Be sure and also check out Resource (5) European Society of Cardiology Clinical Practice Guidelines.
The following are excerpts, text and slides, from Resource (1):
Part I – A Sensible Approach to Sensitive Troponin [Video] [Transcript]Authors:
James L. Januzzi, MD; W. Frank Peacock, MD; and Robert H. Christenson, PhD CME / ABIM MOC / CE Released: 4/17/2017
[I do these posts because in this way I can rapidly review the topic.]:
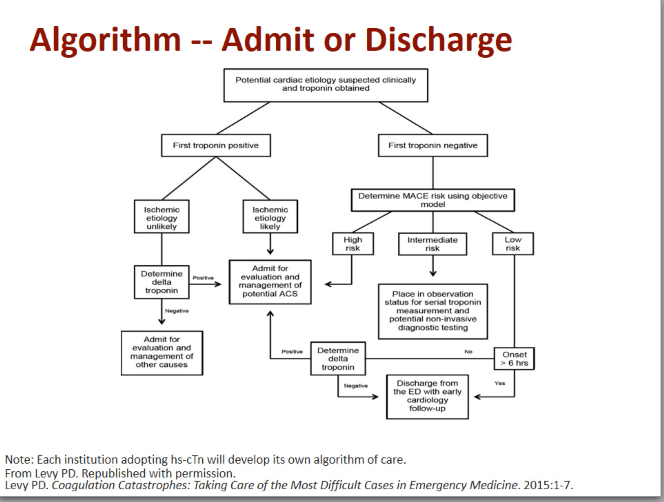
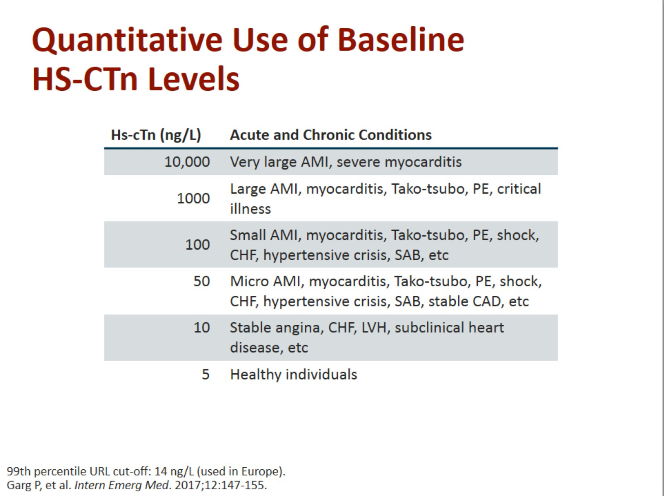
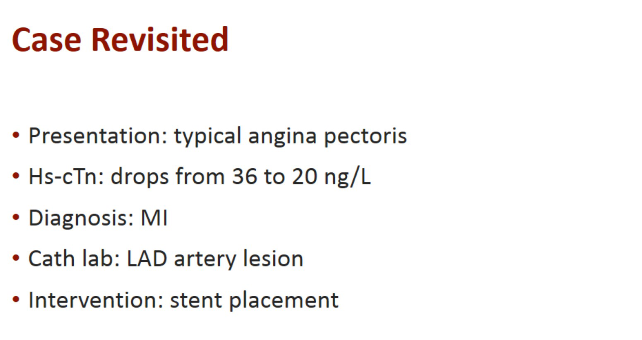
Basically the slide below sums up the topic of using the high-sensitivity cardiac troponin (hs-cTn) assays:
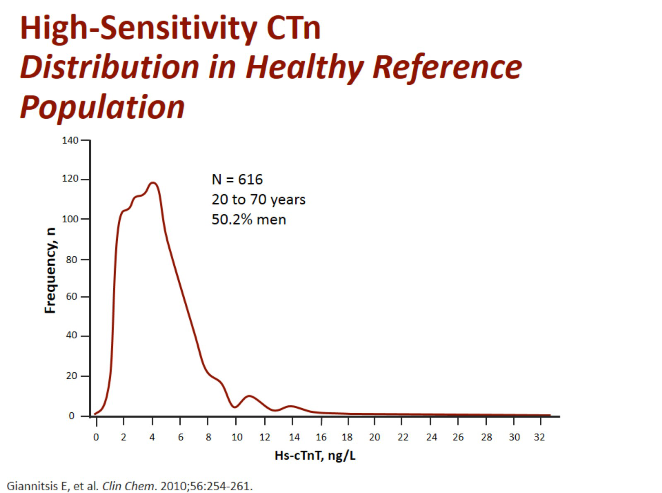
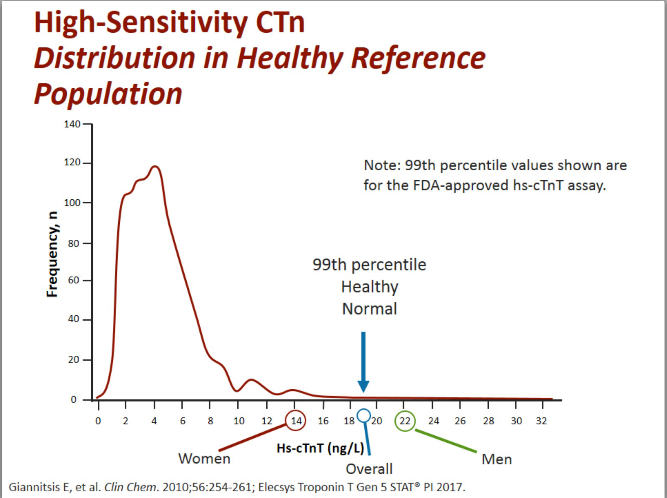
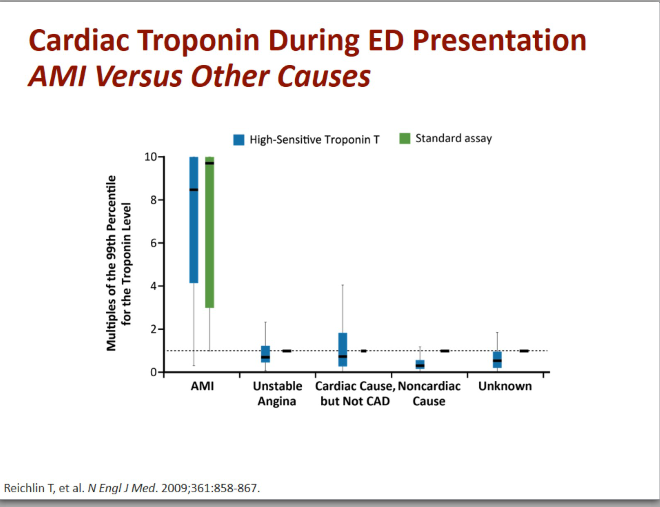
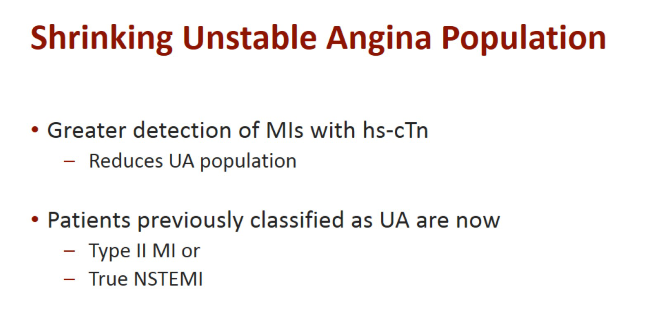
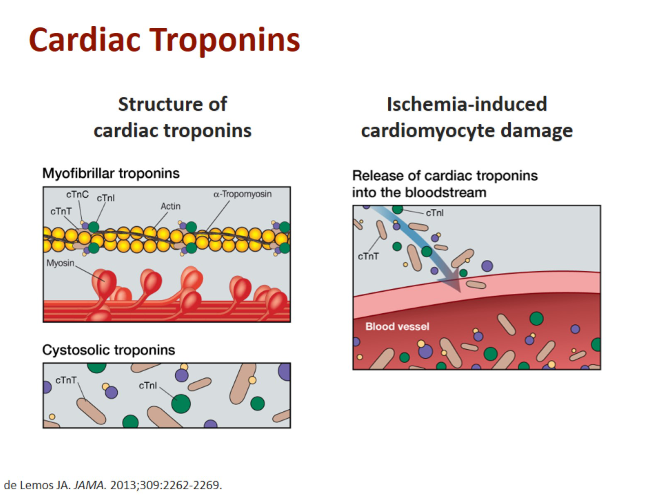
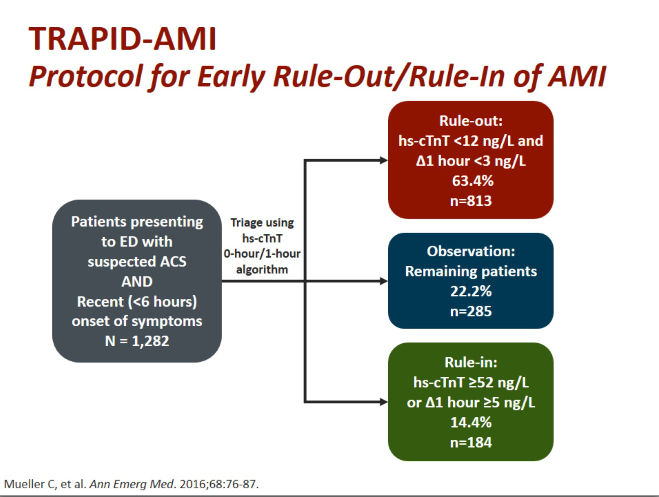
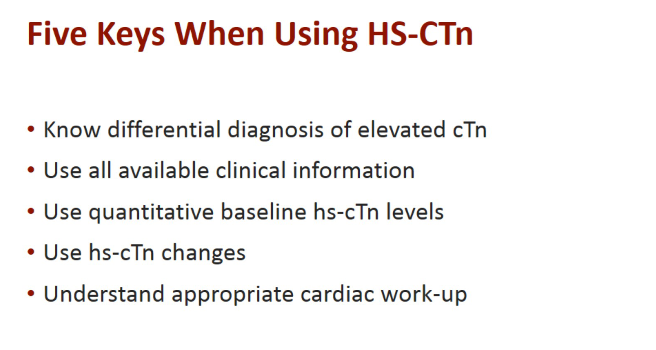
The greater sensitivity and precision of high-sensitivity cardiac troponin (hs-cTn) assays allows more precise detection of rise/fall of cardiac troponin (cTn) levels, which in turn allows for the earlier detection of AMI. Hs-cTn assays also have a high negative predictive value of more than 99%, which allows the safe ruling out of AMI. Hs-cTn values should not be used