In this post, I link to and embed Dr. Josh Farkas‘ PulmCrit YouTube video, 10 minute talk on hypoxemia physiology, Sept. 8, 2021, from
I recommend that you watch Dr. Farkas lecture on YouTube [link is to the YouTube video] because, on the YouTube video, you can follow along with the excellent autogenerated transcript.
All that follows is from the above resource.
Here is a 10-minute video I [Dr. Josh Farkas] made for the Cooper Critical Care Conference. It explores some basic & useful concepts about hypoxemia physiology, including how to apply this at the bedside. The algorithms in the video aren’t intended to be strictly followed, but rather merely as general conceptual schemas.
related
What follows are some screenshots from Dr. Farkas’ YouTube video with accompanying text from the autogenerated YouTube transcript. I do this just because it helps me remember the material. Readers of this blog should go to the YouTube video and watch it and follow along with the autogenerated text on the YouTube site.
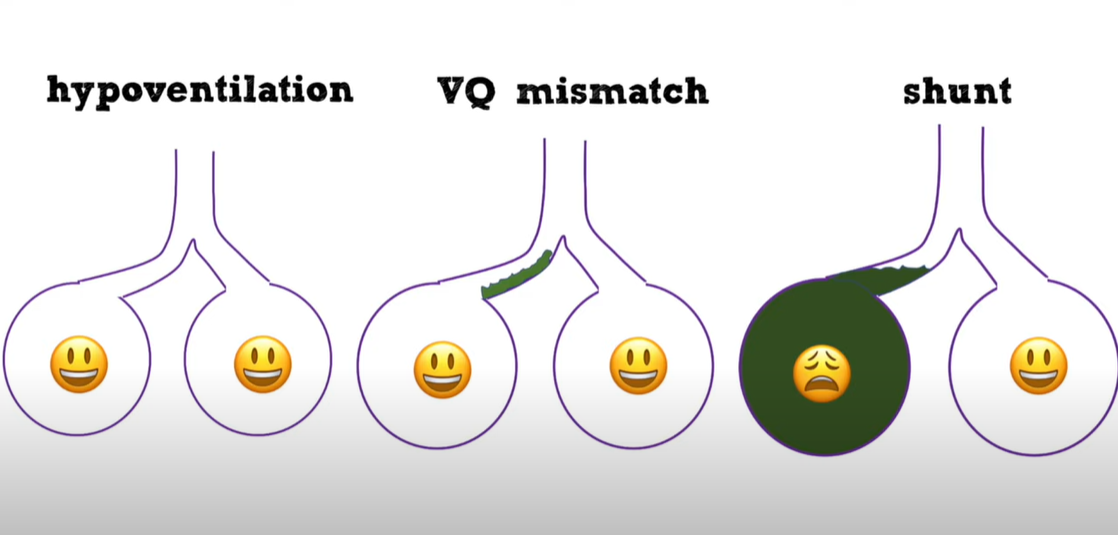
00:22-00:28There are only really three mechanismsof hypoxemia that you need to worryabout: hypoventilation, vq mismatch, andshunting.
