The following are excerpts from Resource (1) Measuring energy expenditure in clinical populations: rewards and challenges:
Abstract:
The measurement of energy expenditure (EE) is recommended as an important component of comprehensive clinical nutrition assessments in patients with altered metabolic states, who failed
to respond to nutrition support and with critical illness that require individualized nutrition support. There is evidence that EE is variable in patients with metabolic diseases, such as chronic renal disease, cirrhosis, HIV, cancer cachexia, cystic fibrosis and patients under intensive care. By using appropriate techniques and interpretations of basal or resting EE, clinicians can facilitate the adequate nutrition support with minimum negative impacts from under- or overfeeding in these
patients. This review is based on our current understanding of the different components of EE and the techniques to measure them, and to re-examine advances and challenges to determine energy needs in clinical populations with more focuses on the obese, pediatric and elderly patients. In addition, technological advances have expanded the choices of market-available equipments for assessing EE, which also bring specific challenges and rewards in selecting the right equipment
with specific performance criteria. Lastly, analytical considerations of interpreting the results of EE in the context of changing body composition are presented and discussed.Introduction
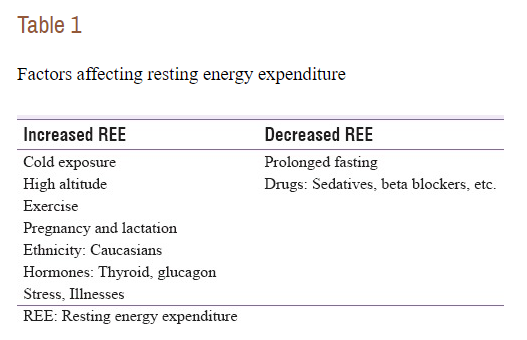
Establishing a patient’s energy expenditure (EE) is an important step in determining nutritional needs. EE has three main components: basal metabolic rate, thermic effect of food or diet-induced thermogenesis, and physical activity EE. Many factors, such as age, body composition, thyroid hormones, catecholamines, ambient and body temperature, disease states and drugs/treatments influence these components to some extent and thus total EE. Basal metabolic rate (BMR), the minimal amount of energy expended for homeostatic
processes, is a major component (about 60–80%) of total EE in free-living individuals and is an even larger component for hospital-bound patients due to a decreased level of physical
activity.Fat-free mass has been found to be the strongest determinant of between-individual variability of BMR during weight-stable periods and after moderate weight loss.1–4 Thermic effect of food represents the increase in EE above resting EE (around 8 12% of the energy
intake) following meal ingestion and has been linked to nutrient composition and energy
content of food consumed. The last component of EE, physical activity EE, is defined as the additional EE (above resting EE) needed to perform physical activities, which can be further divided into exercise and non-exercise activity thermogenesisAs most clinical applications use indirect calorimetry to assess EE, we will briefly overview this method and point out the subtle differences in some systems that could lead to potential errors in measurement. It has been recognized for over a century that metabolic conversion of food energy has a varying heat of combustion or releases a different amount of energy per unit of oxygen used (oxidation), depending on which substrate/fuel is being converted (carbohydrate, protein or fat). Thus, by measuring oxygen consumption (VO2) and carbon dioxide excretion (VCO2), the net energy released from the fuels is being expended, which is typically expressed as calories (or kilocalories, kcal or KJ) per unit of time (min to 24 h) by
using standard equations, such as the commonly used Weir’s equation:12EE(kcal) = 3.941 × VO2(L) + 1.106 × VCO2(L).
There is a small contribution by protein oxidation as measured by nitrogen excretion in the urine, which can be neglected without much added error unless the patient’s protein turnover is substantially high (estimated 1% error in each 12% total calorie from protein oxidation).7
Metabolic carts (shown in Figure 1) are the current standardized equipment for determining resting EE in clinical and field settings. This method consists of a gas collection/sampling system (face-mask, mouthpiece or a domed hood/canopy), a ventilation/flow rate-sensing system, oxygen and carbon dioxide gas analyzers, one or more calibration gas bottles (mixed gases with verified concentrations for O2, CO2 and typically balanced with N2), environmental assessments (temperature, humidity and barometric pressure) and a central
computer to interface among all the measurement components and with the user. Currently, there are three different types of O2 analyzers commonly used in metabolic cart systems,
paramagnetic, electrochemical (fuel cell), and zirconium oxide, while most CO2 analyzers still rely on the non-dispersive infrared sensors.11 Despite the technical differences, properly
maintained and calibrations should yield comparable performances between metabolic carts.Accuracy, validity, reliability and sensitivity of indirect calorimetry
Accuracy is defined as the closeness of the measurement to a true value, and refers to the specific measurement with a metabolic cart system. For example, the accuracy of the analyzers can be directly compared with a known traceable standard, such as reference gases with true concentration values. . . . The true accuracy of a metabolic cart system is difficult to measure as it integrates the accuracies and balances the errors of all the sensors and operation factors.
