I’ve been reviewing congenital heart disease starting with Dr. Helman’s outstanding podcasts EMC Episode 84 – Congenital Heart Disease Emergencies and his EMC Best Case Ever 47 – Cyanotic Infant.
Following the excellent resources in the above shownotes, I eventually came across the podcast ELIZABETH WEINSTEIN: HEARTBREAKERS – SICK KIDS, CONGENITAL HEARTS. This brief 30 minute podcast is outstanding and complements the above two EMC podcasts and the resources they site. This podcast is on the site www.freeemergencytalks.net/.
The following notes are from Dr. Weinstein’s excellent talk:
For the next half hour we are going to be talking about congenital heart disease. And a little disclaimer before we go: we are not to talk about any of the usual suspects. So no discussion of prostaglandins or exons or boot shaped anything. Were not to talk about all those murmurs that radiate to the axilla and which you can hear anyway.
Instead were to focus on what happens to these kids as they get bigger after they’ve had their complicated repairs and they’re on their medications and they been sent home. To grow up.Because eventually all these kids get sick. And the routine pediatric illnesses affect of these children a little bit differently. Warm maybe the children have issues with their complex congenital lesions. Or maybe we see them even as adults with palliative repairs that are starting to fail.
Regardless of what gets these patients to your doorstep it’s your job to fix it. All arrive there with unique physiology. Physiology that is unlike anything you ever learned in medical school. And like it or not, it’s incumbent on us is emergency physicians, to understand the critical nuances of these physiology is so that we can intervene appropriately when these folks get sick. And maybe even more importantly not do things that are meant to make them worse.
Consider for example this case seen recently by one of our grads in his community hospital: a six-year-old little history of a Fontan procedure brought in by EMS because he’s feeling lousy. He’s blue. The SATs are in the 60s.
Where do you start with this kid? After you’ve gone to Google to frantically figure out what the heck a Fontan procedure is in the first place where you even begin?
Do I give the child oxygen? If you raise your hand keep it up there if you feel confident that oxygen is the right choice for this child. Or have any idea what kind of SATs you’re shooting for and how much oxygen to give them?
Put your hand up if you want to give the child IV fluids. Peter hand up there if you feel confident that IV fluid is the right thing to do.
How about this case: a four-month-old with a known VSD. We all understand this lesion correct. Except this little ones Sasser in the toilet and he looks like crap. We give them oxygen and it does nothing. We give IV fluid and it does nothing. We of morphine and it does nothing. And we give multiple other interventions and there’s not a single favorable change and SATs are in the 30s. He finally gets innovated with some ketamine and stabilizes just enough and get into the operating room for definitive repair of what it turns out is an undiagnosed tetralogy of flow.
Congenital heart disease occurs or rate of about 7 to 10 per thousand live births. And that number has been constant over the last 50 years. The number that hasn’t been constant has been survival which is getting much better such that between 1985 and 2000 the number of adults in the US with congenital heart disease has increased by 85%. Bottom line is this: the majority of these children are expected to live into adulthood. So if you haven’t seen them yet in your emergency department, get ready because they are coming.
With that in mind were to spend the next 25 min. doing a couple of things: we are going to talk about to common high-yield cyanotic situations and their associated physiology is. We’ll talk about some common surgical repairs so that you know helpful issues when these kids get sick. And last but not least will do some high-yield quick tips to to the questions that everybody has like: what are their satss supposed to be? Can I give them oxygen? How much?
So let’s dive in.
The first case is a 3 1/2 month old brought my grandma after he starts crying at home and becomes increasingly fussy. She says that he’s got some history of heart disease but she’s not sure what it is and he doesn’t take any medicines Annie’s not had any surgeries. And on physical exam the kid looks like crap. Heart rate in the 170s, respiratory rate in in the 60s, and sats are 50%. He is distressed but his breath sounds are clear. What now?
When we start talking about congenital heart disease, we are really talking about a group of disorders in which there is some derangement in either their pulmonary or systemic blood flow. Let’s face it, the heart is a pretty straightforward job. Deoxygenated blood arrives at the right side of the heart and gets bumped to the lungs and oxygenated blood arrives at the left side of the heart and gets bumped to the body.But there a lot of ways in which that very simple pumping mechanism can become fouled up. And those foulups are what we consider congenital heart disease.
Congenital heart disease typically breaks down into one of four things: they can have not enough pulmonary blood flow. They may have too much pulmonary blood flow. Not enough systemic blood flow. Or not enough coronary artery blood flow.