00:28-02:38Shunting in hypoventilation the alveoliand the bronchi are working perfectlyand the problem is simply there’s notenough ventilation getting to the lungso the alveoli are burning throughoxygen faster than they’re gettingoxygen probably the most commonlyencountered cause of hypoventilation isa central brain drive problem where thebrain is simply not stimulating the body00:48to breathe and we’re most familiar with00:50this probably in the context of opioid00:52intoxication so folks come in their00:53respiratory rate is low they’re00:55substantially altered they’re not00:56breathing this is relatively easy to00:58diagnose other causes of central01:00hypoventilation are folks with brain01:02stem strokes or substantial brain01:04pathology and once again relatively01:05straightforward to diagnose on the basis01:07of substantially altered mental status01:09so the second type of hypoventilation is01:11a respiratory mechanical problem where01:13the brain is stimulating the body to01:15breathe but the body is unable to01:16breathe either due to a tracheal01:18obstruction or upper airway obstruction01:20or neuromuscular problem involving the01:22diaphragm in the chest ball for patients01:24with acute respiratory mechanical01:25problem they will compensate for this01:27with tachypnea and they will only01:29develop hypercapnia and hypoxemia when01:32they’re really on the brink of death so01:34most of these patients will present with01:35tachypnea and they’ll be struggling to01:37breathe but they won’t necessarily be01:39substantially hypercapnic nor hypoxemic01:41and things of this nature would include01:42epiglottitis acute transverse myelitis01:45gumbray syndrome neuromuscular problems01:47things like periodic hypokalemic01:49paralysis so some sort of acute01:50neuromuscular or airway catastrophe and01:53once again these patients are not really01:55going to present with hypoxemia usually01:57they will present with almost like an01:59exfixial problem so the last cause of01:59exfixial problem so the last cause of02:01hypoventilation is a chronic respiratory02:03mechanical problem and this can be very02:04difficult to diagnose so these are folks02:06with for example chronic muscular02:08dystrophy or chronic obesity02:10hypoventilation syndrome and what02:11happens here is that the brain adapts to02:14a higher level of paco2 so the brain is02:16kind of okay with this and it doesn’t02:18really stimulate the patient to drive02:20their respiratory rate too too high