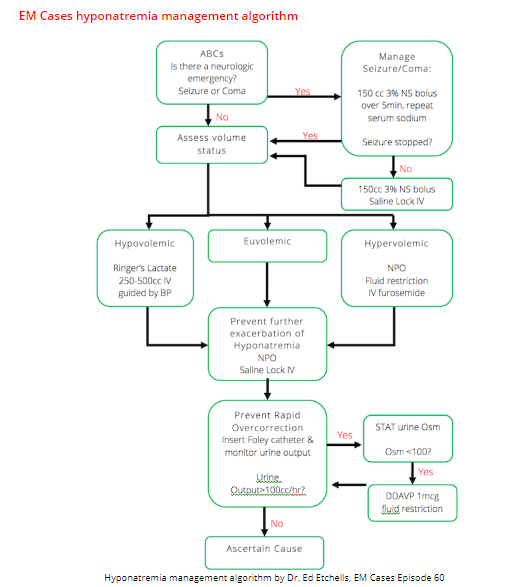
[Note to myself: After reading the show notes for Critcases 10, be sure to listen to podcast and review the show notes of Emergency Medicine Cases Episode 60: Emergency Management of Hyponatremia.]
The following excerpts are from the beginning of the outstanding CritCases 10 Hyponatremia Associated Seizures, June 2018, from Emergency Medicine Cases:
In this EM Cases CritCases blog – a collaboration between STARS Air Ambulance Service, Mike Betzner and EM Cases, a middle aged woman presents to a rural ED with headache and vomiting, normal vital signs with subsequent status epilepticus and serum sodium of 110 mmol/L. What management recommendations would you make to the rural ED physician, the transport team and in your ED with regards to treatment of seizures, safe correction of hyponatremia, airway management, search for underlying cause and prevention of Osmotic Demyelenation Syndrome?
Written by Jim Brokenshire; Edited by Michael Misch & Anton Helman June 2018
Clinical Case
A 52 year old female is brought by car to a rural ED, presenting with gradual onset worsening generalized headache, nausea and vomiting over the past 4 days. According to her husband, she became increasingly confused over the past 4 hours. Her only sick contact is her daughter with sore throat, and she has not recently travelled.
Past medical history is notable for febrile seizure as an infant. She is on no medications.
Triage Vitals are stable: Temp 35.6, HR 85, BP 127/79, RR 17, SpO2 100% on 2L NP, BG = 9.7, weight = 60kg.
While finishing the triage registration process she has a focal right sided tonic/clonic seizure lasting 1 minute. She is subsequently post-ictal with a GCS of 6 and is brought into the resuscitation bay. Shortly thereafter, she begins to seize again…
What is the differential diagnosis and initial management?
The differential at this point is quite broad. The presentation of progressive headache, vomiting, and altered mental state (and now status epilepticus) should prompt consideration of
- intracranial hemorrhage or mass
- meningitis or encephalitis
- toxicological or metabolic cause
The presence of a sick contact suggests a potential infectious etiology.
Initial management should consist of basic airway maneuvers and establishment of intravenous lines. A capillary glucose is a must – in this case it was initially 9.7 mmol/L. Benzodiazepines are first-line for treatment of status epilepticus..
She is given lorazepam 4 mg IV and the seizure terminates. She remains altered and postictal. A transfer via ground EMS to a tertiary care centre is requested.
If you didn’t have an IV you could and maybe should give IM midazolam. See Dr. Farkas post on Status Epilepticus. Here is what he says:
For patients without intravenous access, evidence supports a dose of 10 mg intramuscular midazolam. The RAMPART study found that up-front intramuscular midazolam was more effective than first attempting to get IV access and then giving IV lorazepam.
Returning now to CritCases 10 Hyponatremia Associated Seizures:
As the consulting transfer physician, what are your next steps to facilitate safe transport of this patient? [This link takes you to CritCases 10 where you’ll finish reviewing the show notes.]