Validation refers to how a measurement compares to another similar measure (with the assumption that latter has the acceptable accuracy), or to a standard procedure/input with
measurable outcomes. For example, different metabolic carts have been ‘validated’ against the Douglas bag method,17 an established metabolic cart system (for example, Deltatrac II; VIASYS Healthcare Inc., SensorMedics, Yorba Linda, CA, USA), and/or alcohol burns. The study by Cooper et al. [Link is to the PubMed Abstract, Resource (5) below] 18 is a good example of such a validation study, where six metabolic cart systems were included. The Deltatrac II was used as the common reference criterion to which the remaining five systems were compared. The sample size of each within-subject comparison group was 10–17, and the between-instrument coefficient of variation in measured resting EE ranged from 5.4 to 12.2%. Only one was found to be statistically different from the reference Deltatrac II carts, but the 95% confidence intervals
of the difference were as wide as around 600–1000 kcal.Reliability is generally the ability of the system (or a measurement procedure) to perform at different times. It is commonly reported as repeatability within an individual or between alcohol combustion tests (coefficient of variation). It has been reported that systems such as the Sensormedics 2900 (Yorba Linda, CA, USA) and the Deltatrac MD 1 (Datex, Helsinki, Finland) could achieve a coefficient of variation of 2% or less,19 and the Deltatrac II resulted 3.0–3.6%.18
Sensitivity is the magnitude of change that is measurable by the system. Depending on the analyzer, calibration gases, ventilation rates sensors and the analytical processing (data
smoothing), the sensitivity of metabolic carts can vary significantly. The term precision can sometimes be used to refer to sensitivity. Although there are some reports and recommendations related to sensitivity for metabolic carts in exercise tests (VO2max),16 very limited data exist in the resting EE measurements. This is partly due to the lack of a calibration system that can provide a dynamic or graded input to the indirect calorimeter, which is similar to a phantom for an imaging system (for example, a magnetic resonance imaging scanner).Obesity
[Predictive equations used to prescribe a patient’s calorie needs are inaccurate for a number of reasons.] Predictive equations include only weight as a variable and these analyses illustrate the limitations associated with using predictive equations in samples dissimilar to those from which they were derived. A consensus regarding which weight to use (that is, actual weight,
ideal weight, adjusted weight, and so on) is lacking in the literature.33 Given the difficulty in accurately determining energy needs for obese patients, using indirect calorimetry is advised to get an individual estimate of nutritional needs
The following are excerpts from Resource (2) below, Indirect calorimetry: an indispensable tool to understand and predict obesity:
Introduction
Obesity is fundamentally a consequence of energy imbalance with energy intake chronically exceeding energy expenditure. In 2013,the American Medical Association adopted a position that’recognizes obesity as a disease requiring a range of medical interventions to advance obesity treatment and prevention’. . . . how energy metabolism is regulated varies widely across individuals. Identifying individuals who are metabolically prone to weight gain(thrifty) and the related metabolic diseases and intervening accordingly using tailored approach is a key to change the courseof the obesity epidemic. Here we reviewed data from indirect calorimetry to gain insights into the determinants of energy metabolism and its role in weight gain, and therefore the use of such method to combat obesity.
Indirect Calorimetry
Metabolic carts are ‘user-friendly’ indirect calorimetric devices to assess energy expenditure over shorter periods of time (from minutes to a few hours). Exhaled gas are captured using ventilated hood, canopy, face mask or mouthpiece connected to oxygen and carbon dioxide analyzers mounted on mobile carts. These system are relatively inexpensive and easy to use. The gaseous sampling attachment, however, hinders locomotion and limits study duration to a few hours maximum. Metabolic carts are most commonly used to measure resting metabolic rate (RMR) and in some cases diet-induced thermogenesis, which when combined with an estimated physical activity level provides broad estimates of TDEE [Total Daily Energy Expenditure].
