In addition to the article below, please also review the excellent article, (1) Causes and Evaluation of Chronic Dyspnea [PubMed Abstract] [Full Text PDF]. Am Fam Physician. 2012 Jul 15;86(2):173-82.
The article, Interpreting pulmonary function tests: recognize the pattern, and the diagnosis will follow [PDF], is an excellent short review of the the interpretation of pulmonary function tests (PFTs) including the diffusion lung capacity.
There is one serious weak point in the above article. The article does not include the spirometric normal values that are necessary for PFT interpretation.
However, the commercial website, vitelograph.com, has the needed spirometry normal values.
What follows are extracts from the above article:
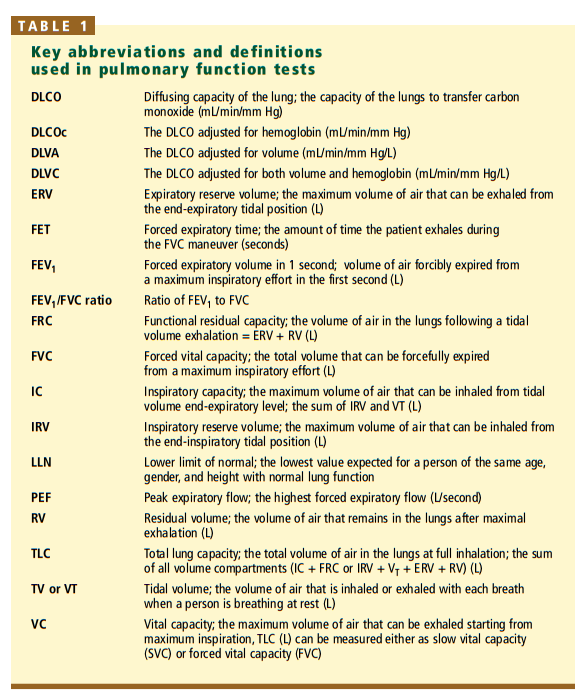
KEY POINTS
- Every clinician should have an organized approach to interpreting pulmonary function tests that will allow him or her to recognize and quantitate abnormalities.
- Before interpreting the results, one should ascertain that the test was acceptable and reproducible and that the patient’s demographic data are correct.[
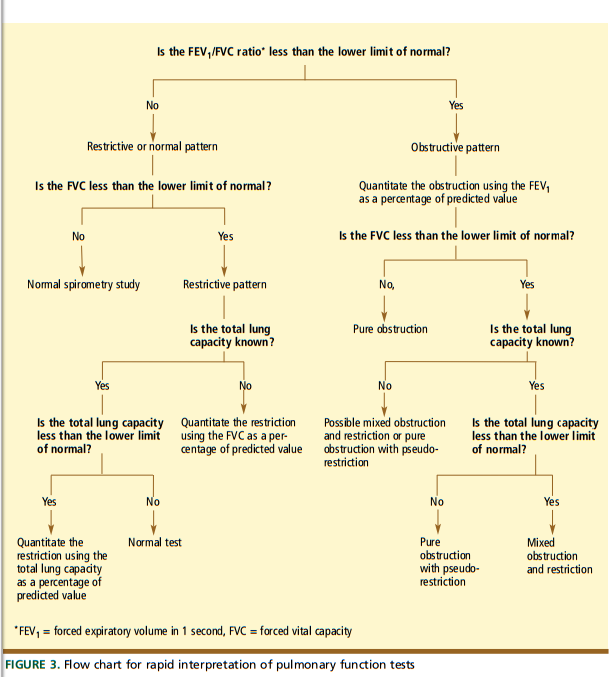
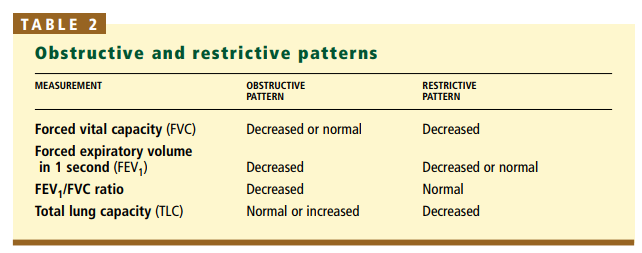
- Pattern recognition is key. A low FEV1/FVC ratio (the forced expiratory volume in 1 second divided by the forced vital capacity) indicates an obstructive pattern, whereas a normal value indicates either a restrictive or a normal pattern. If the FEV1/FVC ratio is normal, a low forced vital capacity value indicates a restrictive pattern, whereas a normal value indicates a normal pattern.
- Pulmonary function tests are not generally indicated in patients without symptoms, and they may be confusing when nonpulmonary diseases that affect the pulmonary system are active (eg, congestive heart failure).
The three most important measures are the:
• FVC
• FEV1
• FEV1/FVC ratioThe FEV1/FVC ratio is used to determine if the pattern is obstructive, restrictive, or normal.
