The flow chart of Resource (4) seems to be most in keeping with the spirit of the recommendations from Resource (1) [the most current recommendation].
Here are the latest recommendations on distal DVTs from Resource (1) Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report [Full Text HTML] [Full Text PDF]. Chest. 2016;149(2):315-352. doi:10.1016/j.chest.2015.11.026:
Whether and How to Prescribe Anticoagulants to Patients With Isolated Distal DVT
Summary of the Evidence
AT9 discouraged routine whole-leg US examinations (ie, including the distal veins) in patients with suspected DVT, thereby reducing how often isolated distal DVT is diagnosed.1,73 The rationale for not routinely examining the distal veins in patients who have had proximal DVT excluded is that: (1) other assessment may already indicate that isolated distal DVT is either unlikely to be present or unlikely to cause complications if it is present (eg, low clinical probability of DVT, D-dimer is negative); (2) if these conditions are not met, a repeat US examination of the proximal veins can be done after a week to detect possible DVT extension and the need for treatment; and (3) false-positive findings for DVT occur more often with US examinations of the distal compared with the proximal veins.1,73,74
If the calf veins are imaged (usually with US) and isolated distal DVT is diagnosed, there are two management options: (1) treat patients with anticoagulant therapy or (2) do not treat patients with anticoagulant therapy unless extension of their DVT is detected on a follow-up US examination (eg, after 1 and 2 weeks, or sooner if there is concern; there is no widely accepted protocol for surveillance US testing).75 Because about 15% of untreated isolated distal DVT are expected to subsequently extend into the popliteal vein and may cause PE, it is not acceptable to neither anticoagulate nor do surveillance to detect thrombus extension.1,76-79
In AT9, we judged that there was high-quality evidence that anticoagulant therapy was effective for the treatment of proximal DVT and PE, but uncertainty that the benefits of anticoagulation outweigh its risks in patients with isolated distal DVT because of their lower risk of progressive or recurrent VTE. We suggest the following as risk factors for extension of distal DVT that would favor anticoagulation over surveillance: (1) D-dimer is positive (particularly when markedly so without an alternative reason); (2) thrombosis is
extensive (eg, >5 cm in length, involves multiple veins, >7 mm in maximum diameter); (3) thrombosis is close to the proximal veins; (4) there is no reversible provoking factor for DVT; (5) active cancer; (6) history of VTE; and (7) inpatient status.1,75-77,80-84 We consider thrombosis that is confined to the muscular veins of the calf (ie,, soleus, gastrocnemius) to have a lower risk of extension than thrombosis that involves the axial
(ie, true deep; peroneal, tibial) veins.76,81,85 Severe symptoms favor anticoagulation, a high risk for bleeding
(Table 11) favors surveillance, and the decision to use
anticoagulation or surveillance is expected to be sensitive
to patient preferences. We anticipate that isolated distal
DVT that are detected using a selective approach to whole-leg US will often satisfy criteria for initial anticoagulation, whereas distal DVT detected by routine whole-leg US often will not.The updated literature search did not identify any new
randomized trials that assessed management of patients
with isolated distal DVT. Two new systematic
reviews76,77 and a narrative review83 addressed
treatment of isolated distal DVT. In addition to
summarizing available data, consistent with AT9, they
emphasize the limitations of available evidence. In the
absence of substantive new evidence, the panel endorsed
the AT9 recommendations without revision. The
evidence supporting these recommendations remains
low quality because it is not based on direct comparisons
of the two management strategies, and ability to predict
extension of distal DVT is limited.7. In patients with an isolated distal DVT of the leg provoked by surgery or by a nonsurgical transient risk factor, we suggest treatment with anticoagulation for 3 months over treatment of a shorter period (Grade 2C), we recommend treatment with anticoagulation for 3 months over treatment of a longer time-limited period (eg, 6, 12, or 24 months) (Grade 1B), and we recommend treatment with anticoagulation for 3 months over extended therapy (no scheduled stop date) (Grade 1B).
Remarks: Duration of treatment of patients with isolated distal DVT refers to patients in whom a decision has been made to treat with anticoagulant therapy; however, it is anticipated that not all patients who are diagnosed with isolated distal DVT will be prescribed anticoagulants.
13. In patients with acute isolated distal DVT of the leg and (i) without severe symptoms or risk factors for extension (see text), we suggest serial imaging of the deep veins for 2 weeks over anticoagulation (Grade 2C), and (ii) with severe symptoms or risk factors for extension (see text), we suggest anticoagulation over serial imaging of the deep veins (Grade 2C).
