The following are some excerpts from A Practical Guide to Diagnosis, Management and Treatment of Testosterone Deficiency from the Canadian Urological Association (1):
Introduction
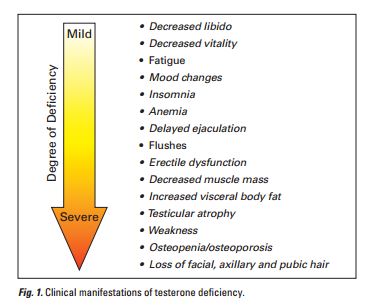
Testosterone deficiency syndrome (TDS), formerly termed andropause, is characterized by a deficiency in serum testosterone (T) levels with or without changes in receptor sensitivity to androgens. This syndrome is also variably referred to as hypogonadism or late-onset hypogonadism (LOH). There are various clinical manifestations of TDS (Fig. 1).
Detection and selective screening for TDS
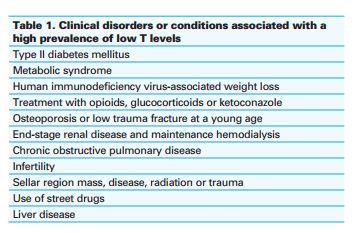
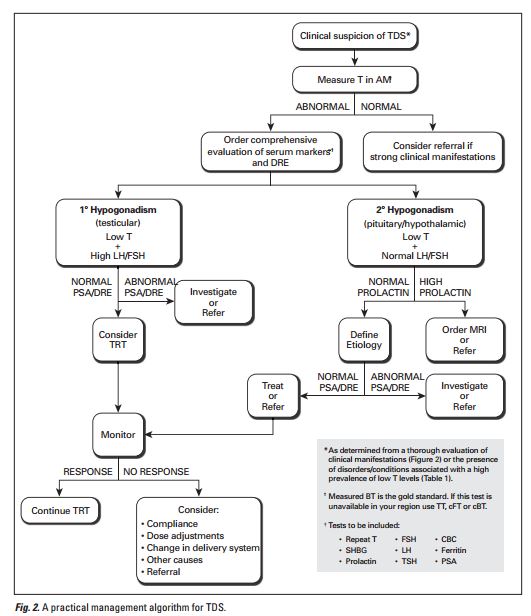
Effective management of TDS begins with an initial screening of high-risk men. A proportion of males with certain clinical disorders exhibit a high prevalence of low T levels (Table 1).1 The incidence of diabetes and T deficiency are directly correlated: 33% of men with diabetes have hypogonadism,13 and men with higher levels of T (15.6–21.0 nmol/L) have a 42% lower risk of type II diabetes.14 In particular, the Canadian Diabetes Association guidelines state that all men with diabetes should be screened for erectile dysfunction (ED), as 34% to 45% of men with diabetes have ED.15 The Endocrine Society guidelines also suggest that all men with Type II diabetes be screened for testosterone deficiency.1 Alternatively, patients may report symptoms consistent with TDS, such as fatigue, insomnia, decreased libido, reduced vitality, mood changes and ED.1,4 A thorough history and physical examination may reveal other clinical manifestations that are often consistent with the degree of T deficiency (Fig. 1).1,4,16,17 These manifestations may be present alone or in combination.
This guideline recommends using the Androgen Deficiency in the Aging Male Questionnaire (ADAM) for screening for testosterone deficiency . However, it is sensitive but not specific.
I prefer using both the Sexual Health Inventory For Men (SHIM) and The Aging Male Symptom Scale (AMS) in my patients for screening and for followup.
Diagnosis of TDS
Patients with symptoms suggestive of TDS require biochemical evaluation of serum T. Circadian rhythm influences T levels: higher T values are obtained in the morning.19 As a result, blood samples should be obtained between 7 and 11 am.4 Serum T circulates in a free or bound state. Most T is bound to either sex hormone-binding globulin (SHBG) (60%) or albumin (38%). Testosterone is tightly bound to SHBG, but weakly bound to albumin. Consequently, both albumin-bound T and free T (FT) are accessible to target tissues and constitute the bioavailable (BT) fraction that carries out the actions of T. Sex hormone-binding globulin-bound T is not biologically active. Generally, TDS manifestations correlate with the degree of T deficiency.16 The panel recognized measured BT as the gold standard for biochemistry. Additionally, the ammonium sulphate precipitation technique correlates well with symptoms of TDS.20 If measured BT is unavailable or unaffordable, calculated free T (cFT), calculated bioavailable T (cBT) or total T (TT) are acceptable alternatives.21 A free calculator for cFT and cBT is available online at the website for the International Society for the Study of the Aging Male (www.issam.ch). The calculated methods closely correlate with FT values obtained through laboratory assays, yet there are shortcomings: (1) SHBG levels vary up to twofold with different assays, and (2) aging and illness alter the binding characteristics of SHBG or serum. The panel has not defined cut-off values for normal T levels because of difficulties with equipment standardization and interlaboratory variability. Instead, it is recommended that physicians consistently use the same local laboratories and gain familiarity with the accuracy, precision and definition of normal values for the assays offered in their community.