so02:22patients may show up on a couple liters02:24of oxygen and they’re not an extremist02:26they don’t look too bad most of these02:27patients can be diagnosed because they02:29may be carrying some sort of chronic or02:31obvious diagnosis of a neuromuscular02:34problem but occasionally very rarely you02:36might encounter this for the first time02:39it can be a little tricky to find this.
The following picture sums up the above part of the transcript.The next section of the transcript discusses V/Q mismatch.
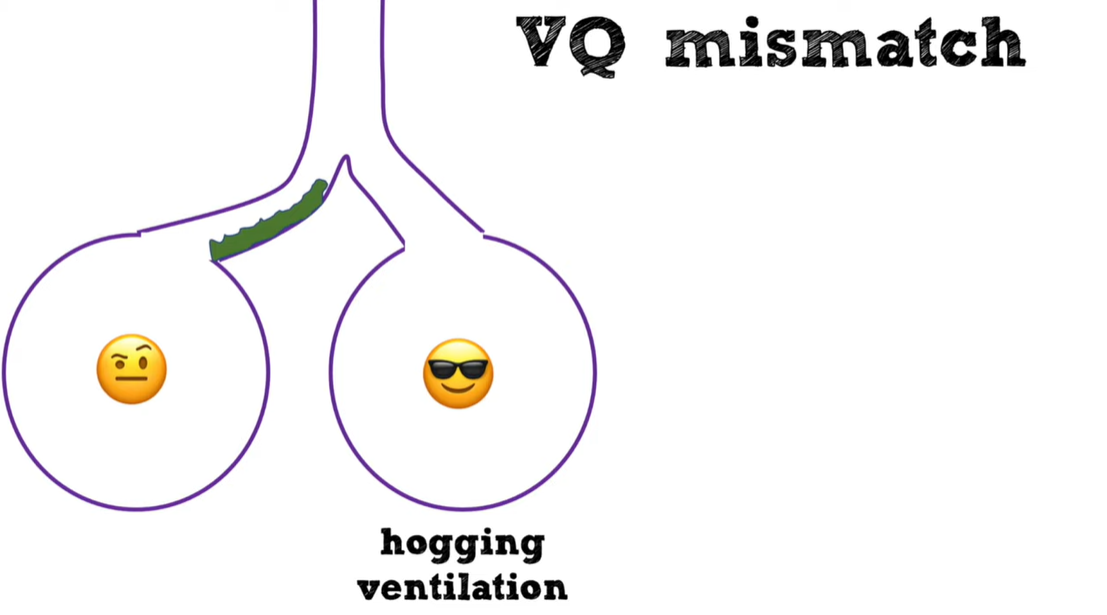
02:40 – 03:32
02:40so getting back to the mainstream here02:41vq mismatch this basically involves a02:44partial obstruction of flow or partial02:47dysfunction of some alveoli so some02:49alveoli are hogging all of the02:51ventilation and other alveoli or getting02:53inadequately ventilated now the problem02:55is that the ventilation hogs here are02:57wasting this ventilation they don’t need02:58that ventilation they are saturating 10003:01before getting the extra ventilation the03:02extra ventilation does nothing for them03:04meanwhile the other alveoli are starved03:06for ventilation they become hypoxemic03:08and the net effect is that overall blood03:10becomes hypoxemic so vq mismatch is the03:12answer to everything in pulmonary03:14medicine if you’re ever asked for a03:15question on you know the boards or03:18rounding and you know why is this03:19patient hypoxemic you can always guess03:21vq mismatch and you’re generally going03:23to be right so this includes patients03:24with asthma copd pulmonary embolism most03:26patients with bronchodomonia where they03:28have kind of like some obstruction of03:29the bronchi but the lung is basically03:31functioning most of your heart failure03:32patients most of your interstitial lung
Next comes shunt
03:34 – 04:02
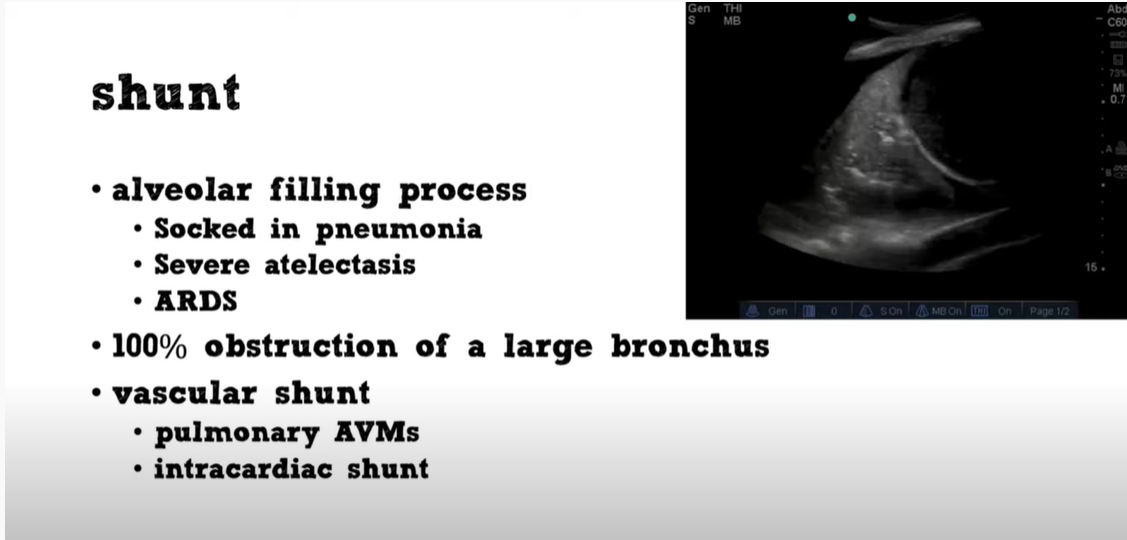
03:34disease patients so our final cause of03:36hypoxemia shunting this involves some03:38situation where the blood does not come03:40in contact with oxygen and there is no03:43way for the blood to ever come in03:45contact with oxygen the most common way03:46that this occurs is an alveolar filling03:49process for example some alveoli are03:51filled completely with plus in the case03:53of pneumonia and no matter how much03:56oxygen you give this patient no matter03:57how much that patient breathes there is03:59not going to get any oxygen to the04:00alveolus and all the blood going to that04:02alveolus is going to be deoxygenated.