Metabolic Predictors of Obesity: What Do We Know From Indirect Calorimetry
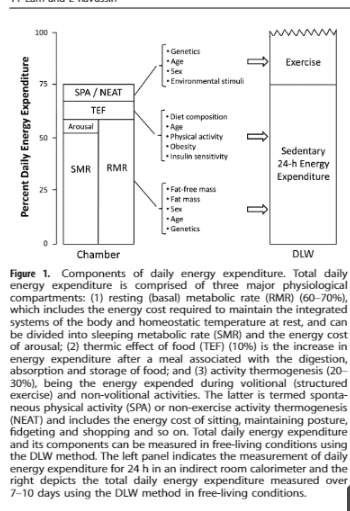
A unique feature of indirect calorimetry is to provide real-time energy expenditure data that makes it ideal to distinguish and investigate the various components of TDEE, namely resting metabolic rate (RMR), thermic effect of food and activity energy expenditure (Figure 1). Furthermore, when coupled with measures of urinary nitrogen excretion, indirect calorimetry also informs on substrate utilization and energy balance can be separated into protein, carbohydrate and lipid balances.
Energy metabolism research using indirect calorimetry has sofar provided evidence for some key metabolic predictors ofobesity:(1) Resting metabolic rate: As early as in the 1970 s, James and Trayhurn9 proposed that obese individuals might have a ‘greater than normal metabolic efficiency’ that predisposed weight gain.Therefore, given similar body size, energy intake and physical activity level, individuals who have a lower metabolic rate will have higher energy surplus and thus greater fat storage. There is a good deal of evidence supporting this hypothesis.2) Spontaneous physical activity: Activity energy expenditure is the most variable component of energy expenditure, accounting for15–50% of TDEE in very sedentary to highly active individuals.25 Activity energy expenditure can be further broken down into energy spent in structured exercise (sports and fitness-related activities) and that spent in SPA including daily living activities, fidgeting, posture maintenance and non-volitional ambulatory behaviors such as pacing.26 SPA in whole-room respiratory chambers is defined as the percentage of time during which the participant is active, and thus is a measure of duration of motion independent of work intensity. In our laboratory, participants spent 4–17% of their time on SPA that approximated to 400–3000 kJ/day.8,27 In a longitudinal study in male non-diabetic Pima Indians, SPA was positively correlated with TDEE at baseline and negatively with the rate of body weight and fat mass changes at 33 months follow-up,28 suggesting that a low level of SPA may be a predictor for obesity risk.
3) Twenty-four-hour respiratory quotient (RQ): It has long been proposed that reduced fat oxidation favors positive fat balance and thus predisposes obesity.32 Testing such hypothesis requires quantifying energy substrate oxidation by tracking changes in oxygen consumption and carbon dioxide production using indirect calorimetry with simultaneous measures of urinary nitrogen excretion and calculation of RQ, that is, VCO2/VO2.Ingeneral, RQ is in the range of 0.70 (complete fat oxidation) to 1.0(complete carbohydrate oxidation) and anywhere within this range indicates that a mixture of energy substrates are oxidized simultaneously. There are circumstances that lead to deviations from this expected range, for example, loss of ketone bodies (in urine or expired air) will cause a drop of RQ to < 0.70, whereas lipogenesis will increase RQ to > 1.0. 33 Physiological character-istics including diabetes, high urinary glucose excretion, hypo- or hyperventilation also skew the interpretation of substrate utilization based on RQ values.
Similar to that with RMR, the relationship between obesity andRQ is dynamic in response to weight changes.
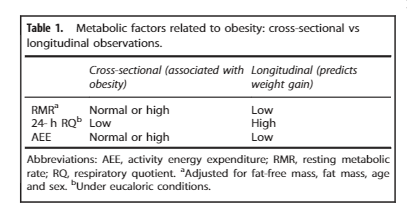
ConclusionIndirect calorimetry is the most commonly used method tomeasure energy expenditure in the research setting and has provided unprecedented insights into the mechanisms by which energy homeostasis is regulated in response to weight loss or weight gain. The literature clearly suggests that RMR, SPA and RQ are metabolic predictors for obesity risk (Table 1). This can be an important basis to identify at-risk individuals, thus allowing early preventative interventions to curb the increasing prevalence of obesity. Mathematical modeling based on indirect calorimetry data is likely to have a pivotal role in prescribing person-specific interventions and better inform on public health policies to halt the rise of global obesity.