If you can figure out what the derangement in blood flow is then that will help you tremendously in figuring out how to intervene and help these folks and to troubleshoot when they get sick. Thankfully, figuring out the arrangements is pretty easy.
And for those of you who have heard Dr.Blank’s [couldn’t get name] elegant presentation on neonatal emergencies this is her approach to the problem.
If the kid is blue they don’t have enough pulmonary blood flow. If they’re pink they may have too much pulmonary blood flow. And if they’re gray they don’t have enough’s systemic blood flow. So it’s blue, pink, or gray.
Add to that a thoughtful differential diagnosis: in this case may be sepsis or pulmonary hypertension. Maybe grandmother is been a little overzealous with the ambusol and the kid’s got methemaglobinemia.
Or maybe as many of you surmised as you look at the case this is a child who has had a Tet spell.
Tetralogy of flow accounts for about 10% of all cyanotic heart disease. It is one of the most common causes of cyanosis in kids over 3 months of age. It is defined as many of you will recall by pulmonary stenosis or right ventricular outflow tract obstruction, overriding aorta, VSD, and right ventricular hypertrophy.
Now clinically these kids will look a little bit different at any given moment in time depending upon the degree of outflow tract obstruction, and their degree of systemic vascular resistance. Here’s how that works: kids was really mild pulmonary stenosis at usually able to maintain good pulmonary blood flow. These kids have normal SATs a baseline and we often refer to them as pink Tets.They may go quite some time before they’re diagnosed because their symptoms are so mild.
By contrast children with tight outflow tract obstructions are often quite hypoxic it baseline with SATs in the 70s. At any moment in time that picture can change if there systemic vascular resistance drops. When SVR drops they will preferentially shun blood from the right side of the heart through the VSD to to the left side of the heart rather than trying to navigate that tight outflow tract. This results obviously in increasing hypoxia.
Now the tet or hyper cyanotic spell is the dreaded event for these kids before they have surgical repair. What happens is there some sort of innocuous event. Maybe the kid gets upset he starts crying maybe he’s taking a dump and whatever it is results in dropping systemic vascular resistance. And when you drop systemic vascular resistance and these kids you get increased shunning from the right side of the heart to the left side of the heart. This results in a falling PO2 a rising CO2 and the falling pH. All of that increases your pulmonary vascular resistance and stimulate your respiratory drive. And this results in increased venous return. An increased venous return to the right side of the heart against that fixed lesion results in even more shunting. The cycle continues in perpetuity until the kid either hits that dreaded seizure –coma – death trifecta (which we try very hard to avoid) or until some really smart person decides to intervene.
Now there are a couple of ways in which we can stop this: we can work to increase their systemic vascular resistance and we can do that by putting them in the knee to chest position, by giving them IV fluid, or by giving the medications like ketamine or phenylephrine. We can try to decrease their venous return again by putting them in the knees just position or by giving the medications that might decrease that respiratory drive. We can try to drop the pulmonary vascular resistance again with things like 02 or morphine.
And then there are a couple of strategies that seem counterintuitive. We can give them esmolol which seems kind of silly when we are tryingTo raise that systemic vascular resistance. But this is thought to relax that outflow tract obstruction and also by slowing the heart rate to decrease some of the shunting problem. We can always intubate and sedate.
Perhaps the most important thing we can do is to calm these children. You would be amazed at how successful in aborting a Tet spell. We actually last week had a 16-month-old undiagnosed tet arrive in our emergency roomIn the midst of a Tet spell. Everyone was panicking and we stuck a knife pad in front of the child and his stats shot up to 100%!So maybe iPads should be on there as part of your armamentarium. But the real point is to calm them.
There is sort of a preferred order of this. I’m to give you my top five. And let you know that I skipped a couple of steps and I’ll let you know why. At the end of the day if you’re in the weeds this is your plan.
Put the kid in the knee to chest physician. Calm them. Give them high flow oxygen. Give them morphine an IV fluid and I don’t care which you do first. And if you’re still having problems go to ketamine. Ketamine as we’ve just heard is ubiquitous in the emergency department. We all know the dose. The janitor knows the dose. He’s like two per kilo just give it. Your nurses can pull it off really quickly. You can give it IM.
This is my go to algorithm: knee to chest and calm them. High flow 02, morphine, IV fluid, and ketamine. This will get you out of most Tet spells.
Now complete repairs is typically what we do for these children and it happens by about six months of age. We patched the VSD we open the outflow tract obstruction and we call it a day.