Vascular Shunting
04:04 – 04:56
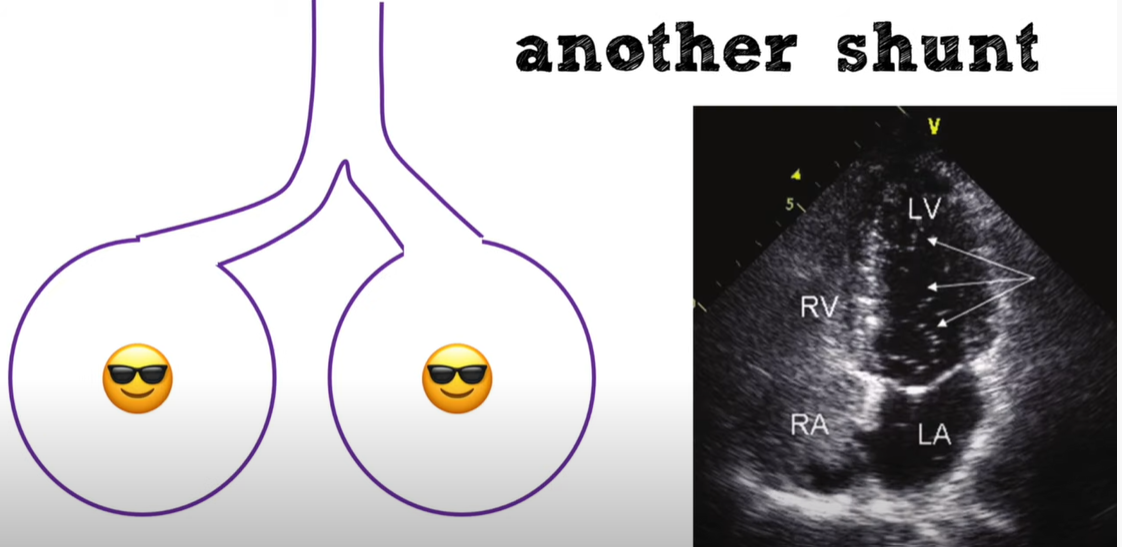
04:04another cause of shunting is a vascular04:07or intracardiac shunt and what’s going04:09on here is deoxygenated blue blood from04:12the right side of the heart is pouring04:13directly into the left side of the heart04:15without ever coming in contact with the04:17alveoli so even if the alveoli may be04:20functioning perfectly this patient will04:22still desaturate so shunts may be caused04:24by alveolar filling processes most04:26commonly things like socketing pneumonia04:28severe adolexis with total on collapse04:30ards sometimes you can see folks with04:33kind of a diffuse infiltrate on their04:34chest x-ray but what they have are kind04:36of just patchy areas where the alveoli04:38are totally dysfunctional in args and04:40that can cause a shunts you can have04:42folks with bronchial obstruction of a04:43large process and that’s probably what’s04:45going on in the icu when you have an04:47intubated patient who suddenly04:48desaturates and they get suctions and04:50then their saturation pops right up04:52those are intermittent kind of bronchial04:53obstruction due to mucus plugging and of04:55course vascular shunting like04:56intracardiac shots in pulmonary avms
How To Use This Information Clinically
04:58 – 06:0604:58we talked about hypoventilation vq05:00mismatch and shunting so how can we05:02actually use this information clinically05:03so let’s think about what will happen if05:05we expose patients with hypoventilation05:08vq mismatch or shunting to a hundred05:10percent oxygen or a very high inhaled05:12amount of oxygen in hypoventilation and05:14vq mismatch if we’re flooding these05:16patients with oxygen there’s so much05:18oxygen in their trachea that even if05:19there’s not like a huge bulk flow going05:21to these alveoli in hypoventilation or05:24even if there’s like an obstruction here05:25in vq mismatch the oxygen concentration05:28is so high that enough oxygen will get05:29into the alveoli that the saturation05:31will be okay alternatively for our05:33patients with