In this post I link to and excerpt from Core EM‘s Episode 173.0 – Blunt Neck Trauma, November 2019. Hosts: Audrey Bree Tse, MD and Brian Gilberti, MD.
In addition to the above please review my post Core EM’s Outstanding Minicourse on Cervical Spine Injuries. That post is simply a list of Core EM’s great resources on the subject so that I can do a rapid review when I need to.
Here are excerpts from Episode 173.0 [Note to my readers: I recommend listening to the entire podcast and reviewing the complete show notes. I excerpt the notes simply because it helps me fix the information in my memory.]:
Show Notes
Overview
- Blunt neck trauma comprises 5% of all neck trauma
- Mortality due to loss of airway more so than hemorrhage
Mechanism
- MVCs with cervical hyperextension, flexion, rotation during rapid deceleration, direct impact
- Strangulation: hanging, choking, clothesline injury (see section on strangulation in this chapter)
- Direct blows: assault, sports, falls
Initial Management/Primary Survey
- Airway
- Evaluate for airway distress (stridor, hoarseness, dysphonia, dyspnea) or impending airway compromise
- Early aggressive airway control: low threshold for intubation if unconscious patient, evidence of airway compromise including voice change, dyspnea, neurological changes, or pulmonary edema
- Assume a difficult airway
- Breathing
- Supplemental oxygen
- Assess for bilateral breath sounds
- Can use bedside US to evaluate for pneumothorax or hemothorax
- Circulation
- Assess for open wounds, bleeding, hemorrhage
- IV access
- Disability
- Maintain C-spine immobilization
- Calculate GCS
- Look for seatbelt sign
Types of Injuries
- Vascular injury
- Overview
- Carotid arteries (internal, external, common carotid) and vertebral arteries injured
- Mortality rate ~60% for symptomatic blunt cerebral vascular injury
- Mechanism
- Hyperextension and lateral rotation of the neck, direct blunt force, strangulation, seat belt injuries, and chiropractic manipulation
- Morbidity due to intimal dissections, thromboses, pseudoaneurysms, fistulas, and transections
- Clinical Features
- Most patients are asymptomatic and do not develop focal neurological deficits for days
- if Horner’s syndrome, suspect disruption of thoracic sympathetic chain (wraps around carotid artery)
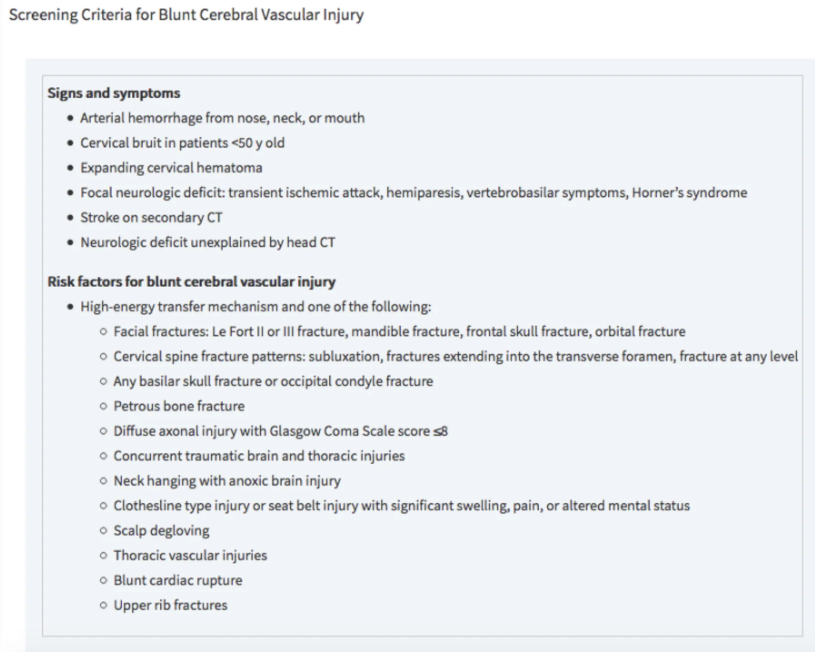
- specific screening criteria are used to detect blunt cerebrovascular injury in asymptomatic patients (see below)
Tintinalli 2016
- Diagnostic Testing
- Gold standard for blunt cerebral vascular injury = MDCTA (multidetector four-vessel CT angiography)
- <80% sensitive but 97% specific
- Also images aerodigestive tracts and C-spine (unlike angiography)
- Followed by Digital Subtraction Angiography (DSA) for positive results or high suspicion
- Angiography is invasive, expensive, resource-intensive, and carries a high contrast load
- Management
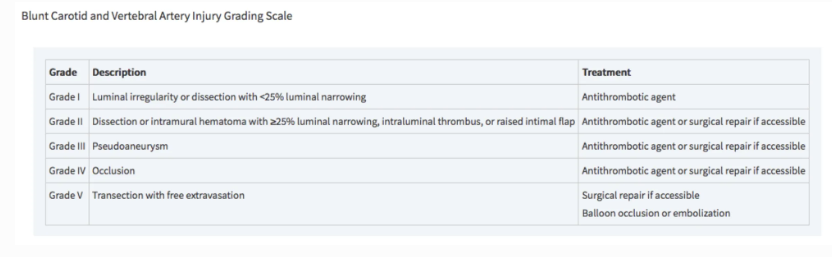
- Antithrombotics vs. interventional repair based on BCVI grading system
- Involve consultants early: trauma surgery, neurosurgery, vascular surgery, neurology
- All patients with blunt cerebral vascular injury will require admission
Tintinalli 2018
- Pharyngoesophageal injury
- See show notes for detailed instructions on evaluation.
