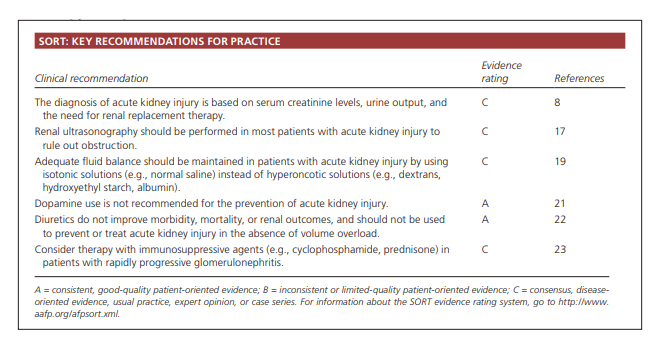
This post consists of excerpts from Resource (1), Acute kidney injury: a guide to diagnosis and management, and Resource (2), Management of Acute Kidney Injury.
Here are excerpts from Resource (1), Acute kidney injury: a guide to diagnosis and management:
Definition of Acute Kidney Injury
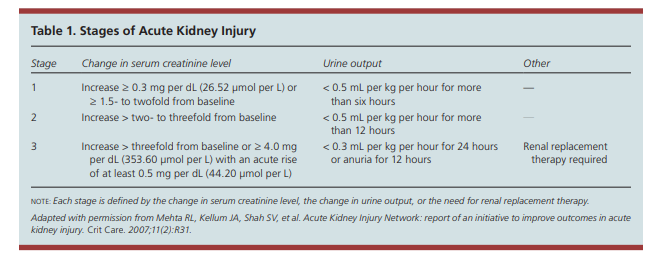
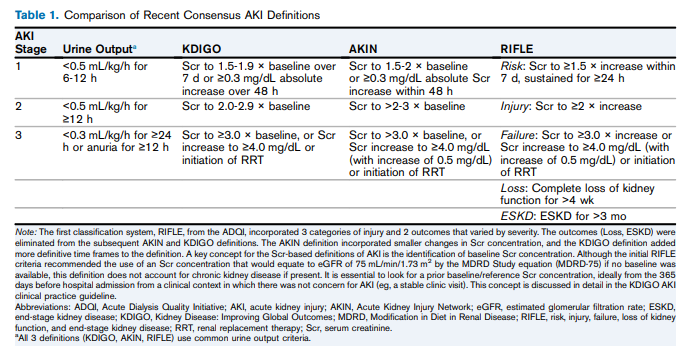
Acute kidney injury is defined as an abrupt (within 48 hours) reduction in kidney function based on an elevation in serum creatinine level, a reduction in urine output, theneed for renal replacement therapy (dialysis), or a combination of these factors. It is classified in three stages (Table 1). 8 The term acute kidney injury should replace terms such as acute renal failure and acute renal insufficiency, which previously have been used to describe the same clinical condition.
Causes
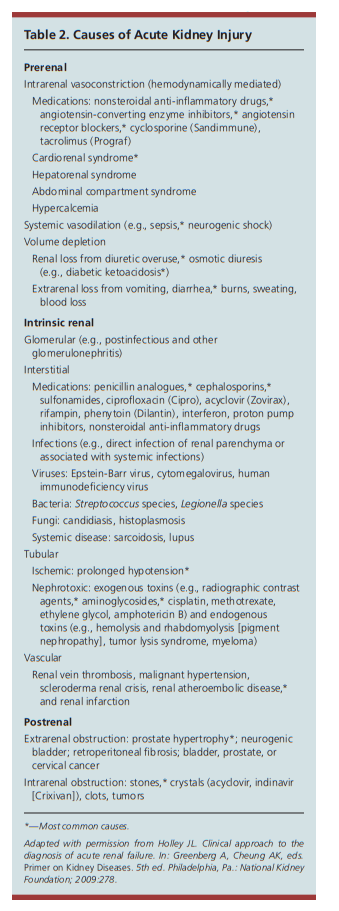
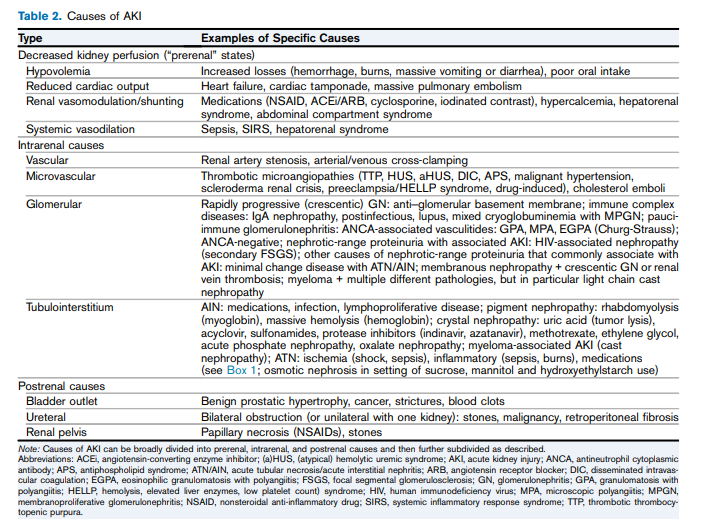
The causes of acute kidney injury can be divided into three categories (Table 2): prerenal (caused by decreased renal perfusion, often because of volume depletion), intrinsic renal (caused by a process within the kidneys), and postrenal (caused by inadequate drainage of urine distal to the kidneys). In patients who already have underlying chronic kidney disease, any of these factors, but especially volume depletion, may cause acute kidney injury in addition to the chronic impairment of renal function.