Remarks: Patients at high risk for bleeding are more likely to benefit from serial imaging. Patients who place a high value on avoiding the inconvenience of repeat imaging and a low value on the inconvenience of treatment and on the potential for bleeding are likely to choose initial anticoagulation over serial imaging
14. In patients with acute, isolated, distal DVT of the leg who are managed with anticoagulation, we recommend using the same anticoagulation as for patients with acute proximal DVT (Grade 1B).
15. In patients with acute, isolated, distal DVT of the leg who are managed with serial imaging, we (i) recommend no anticoagulation if the thrombus does not extend (Grade 1B), (ii) suggest anticoagulation if the thrombus extends but remains confined to the distal veins (Grade 2C), and (iii) recommend anticoagulation if the thrombus extends into the proximal veins (Grade 1B).
See my post Estimating The Risk of Bleeding From Anticoagulation Therapy July 5, 2017 for information on this topic from the above reference.
The following are excerpts from Resource (2):
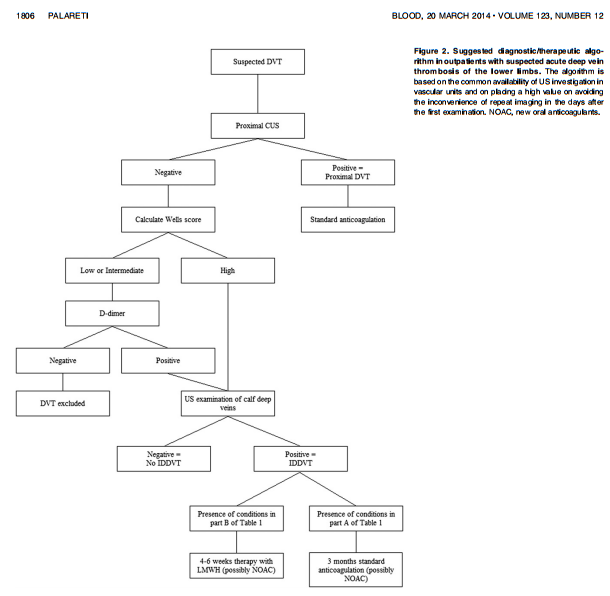
Thromboses limited to infrapopliteal leg deep veins (isolated distal deep vein thrombosis [IDDVT]) are frequently diagnosed in subjects with suspected pulmonary embolism or DVT and account for one-fourth to one-half of all diagnosed leg DVTs. Despite their frequency, the natural history of IDDVTs and their real risk of thromboembolic complications are still uncertain because of the scarcity of prospective, blind, nonintervention studies. Therefore it is still debated whether they warrant diagnosis and treatment. Diagnosis is based on ultrasonographic examination, which is more operator dependent and less sensitive in distal than in proximal veins. The available data seem to support the view that most IDDVTs are selflimiting and inconsequential for patients, though in some cases they can be associated with complications and warrant diagnosis and treatment. The available guidelines for treatment of IDDVTs give different indications ranging from serial imaging of the deep veins for 2 weeks to detect and treat only in case of proximal extension, to giving oral anticoagulation in all IDDVT patients for 3 months. I review this issue, focusing on possible and suggested treatments in symptomatic IDDVT patients, and describe our current therapeutic approach to these patients. (Blood. 2014;123(12):1802-1809)
The following chart is the way the author approaches distal DVTs:
In Resource (3) the author points out that there is no consensus in the various guidelines on the diagnosis and treatment of distal DVTs:
The treatment for ICDVT is even not mentioned at all by the National Clinical Guideline Centre (last published in June 2012)
since the guideline “…focused on proximal DVT rather than isolated calf vein DVT as the latter is less likely to cause postthrombotic syndrome than proximal DVT and also less likelyto embolize to the lungs.” (3). In contrast, the International Consensus Statement on prevention and treatment of VTE
affirms that evidence “…indicates that oral anticoagulants should be given to all patients with symptomatic isolated calf DVT and that three months seems to be sufficient.” (4). It is really evident that the diagnostic and therapeutic approaches
to suspected or diagnosed ICDVT vary greatly among guidelines as well as among even expert professionals and in clinical practice. This seems mainly attributable to the fact that the natural history of calf-limited DVTs, their potential risk and optimal treatment have, to date, not been sufficiently investigated. Thus, different options and clinical decisions are possible and equally justified.