in isolation for the diagnosis of AMI. According to the third universal definition of AMI, diagnosis requires a rise and/or fall of cTn values in conjunction with one of the following: symptoms of ischemia; electrocardiography (ECG) changes; left bundle branch block; as well as imaging evidence of viable myocardium loss, wall motion abnormality, or intracoronary thrombus.
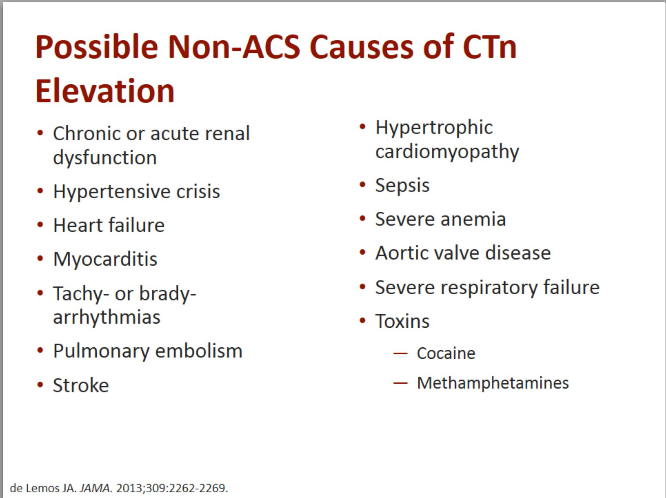
Patients with a positive cTnT, regardless of the cause, are at increased risk for adverse events and discharging [these patients to] home is not recommended. [When] there is no rise or fall noted on serial measurement, admission to evaluate for other causes is most appropriate. Cardiac catheterization may be warranted at some point in [a] patient’s care if alternative causes are not found, but anchoring on ACS as the etiology of the troponin elevation could lead to misdiagnosis. After the first 6 hours, further cTnT testing is of limited diagnostic or prognostic value and should be avoided.
t
t
t
t
Type II MI is an MI not due to plaque rupture but rather to demand imbalance [See Resource (4) below]:
Type 2 MI is defined as “myocardial infarction secondary to ischaemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anaemia, arrhythmias, hypertension or hypotension.”