The following is an excerpt from Resource (4) below, Indirect Calorimetry: From Bench to Bedside:
Resources:
(1) Measuring energy expenditure in clinical populations: rewards and challenges [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur J Clin Nutr. 2013 May;67(5):436-42. doi: 10.1038/ejcn.2013.38. Epub 2013 Feb 27
(2) Indirect calorimetry: an indispensable tool to understand and predict obesity [PubMed Abstract] [Full Text HTML] . Eur J Clin Nutr. 2017 Mar;71(3):318-322. doi: 10.1038/ejcn.2016.220. Epub 2016 Nov 16.
(3) Indirect Calorimetry: A Practical Guide for Clinicians [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Nutr Clin Pract. 2007 Aug;22(4):377-88.
(4) Indirect Calorimetry: From Bench to Bedside [PubMed Abstract] [Full Text HTML] [Full Text PubReader]. Indian J Endocrinol Metab. 2017 Jul-Aug; 21(4): 594–599.
(5) Assessing validity and reliability of resting metabolic rate in six gas analysis systems [PubMed Abstract] [Full Text PMC] [Full Text PDF]. J Am Diet Assoc. 2009 Jan;109(1):128-32. doi: 10.1016/j.jada.2008.10.004.
(6) Employing RMR technology in a 90-day weight control program [PubMed Abstract] [Full Text PDF]. Obes Facts. 2008;1(6):298-304. doi: 10.1159/000178026. Epub 2008 Dec 2
The Role of Energy Expenditure in the Differential Weight Loss in Obese Women on Low-Fat and Low-Carbohydrate Diets [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Endocrinol Metab. 2005 Mar;90(3):1475-82. Epub 2004 Dec 14
When To Use Metabolic Carts In Clinical Practice, Thursday, January 14, 2016. From Dr. Sharma’s Obesity Notes
Dietary effects on resting metabolic rate in C57BL/6 mice are differentially detected by indirect (O2/CO2 respirometry) and direct calorimetry [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Mol Metab. 2014 Mar 21;3(4):460-4. doi: 10.1016/j.molmet.2014.03.003. eCollection 2014 Jul.
Should we abandon indirect calorimetry as a tool to diagnose energy expenditure? Not yet. Perhaps not ever. Commentary on Burnett and Grobe (2014) [PubMed Abstract] [Full Text] [Full Text PDF]. Mol Metab. 2014 Apr 18;3(4):342-4. doi: 10.1016/j.molmet.2014.04.003. eCollection 2014 Jul.
QUARK RMR INDIRECT CALORIMETRY
THE GOLD STANDARD FOR CLINICAL NUTRITIONAL ASSESSMENT
The Most Accurate Indirect Calorimetry solution for Research and Clinical Practice
Indirect calorimetry (continuous VO2, VCO2)
- Accurate measurement Metabolism substrate (RQ, FAT, CHO, PRO)Provided with flow-based-dilution Canopy Hood & Multiuse Face
- MasksEthanol Burning Kit
- Either Spontaneously Breathing subjects or Mechanically Assisted patientsICU Kit for ventilated patients (option)
The Quark RMR is a new generation metabolimeter designed to measure Resting Energy Expenditure (REE) through indirect calorimetry provided in a compact bedside solution. It is designed to accurately and instantaneously measure energy requirements of either spontaneously breathing or mechanically- assisted patients. Additionally, the Quark RMR identifies metabolism substrate utilization, allowing improved nutrition and evaluation of nutritional therapies. Tests can be performed with either a flow-dilution canopy hood, a face mask, or (optionally) connected with a ventilator in Intensive Care Unit (ICU) applications.
Indirect Calorimetry and Metabolic Cart by Chris Nickson, Last updated August 30, 2017 from Life In The Fast Lane.
Indirect Calorimetry: A Practical Guide for Clinicians [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Nutr Clin Pract. 2007 Aug;22(4):377-88.