Clinical Presentation
Clinical presentation varies with the cause and severity of renal injury, and associated diseases. Most patients with mild to moderate acute kidney injury are asymptomatic and are identified on laboratory testing. Patients with severe cases, however, may be symptomatic and present with listlessness, confusion, fatigue, anorexia, nausea, vomiting, weight gain, or edema.15 Patients can also present with oliguria (urine output less than 400 mL per day), anuria (urine output less than 100 mL per day), or normal volumes of urine (nonoliguric acute kidney injury). Other presentations of acute kidney injury may include development of uremic encephalopathy (manifested by a decline in mental status, asterixis, or other neurologic symptoms), anemia, or bleeding caused by uremic platelet dysfunction.
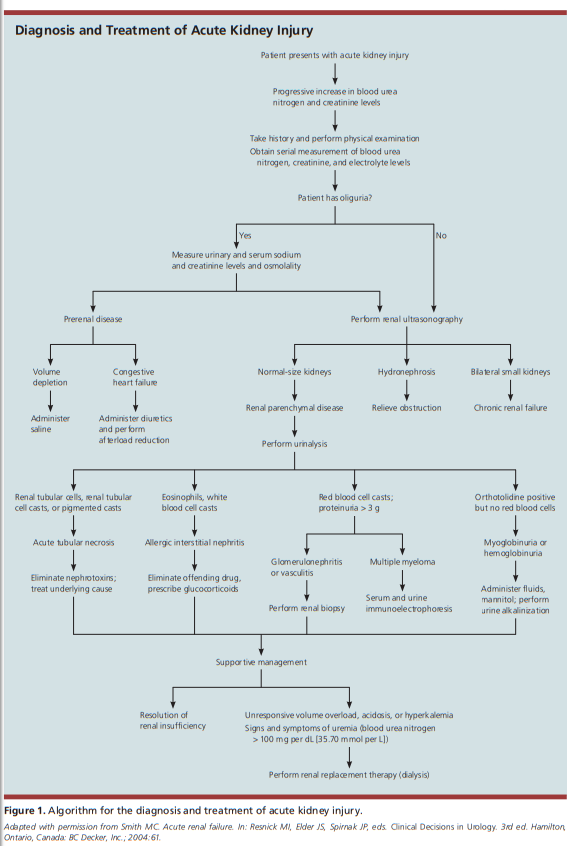
Diagnosis
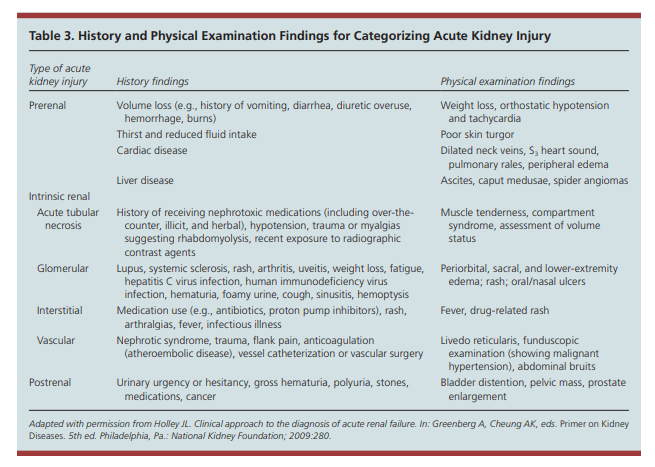
A patient history and physical examination, with an emphasis on assessing the patient’s volume status, are crucial for determining the cause of acute kidney injury(Table 3).