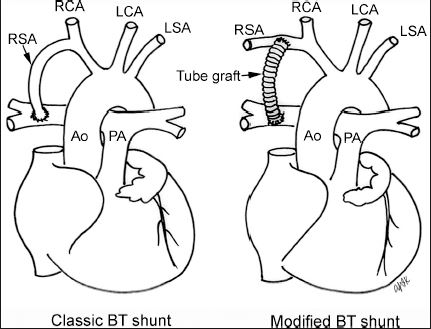
Now sometimes the patient’s need a palliative repair to get them big enough to undergo the definitive repair. This is for children whose outflow tract is so tight that they can’t maintain adequate pulmonary blood flow. For those kids we do a something called the Blalock-Taussig shunt. [The picture below is not the one that the speaker used.]
For all intensive purposes this is a man-made patent ductus arteriosus. It allows those children to maintain pulmonary blood flow in the presence of in obstructive lesion until they’re big enough to undergo definitive repair. Survival for these kids is great: 86% at 30 years. But it doesn’t come without a few bumps along the way.
Next case is a 30-year-old man status post remote repair of to tetralogy of Fallot complains of an episode of syncope while participating in a rally. Now he feels pretty good. SATs are normal and the heart rate is 83.And here’s an EKG which doesn’t project very well. I think you can all appreciate that there is a right bundle branch block pattern. And the nurse hands you the rhythm strip and says he keeps having this ventricular ectopy what you want me to do. And you say I’m going to admit the guy since he’s failed everything I tried to do and I’ll think about the ectopy a little more.
In the meantime the paramedics drop off a rhythm strip that shows what he was doing when they picked him up. [not available on website]
So let’s talk about what happens to these folks as they get a little older. First of all a right bundle branch block pattern is the rule. More than 90% of patients will have the right bundle pattern after surgery. As they get older couple of other things happen. Some of them will develop some degree of pulmonary regurgitation or restenosis that requires an intervention. Right ventricular dysfunction is common in these folks. So keep this in mind if you’re attempting to resuscitate these people is it’s easy to fluid overload them.
Sudden cardiac death is a real phenomenon. 4% at 25 years. Thought to increase if there QRS duration is greater than 180 ms.So if you see a wide complex QRS, that’s a conversation that you want to have with your electrophysiologist. Arrhythmias are really one of the bigger deals. And although we can induce the V tach in the EP lab in about 30% of these folks, very rarely do we see ventricular tachycardia clinically.Many of them however will have frequent complex ventricular ectopy.So not unusual to see this.
By contrast, atrial arrhythmias are very common in this population. And an entity called IAPR [?] predominantly seen in patients with congenital heart disease.It tends to be a sort of fib-flutter hi-bred. And in patients with tetralogy of Fallot specifically Often is a wide complex tachycardia which is very difficult to distinguish from ventricular tachycardia.
Quick summary before we move on:
Tetralogy of Fallot: put the patient in the knee to chest position. Calm them down. Give high flow oxygen. Morphine. IV fluids. Ketamine if you need it. As they get older beware of arrhythmias. Most of them are atrial. Watch that QRS duration.
Let’s change gears just a little bit.
Next case six-year-old with a history of nausea vomiting and diarrhea for the last 24 hours. Mom says the kids not eating anything down. You got a sibling with norwich virus And mom is worried about this kid because she says, he had a Fontan because one part of his heart was bad. He takes aspirin every day And antibiotics before dental procedures. And on physical he too looks very bad. His heart rate is in the 120s. His SATs are in the 70s.His respiratory rate is in the 30s And he is ill appearing.Is mucous membranes dry. His eyes are sunken.He’s got poor pulses and poor capillary refill.And he is tachypneic.So what’s up with this patient.
So the kids blue which means he doesn’t have enough pulmonary blood flow. But in addition he has some signs of systemic hypoperfusion. More importantly to most of us is the question what does his heart looked like [what is a Fontan procedure].
The Fontan procedure was first done in 1971.It is the procedure of choice for children with functionally uni-ventricular hearts. And by that I mean kids who only have one ventricle that can work. There are a lot of complex variations that the cardiologists talk about but they are really just confusing to the rest of us and at the end of the day all these kids have fundamentally the same issue. And that is that only one of their ventricles works. This accounts for about 10% of complex congenital heart disease and it is something that you just are going to see [in your EM practice].