shunts it they don’t care05:35it doesn’t matter you can give these05:37patients 100 oxygen it’s still not going05:39to get to that alveolus and they will05:40still be hypoxemic so this is a super05:42important concept here hypoventilation05:44and vq mismatch can be fixed with oxygen05:47whereas supplemental oxygen will not fix05:49a shunt so what this means is that
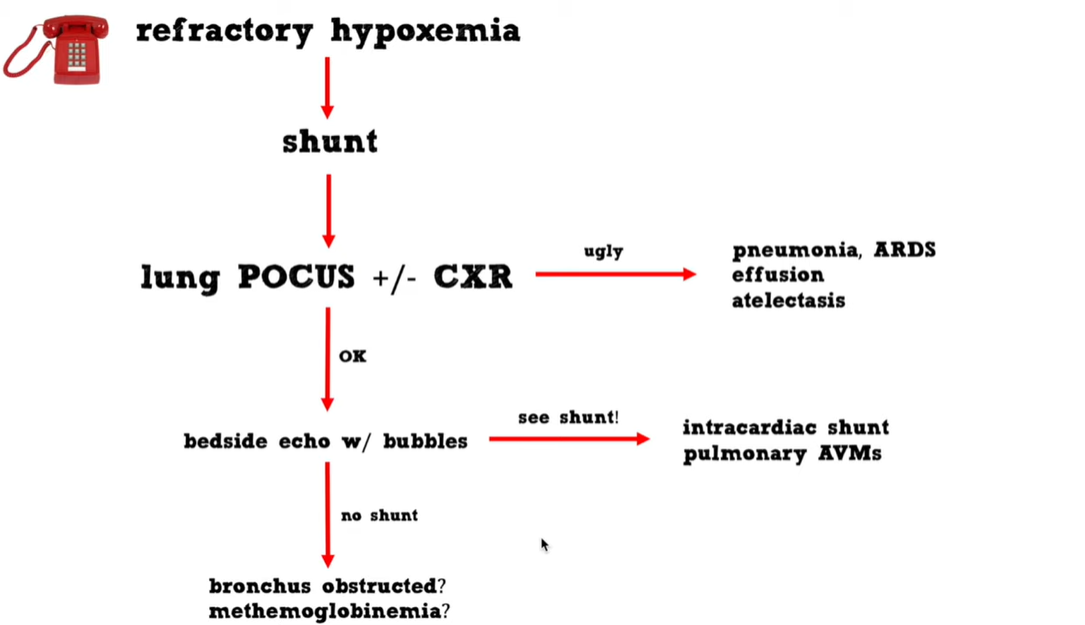
05:51refractory hypoxemia must always be due05:54to a shunt so when you get called that05:55there’s a patient who has hypoxemia05:57that’s not responding to oxygen you can05:59know over the phone right then and there06:01that that’s a patient with shunt06:02physiology even before you go down to06:04the emergency department to see that06:06patient.
06:06 – 07:0406:08the basic stuff we’re going to look at06:09their lungs with ultrasounds perhaps06:11we’re going to look at a chest x-ray and06:13most of the time we’re going to find06:14some sort of obvious pathology in the06:16lungs which will explain their hypoxemia06:18we can move on from there but what if06:20the lung ultrasound and the chest x-ray06:22are normal then we need to consider the06:23possibility of an intracardiac shunt or06:26vascular shots and the way that we can06:27evaluate those at the bedside is to06:30inject agitated saline while doing a06:32bedside pocus that’s a pretty simple06:34thing to do i think anyone who’s06:36interested in emergency medicine or06:37critical care should probably know how06:38to do that and you can identify at the06:41bedside patients with intracardiac06:42shunting or pulmonary avms you can06:44differentiate between those two06:46pathologies based on when the bubbles06:47show up in the left side of the heart06:49now what if your shunt study is negative06:52there are no bubbles on the left side of06:53the heart then you get into a weird box06:55here maybe this patient has a strange06:57bronchial obstruction perhaps they have06:59methemoglobinemia it’s a little outside07:01the scope of this talk but it’s07:02relatively easy to diagnose once you07:04think about it.