Here are excerpts from Resource (2), Management of Acute Kidney Injury:
Introduction:
Acute kidney injury (AKI) is a common diagnosis in hospitalized patients, often occurring in patients with multiple comorbid
conditions. It is associated with significant increases in both short- and long-term morbidity and mortality.Diagnosis And Evaluation Of AKI
AKI is characterized by the accumulation of creatinine, urea, and other unmeasured waste products after an abrupt decrease in kidney function. More recently, injury has replaced
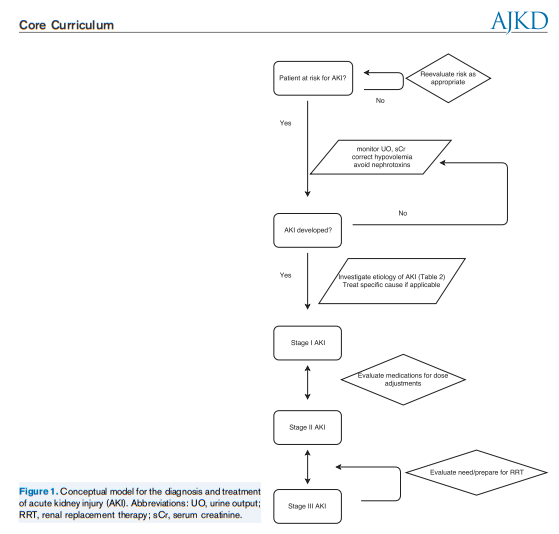
“failure” to emphasize the disease continuum because even modest reductions in kidney function are associated with worse outcomes. AKI is common, affecting approximately 5% to 10% of hospitalized patients and up to 60% of patients admitted to the intensive care unit (ICU).AKI has a variety of causes and should not be viewed as a single disease. Although some management strategies can be universally applied, others are disease specific.
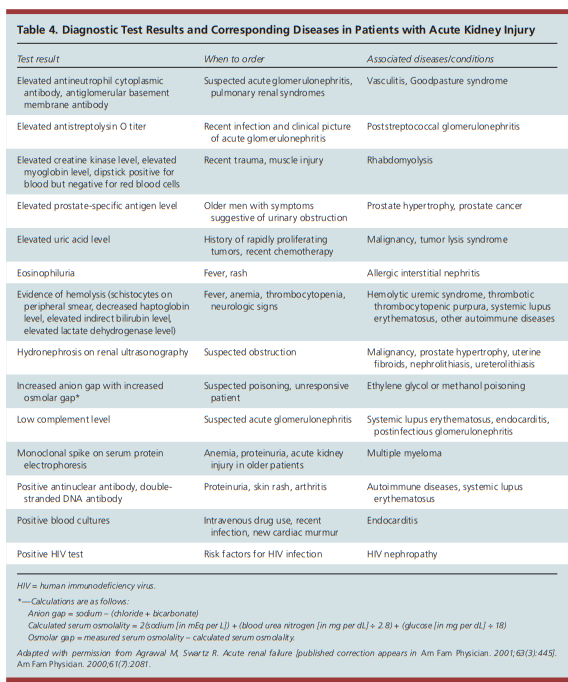
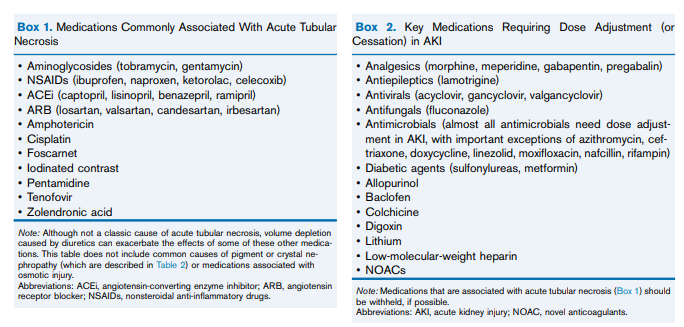
Thus, when AKI is recognized, a critical first step is the prompt evaluation for the cause of AKI, with special attention to reversible causes.Patients suspected of having a specific treatable intrarenal cause of AKI (such as acute interstitial nephritis [AIN], glomerulonephritis, or thrombotic microangiopathy) should have a urine sediment examination and serologic/hematologic tests, as indicated. A kidney biopsy should be considered when there is significant new proteinuria (protein excretion > 3 g/d) or hematuria, active urine sediment, or no readily identifiable cause of decreased kidney perfusion, obstruction, or ATN. A retrospective study of 68 critically ill patients who underwent kidney biopsy based on clinical suspicion found that 51% of patients had a specific cause of AKI, which led to a significant change in treatment plan in 21%. However, kidney biopsy was associated with complications in 22%, most commonly from bleeding.
Resources:
Acute kidney injury: a guide to diagnosis and management [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2012 Oct 1;86(7):631-9.
Management of Acute Kidney Injury: Core Curriculum 2018 [PubMed Abstract] [Full Text HTML] [Full Text PDF] American Journal Of Kidney diseases, 2018 Jul;72(1):136-148. doi: 10.1053/j.ajkd.2017.11.021. Epub 2018 Feb 22.
KDIGO Clinical Practice Guideline for Acute Kidney Injury [Full Text PDF]. VOLUME 2 | ISSUE 1 | MARCH 2012 https://www.kidney-international.org.