For definitive diagnosis of hypogonadism, physicians should rule out other clinical conditions that may masquerade as TDS. For example, some symptoms of TDS are consistent with depression or hypothyroidism, the latter diagnosed through detection of elevated serum thyroidstimulating hormone (TSH). Measures of prolactin and ferritin can exclude hyperprolactinemia and hemochromatosis, respectively. Physicians should consider referral in patients with elevated prolactin levels. To exclude the possibility of pituitary/hypothalamic lesions, magnetic resonance imaging (MRI) should be performed in patients with very low levels of T and persistent hyperprolactinemia,24,25 or in patients with prolactin levels greater than 2 times the upper normal limit.26
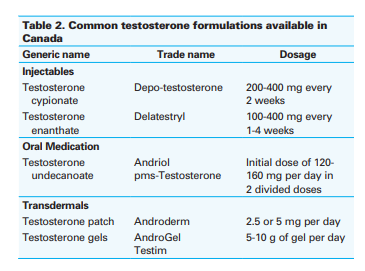
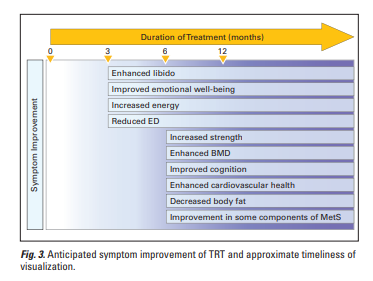
Benefits of TRT
Testosterone treatment has been shown to improve many of the symptoms of TDS and enhance overall health and potentially survival.41 Clinical studies indicate that T therapy enhances strength,42 sexual desire,43,44 energy,45 emotional well-being and cognition.45-47 Bone mineral density (BMD) is increased by T therapy in men with low T levels.48,49 Testosterone replacement therapy reduces body fat,50 enhances glycemic control in diabetic patients and may improve some components of MetS.8 Men with profound hypogonadism show significant improvement in ED when on TRT.35,51 Evidence is emerging that T may also improve cardiovascular health in hypogonadal men.9-11
Contraindications to TRT
Patients should be evaluated for other medical conditions that may lead to adverse events upon treatment. Testosterone therapy is absolutely contraindicated in men with breast or prostate carcinomas.1,4 Prior to initiation of T therapy, it is recommended that physicians measure the prostate-specific antigen (PSA) level and perform a digital rectal examination (DRE). Patients with abnormal PSA or DRE findings should be referred to a urologist for further evaluation. Testosterone therapy may also worsen other medical conditions, including erythrocytosis, untreated obstruc tive sleep apnea and severe congestive heart failure.50,52 Erythrocytosis can be revealed through a complete blood count (CBC). Testosterone replacement therapy is not suggested for men wishing biological fatherhood as T may reduce sperm production. Treatment with T in men with any of these medical conditions should not be initiated until these issues have been addressed.
Alternative treatments to TRT
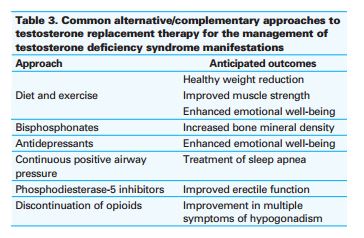
Occasionally, some testosterone deficiency manifestations
can be managed with reversal of an underlying cause, drug
therapy or lifestyle modifications (Table 3). Treatment of
sleep apnea,53 weight reduction54 and discontinuation of
opioid medication55 may improve manifestations of T deficiency.
Yet, the poor adherence to many of these regimens
(e.g., diet and exercise) makes T therapy a logical option.
Resources:
(1) A practical guide to diagnosis, management and treatment of testosterone deficiency for Canadian physicians [PubMed Abstract] [Full Text HTML] [Full Text PDF].
(2) 2015 CUA Practice guidelines for erectile dysfunction [PubMed Abstract] [Full Text HTML] [Full Text PDF].