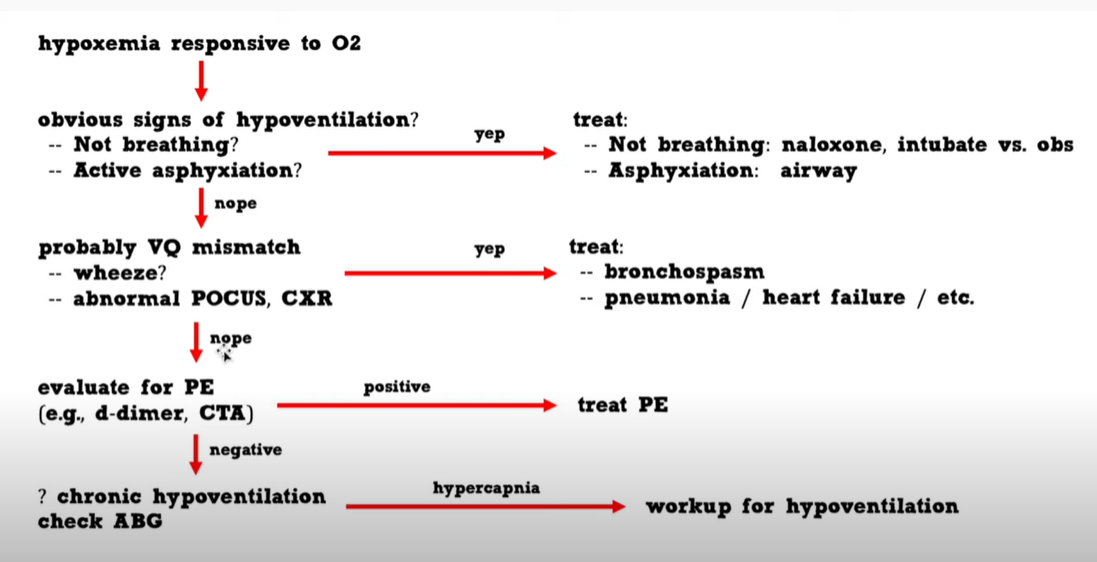
07:04 – 07:57
07:04So let’s get back to07:05bread and butter here. what about our07:07hypoxemic patient who is responsive to07:09oxygen so you’re called to evaluate a07:11patient who is on two to four maybe five07:13liters of oxygen and their saturation07:15response to the oxygen what’s going on here07:17so you can know apriori that these07:19patients probably have either the07:20mismatch or hypoventilation so our07:22approach to a patient with hypoxemia07:24responsive to oxygen now first we’re07:26going to look at the patient if they’re07:27clearly not breathing maybe they’re07:29probably hypoventilating if they are07:31asphyxiating perhaps they have an upper07:33airway obstruction these things are07:34usually going to be relatively clear to07:36detect and honestly they’re not going to07:38really manifest with hypoxemia so moving07:40on from there most of these patients are07:42going to have vq mismatch so here’s07:44where we do our basic pulmonary workup07:46we listen to them we do an ultrasound so07:48perhaps they bronchospasm asthma copd07:50perhaps they have pneumonia heart07:51failure stuff like that this is our07:53bread and butter evaluation for07:55hypoxemia that we’re used to doing all07:57if that [POCUS, CXR, and auscultation for wheezing] is negative this is07:59when you need to think about pulmonary08:00embolism so you’re going to pull out08:01your d-dimer your ct angio and perhaps08:04diagnose a pe or maybe find some sort of08:06subtle lung pathology that you missed08:08previously if that is negative then you08:10need to reconsider the possibility that08:11the patient may have hypoventilation and08:13check an abg to look for hypercapnia08:16this is a rare occurrence but08:17occasionally you may see this so finally