The following excerpts are from Resource (4)
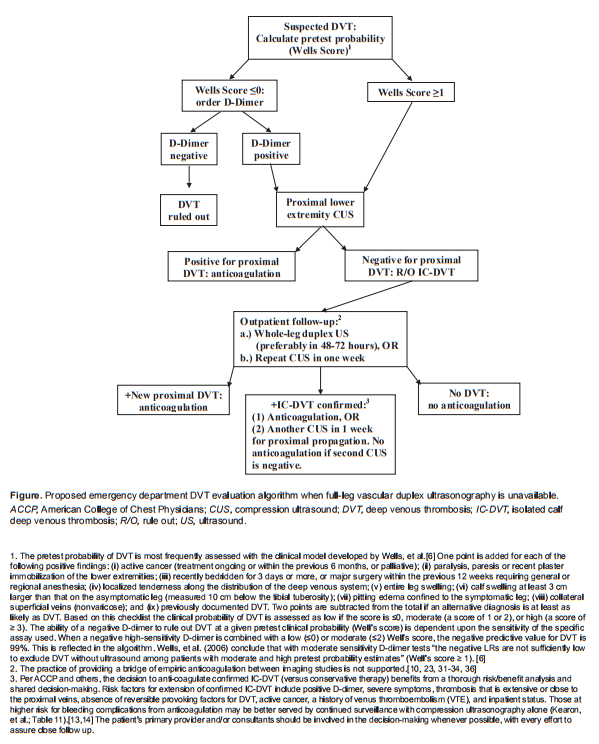
Introduction: Unilateral leg swelling with suspicion of deep venous thrombosis (DVT) is a common emergency department (ED) presentation. Proximal DVT (thrombus in the popliteal or femoral veins) can usually be diagnosed and treated at the initial ED encounter. When proximal DVT has been ruled out, isolated calf-vein deep venous thrombosis (IC-DVT) often remains a consideration. The current standard for the diagnosis of IC-DVT is whole-leg vascular duplex ultrasonography (WLUS), a test that is unavailable in many hospitals outside normal business hours. When WLUS is not available from the ED, recommendations for managing suspected IC-DVT vary. The objectives of the study is to use current evidence and recommendations to (1) propose a diagnostic algorithm for IC-DVT when definitive testing (WLUS) is unavailable; and (2) summarize the controversy surrounding IC-DVT treatment.
Discussion: The Figure combines D-dimer testing with serial CUS or a single deferred FLUS for the diagnosis of IC-DVT. Such an algorithm has the potential to safely direct the management of suspected IC-DVT when definitive testing is unavailable. Whether or not to treat diagnosed IC-DVT remains widely debated and awaiting further evidence.
Conclusion: When IC-DVT is not ruled out in the ED, the suggested algorithm, although not prospectively validated by a controlled study, offers an approach to diagnosis that is consistent with current data and recommendations. When IC-DVT is diagnosed, current references suggest that a decision between anticoagulation and continued follow-up outpatient testing can be based on shared decision-making. The risks of proximal progression and life-threatening embolization should be balanced against the generally more benign natural history of such thrombi, and an individual patient’s risk factors for both thrombus propagation and complications of anticoagulation. [West J Emerg Med. 2016;17(4)384-390.]
For the Wells Score see “DVT Probability: Wells Score System” From Medscape
Posted on July 2, 2017 and here is the flow chart for Resource (4)
(1) Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report [Full Text HTML] [Full Text PDF]. Chest. 2016;149(2):315-352. doi:10.1016/j.chest.2015.11.026
(2) How I treat isolated distal deep vein thrombosis (IDDVT). [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Blood. 2014 Mar 20;123(12):1802-9. doi: 10.1182/blood-2013-10-512616. Epub 2014 Jan 28.
Here are two similar articles that cite the above article:
(3) Do isolated calf deep vein thrombosis need anticoagulant treatment? Palareti G.J Thorac Dis. 2016 Dec;8(12):E1691-E1693. doi: 10.21037/jtd.2016.12.93. No abstract available.PMID: 28149615 [Full Text HTML] [Full Text PDF]
(4) Emergency Department Management of Suspected Calf-Vein Deep Venous Thrombosis: A Diagnostic Algorithm. Kitchen L, Lawrence M, Speicher M, Frumkin K. West J Emerg Med. 2016 Jul;17(4):384-90. doi: 10.5811/westjem.2016.5.29951. Epub 2016 Jun 28. Review. [PubMed Abstract] [Full Text HTML] [Full Text PDF]