Delayed steroid treatment, when interstitial fibrosis has taken place, would have a less pronounced or nule therapeutic benefit.
(4) Drug-induced acute interstitial nephritis [PubMed Abstract]. Nat Rev Nephrol. 2010 Aug;6(8):461-70. doi: 10.1038/nrneph.2010.71. Epub 2010 Jun 1.
Abstract
Acute interstitial nephritis (AIN) is a common cause of acute kidney injury. Many etiologies of AIN have been recognized–including allergic/drug-induced, infectious, autoimmune/systemic, and idiopathic forms of disease. The most common etiology of AIN is drug-induced disease, which is thought to underlie 60-70% of cases. Multiple agents from many different classes of drugs can cause AIN, and the clinical presentation and laboratory findings vary according to the class of drug involved. AIN is characterized by interstitial inflammation, tubulitis, edema, and in some cases, eventual interstitial fibrosis. A definitive diagnosis of AIN can be established only by kidney biopsy. Noninvasive tests such as (67)gallium scintigraphy and testing for eosinophiluria have limited diagnostic utility. The mainstay of therapy for drug-induced AIN is timely discontinuation of the causative agent. Although the benefits of corticosteroid therapy remain unproven, they do appear to have a positive effect in some patients with drug-induced AIN, especially when treatment is initiated early in the course of the disease. In general, the prognosis for drug-induced AIN is good, and at least partial recovery of kidney function is normally observed. Early recognition is crucial because patients can ultimately develop chronic kidney disease.