Dr. Fontan recognized that the one ventricle could not sustain the work up to ventricles. So he decided to create a circulation in which that ventricle had only one job to do and he gave it the job of systemic perfusion. He did that by making pulmonary blood flow passive. And here’s how that works. He connected the IVC and the SVC directly to the pulmonary artery bypassing the right ventricle completely And creating a pulmonary blood flow that is entirely passive. And the solo ventricle is responsible only for systemic flow.
The procedure is done in stages as the patient couldn’t tolerate the complete operation all at once. So first the SVC is connected to thePulmonary artery and then later the IVC is connected to the pulmonary artery.So by the time these children are 2 to 3 years of age that had the full Fontan procedure completed. And both SVC and IVC are connected to the pulmonary artery. And so pulmonary blood flow is passive. And systemic flow is the responsibility of that single ventricle.There are a bunch of different modifications of this procedure but you don’t really care because they are all fundamentally the same.
Survival of these children is shockingly good 85% twenty years postop. In some children we need to intervene before they’re ready for the first stage of the Fontan. Occasionally the patient will need a [?]. And Patients who have functionally only a right ventricle will need a procedure called the Norwood so that the ventricle can function as a systemic pump before the Fontan. But were not a to discuss that.
But there are some things about the Norwood procedure that we do need to know. First it is an incredibly unstable situation. These kids have a risk have a risk of sudden death as high as fifth 15% had any time. And number two is that they are incredibly sensitive to fluid and oxygen. It is easy to kill these children inadvertently.
So if you have a kid with a Norwood tread very carefully and get your pediatric cardiologist involved early. We’ll talk a little bit more about the nuances of that at the end.
Back to the Fontan. You can imagine that if you have a physiology that is completely passive there are some nuances that you have to be careful about. At the top of that list is this: if pulmonary blood flow is passive that means that that it is both volume and pressure dependent. These kids need adequate circulating blood volume and adequate blood pressure to maintain adequate forward flow. In real terms for us in the emergency department it means this: dehydration is bad. A dry Fontan is a dead Fontan they say. And that is because they cannot maintain pulmonary blood flow or cardiac output.Dehydrated Fontan will become increasingly hypoxic. If you rehydrate them and resuscitate them, their hypoxia will resolve.
Low blood pressure is also an issue because of forward flow and intrathoracic pressures are poorly tolerated by these patients at any time.That means that routine respiratory diseases can be a big issue for these kids. So be very cautious in your management and consider bringing them in for routine kinds of stuff.
It also means that when we have to intubate there are some things we need to consider. So we try if we can not to intubate these children because they do better with spontaneous respiration. But sometimes they’re just so sick that we have to do it and in those cases we should. But we have to keep in mind a couple of things. Intrathoracic pressure is bad which means you have to keep your peep low, typically not more than five. Keep your volumes low and your rates low to allow that pulmonary blood flow to happen. Low peep. Low volume. Low rate.
In addition when you are thinking about induction ketamine is your friend. Ketamine maintains hemodynamics and won’t get you in trouble like some other induction agents.
So what’s our management now for this case, this dehydrated Fontan? What do we want to do? Give him fluid! All of a sudden this case becomes a very easy.We give him some fluid and we give him some oxygen. Fully repaired Fontan’s like oxygen. And we admit him.
Unfortunately in a few months he comes back and he doesn’t feel well and he feels a little bit tired. [And he has an abnormal looking electrocardiogram which I can’t show] raise your hand if you think of this is a sinus rhythm. So this is that same arrhythmias the IAPR [?] that we talked about earlier. It is that fib-flutter kind of combination rhythm. It often occurs in patients with Fontan’s just like our tetralogy of Fallot. But unlike tet, in Fontan it is at a much slower rate often in the 90s or low 100s. And if the cycle length is fixed it can actually be very difficult to distinguish from a sinus rhythm. But it is important to make that distinction because they don’t tolerate arrhythmias very well for very long.
So you can look at congenital heart disease EKGs and it’ll make your eyes bleed because you have no idea what’s going on. Really the only question you need to ask and answer is is this sinus or not. Because if it’s not sinus rhythm then they will require some other interventions. Both tachy and brady arrhythmias are common in this population. And they are to risk for profound the hemodynamic deterioration if they are not handled in a timely manner.
It is common and 15 to 20% of these children will experience an arrhythmia by five years following their repair. Just like our tetralogy patients ventricular arrhythmias are fairly rare. Sinus node dysfunction is common so look out for junctional rhythms. Atrial arrhythmias especially this IART Is something you’re likely to see.
The good news is that your management is no different for arrhythmias that it is in any other population.