The definition of type 2 MI is unsatisfactory because it is not really defined by what it is but rather what it is not.6 Nevertheless, the clinical problem remains: to distinguish acute MI (associated with plaque rupture or erosion, traditional or type 1 MI)—for which there is evidence-based treatment—from acute secondary ischaemic cardiac injury, including type 2 MI, where such treatments are not evidence based and may even be harmful.
t
t
t
t
t
t
t
t
Resources:
(1) Part I – A Sensible Approach to Sensitive Troponin [Video] [Transcript]Authors:
James L. Januzzi, MD; W. Frank Peacock, MD; and Robert H. Christenson, PhD CME / ABIM MOC / CE Released: 4/17/2017
(2) Part II: It Takes a Team — Incorporating High Sensitivity Troponin Into Clinical Care
Authors: James L. Januzzi, MD; Peter Kavsak, PhD; Robert H. Christenson, PhD; Ali Tann, BSN, RN, CEN CME / ABIM MOC / CE Released: 5/1/2017
(3) Part III Lessons Learned: A Master Class in High-Sensitivity Troponin: A Global Perspective Authors: James L. Januzzi, MD; Christian E. Mueller, MD; W. Frank Peacock, MD; Richard Body, MBChB, PhD
Faculty and Disclosures
CME / ABIM MOC / CE Released: 5/15/2017
(4) Diagnosing Type 2 Myocardial Infarction May 18, 2016 | Paul Collinson, MD; Bertil Lindahl, M.D., Ph.D. Expert Analysis
(5) European Society of Cardiology Clinical Practice Guidelines