- Diagnostic Testing
- Esophagography with water-soluble contrast (e.g. Gastrograffin)
- If negative contrast esophagography, obtain flexible endoscopy (most sensitive)
- Combination of contrast esophagography + esophagoscopy has sensitivity close to 100%
- Swallow studies with water-soluble agent
- MDCTA
- Plain films of neck and chest
- Findings such as pneumomediastinum, hydrothorax, or retropharyngeal air may suggest perforation but are not sensitive
- Management
- See show notes for instructions on management.
- Laryngotracheal injury
- Overview
- Occurs in >0.5% of blunt neck trauma
- Includes hyoid fractures, thyroid/ cricoid cartilage damage, cricotracheal separation, vocal cord disruption, tracheal hematoma or transection
- Mechanism
- Assault, clothesline injuries, direct blunt force from MVCs compressing the larynx between a fixed object and the spine
- Clinical Features
- Patients are often asymptomatic at first and then develop airway edema and/or hematoma resulting in airway obstruction
- Children are at higher risk for airway compromise due to less cartilage calcifications
- Diagnostic Testing
- Flexible fiberoptic laryngoscopy (FFL) to assess airway patency and extent of intraluminal injury
- MDCTA
- Obtain 1-mm cuts of larynx and perform multiplanar reconstructions
- Consider POCUS to detect laryngotracheal separation
- Plain films of neck and chest
- Poor sensitivity for penetrating neck trauma injuries
- Can show extraluminal air, fracture or disruption of cartilaginous (e.g. larynx) structures
- Management
- When securing airway, use an ETT that is one size smaller due to likelihood of airway edema
- Conservative management (IV antibiotics, steroids, observation) vs. surgical repair
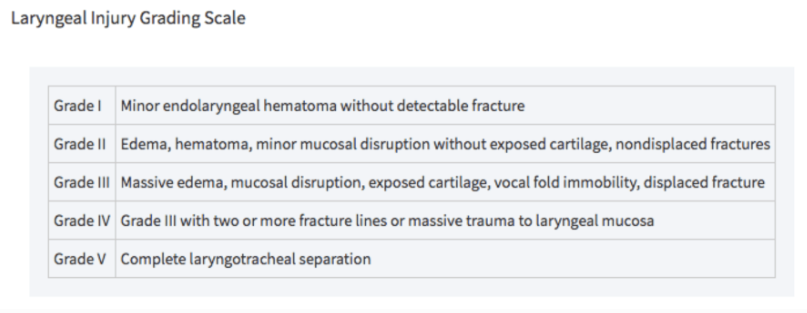
- Grades III, IV, and V laryngotracheal injuries as defined by Schaefer and Brown’s classification system require OR
- Cervical spine/ spinal cord injury
- See chapter for spinal trauma
- See my post Core EM’s Outstanding Minicourse on Cervical Spine Injuries
Posted on February 27, 2020 by Tom Wade MD
- My post is simply a list of Core EM’s great resources on the subject so that I can do a rapid review when I need to.
Disposition
- Admit symptomatic patients to monitored setting
- Given delayed symptoms, consider monitoring patients who are asymptomatic on arrival
- Serial exams for worsening dyspnea, dysphonia, stridor, drooling, bruits, focal neuro deficits
- Only discharge after ruling out airway threat, neurological deficit, vascular injury, or suicidal/ homicidal ideation
- Monitor asymptomatic patients on home anticoagulation in ED for at least 6 hours from trauma to rule out delayed neck hematoma
- Social work and/or psychiatry for patients in whom you suspect suicide risk or domestric violence, look for other signs of self harm