Be careful with calcium channel blockers and kids we don’t use them under a year of age because they are at risk of cardiovascular collapse.
Electricity if you needed. Kids do have an increased risk of thromboembolic disease kids do have cardiac thrombus. However, the stroke risk is still low and if there unstable you have to shock them.
Brady arrhythmias are the same thing. Atropine, epi, and pace them if you need to.
As they get older there are couple of other things that can happen. Thromboembolic disease is a real phenomenon for these patients. It occurs clinically in 3 to 20%. So keep your suspicions high if the clinical story fits or something that may be thromboembolic. Also the majority of these children will develop some degree of myocardial depression as they get older. And it may not be clinically apparent when you look at them. The reason that this is important is because it’s easy to volume overload them.
I just spent 10 min. telling you that you want to give fluid and now I’m saying this. You want to be judicious in your fluid use. Because you don’t want to tip them in the other direction.Our old 20 per kilo plan goes out the window. 10 per kilo should start for these kids. And go slowly but continue until you get to where you need to get.
We’re going to finish up with a little discussion of oxygen which is everybody’s favorite subject. And that’s because oxygen in congenital heart disease confuses all of us.
Keep in mind that when were talking about congenital heart disease were talking about children who have mixing lesions. Their oxygenated blood and their deoxygenated blood tend to live in the same place. And that balance that decides how much blood goes to the lungs and how much blood goes to the body is very tightly held. It is easy to push it out of whack.
If you vasodilate these kids pulmonary vasculature by giving them too much oxygen you can tip the balance so they get a lot of pulmonary blood flow at the expense of their systemic flow. So all at once you can drive them into pulmonary vasculature overflow and cardiovascular circulatory collapse. And obviously we don’t do that.
The first thing we need to talk about is what are these children’s normal sats anyway. Here’s a cheat sheet. As a general rule if the child has a shunt or a partially repaired complex lesion their SATs are between 75 and 85%. This includes your children with [?] shunts, your kids with Norwood’s or kids with central shunts which we didn’t talk about and kids who have undergone the first stage of the Fontan’s. Typically 75 to 85%.
Tetralogy of Fallot patients can be anywhere from 70 to 100% on room air. Many of them live in the 80s.
A child that has had the full Fontan’s completed typically lives with normal SATs 95 to 100%. However, as they get older that can start to drop.
Rules of thumb: ask the family and the patient what the kids normal SATs are. Typically, they are going to know. And if the kid lives at 70 then there is no reason for you to try to get him to 75. You’re probably going to make him worse and you probably not going to be able get in there.
Fontan fully repaired like oxygen. It relaxes their pulmonary vasculature and allows that it passive pulmonary forward slow. A fully repaired Fontan likes oxygen.
By contrast, those kids with the Norwood and something called central shunts are very oxygen sensitive and it is easy to pushing them towards pulmonary over circulation at the expense of their systemic circulatory flow. S0 be careful with those kids.
Last but not least are these neonates with newly diagnosed congenital heart disease that you’re going to start on prostaglandin. Be careful with them, the same thing you can cause pulmonary over circulation but also oxygen will hasten the closure of the ductus. So in general for those kids you want to aim for 85% or so.
At the end of the day when all of this fails you and you’ve got a sick kid in front of you and you can’t remember what the hell we talked about today, aim for 80 to 85%. It may not be ideal for for these kids but it’s unlikely to cause a big problem and will keep you from keeping them to hypoxic.
Fluid like we talked about, 10 per kilo and go slow.
That’s a lot so let’s summarize and move on.
Tetralogy of Fallot – Remember For the Tet spells knee to chest position, Calm them, high flow 02, morphine, saline,ketamine. Watch out for arrhythmias as they get older and keep a lookout for that wide QRS.
For most tet spells you can resolve them within a few minutes.Calm them, put them in needed chest, give them some oxygen, give them some fluid, and give them some morphine. And these things will resolve the problem in the majority of kids and if they don’t then your next step is ketamine. And if you’re still having trouble than you get innovate these kids. A lot of times needed chest and calming the kid is all it takes.
Fontan, this is a repair for the unit ventricular lesion, and pulmonary blood flow is passive. The IVC and SVC are directly connected to the pulmonary artery. That means that dehydration is bad and increased intrathoracic pressures are bad. Watch your peep, volumes, and your rates. As they get older keep a lookout for arrhythmias. These arrhythmias can be difficult to distinguish from sinus Rhythm. When in doubt shoot for 80 to 85% and 10 per kilo and go slow.