Use of the CHA2DS2-VASc and HAS-BLED Scores to Aid Decision Making for Thromboprophylaxis in Nonvalvular Atrial Fibrillation [Full Text HTML ] [Full Text PDF] [List of Articles Citing This Article]. Circulation.2012; 126: 860-865.
Below are some excerpts from this article:
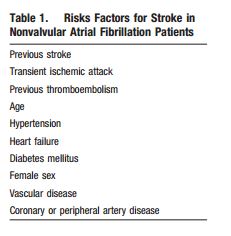
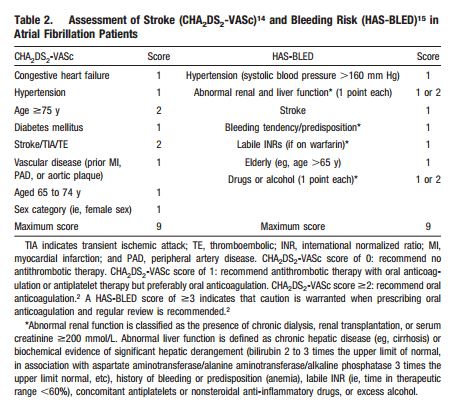
Although simple, the CHADS2 score does not include many common stroke risk factors, and its limitations have recently been highlighted.10,11 Even patients classified as low risk by CHADS2 in its original validation study have a stroke rate of 1.9%/y,6 which is close to the criterion of a cardiovascular event rate of 20% over 10 years for primary prevention strategies (eg, the use of statins). A recent analysis also confirms that patients with a CHADS2 score of 0 were not all low risk, and anticoagulation decisions based simply on a CHADS2 score of 0 (the category recommended to have no antithrombotic therapy or aspirin in some guidelines) may be insufficient to avoid stroke/thromboembolism in patients with AF.12
[So don’t use CHADS2 score rather use CHA2DS2-VASc]
Despite the abundant evidence in favor of OAC for stroke prevention, a recent systematic review19 investigating the current treatment practice for stroke prevention in eligible AF patients revealed ongoing underuse of OAC treatment (defined as <70% of eligible patients receiving OAC), particularly among those patients at highest risk (ie, those with a previous stroke/transient ischemic attack).
Overestimation of the risk of bleeding by physicians is a key barrier to OAC prescription,21 particularly among elderly patients, in whom aspirin is perceived as a safe and viable alternative. However, a patient-level data analysis of 12 trials comprising almost 9000 patients that assessed the effect of antithrombotic therapy on stroke prevention, serious hemorrhage, and vascular events demonstrated that although the risk of all these outcomes was greater with increasing age, OAC remained significantly protective against ischemic stroke regardless of the patient’s age.22
Thus, aspirin is not safer than warfarin in elderly people, but it is substantially less effective.
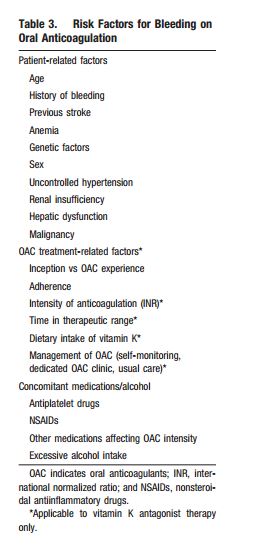
Many risk factors for stroke are also risk factors for bleeding on OAC23 (see Table 3). Integral to the decision about whether to anticoagulate an AF patient is the assessment of bleeding risk, which must be undertaken on an individual basis.
[Use HAS-BLED to assess bleeding risk.]
HAS-BLED should not be used on its own to exclude patients from OAC therapy; it allows the clinician to identify bleeding risk factors and to correct those that are modifiable, ie, by controlling blood pressure, removing concomitant antiplatelet or nonsteroidal antiinflammatory drugs, and counseling the patient about reducing alcohol intake (if excessive). Thus, bleeding risk assessment with HAS-BLED should not be used as an excuse not to prescribe OAC but rather to highlight those patients in whom caution with such treatment and regular review is warranted.
List of Articles Citing This Article (as of date of blog post)
Articles citing this article