If the FEV1/FVC ratio is low, an obstructive defect is present.
Pulmonary function testing pearl: Distinguish a mixed pattern vs air trapping
Once you have determined that the spirometry data are compatible with obstruction and you have quantitated the degree of obstruction on the basis of the FEV1 percent of predicted, you should look at the FVC.
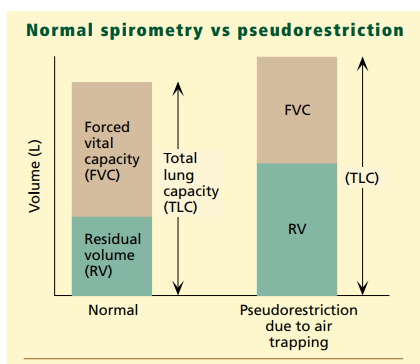
If the FVC is less than the lower limit of normal, then two possibilities exist. The first is that there is a mixed pattern with both an obstructive and a restrictive component. The second is that the obstruction is very severe and has led to significant air trapping.
Air trapping will increase the residual volume so that it takes up a greater percentage of the total lung capacity. If the residual volume increases enough, it will encroach on the air in the lung that can be exhaled and may lower the FVC below the lower limit of normal. This spirometry pattern is known as pseudorestriction (FIGURE 4 -Below).
To distinguish between these two possibilities, measure the residual volume and total lung capacity. If there is a mixed pattern with obstructive and restrictive components, the total lung capacity will be decreased. If air trapping is the cause of the low FVC, then the total lung capacity will be normal or elevated and the residual volume will be significantly increased.
For information on how to measure Residual Volume, see Resource (2) below. What follows is a brief extract from that article:
How the measurement of lung volume is derived
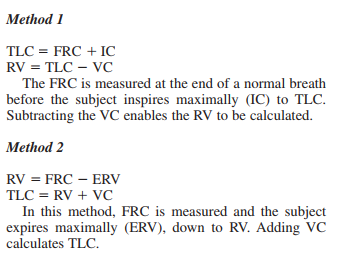
As it is impossible to exhale all the gas from the lungs we cannot make a direct measurement of RV and TLC. These values may be derived by first measuring the FRC using one of three commonly used indirect techniques [helium dilution, nitrogen washout, and body plethysmography]. Once the FRC is measured, a simple calculation may be used to calculate TLC and RV.
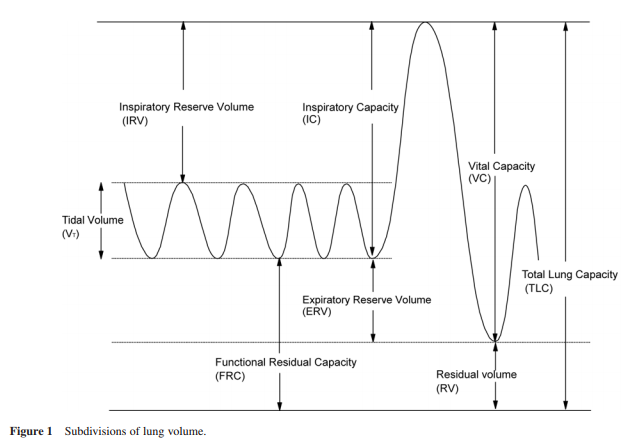
Referring to the spirometry trace shown in Figure 1, TLC and RV may be calculated as follows:
Returning now to extracts from the article Interpreting pulmonary function tests – recognize the pattern, and the diagnosis will follow [PDF]:
Pulmonary function testing pearl: Distinguish parenchymal vs extraparenchymal causes of restriction
A restrictive pattern seen on pulmonary function
testing may be due to causes inside or outside
the lung parenchyma.Pulmonary parenchymal causes include diseases such as pulmonary fibrosis, in which abnormalities of the lungs themselves result in restriction. Extraparenchymal causes of
restriction include obesity, neuromuscular diseases, chest wall deformities, and large pleural effusions, which may impair a person’s ability to fully inflate the lungs.The diffusing capacity of the lungv(DLCO) can be used to distinguish between these categories. If the DLCO is still below the lower limit of normal after being adjusted for the lung volume (ie, the DLVA), hemoglobin level (ie, the DLCOc), or both (ie, the DLVc), then parenchymal disease is likely. If normal, it
suggests that the cause of restriction is extraparenchymal.
Resources:
(1) Interpreting pulmonary function tests: recognize the pattern, and the diagnosis will follow [PubMed Abstract] [Full Text PDF]. Cleve Clin J Med. 2003 Oct;70(10):866, 868, 871-3, passim.
(2) REVIEW SERIES: Lung function made easy – Assessing lung size [PubMed Abstract] [Full Text PDF]. Chron Respir Dis. 2007;4(3):151-7.
(3) Causes and Evaluation of Chronic Dyspnea [PubMed Abstract] [Full Text PDF]. Am Fam Physician. 2012 Jul 15;86(2):173-82.