In this post, I link to and embed the YouTube video, Management of Gastrointestinal Symptoms in Dysautonomia – Laura Pace, MD, PhD. Jul 20, 2020. Dysautonomia International.
Dr. Laura Pace is a neurogastroenterologist from the University of Utah. She gave a great overview of gastrointestinal motility testing and how these tests may be helpful for people with dysautonomia who have gastrointestinal motility problems.
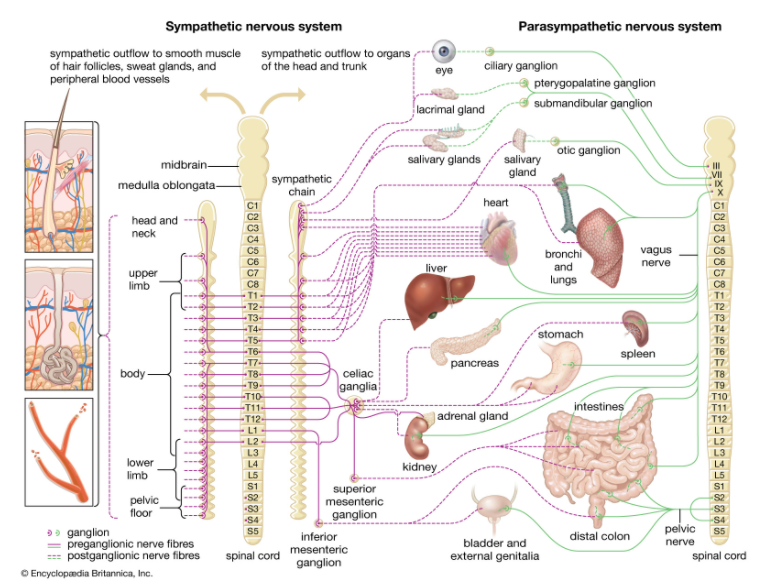
03:18gonna start with a couple definitions um03:20so you know what I’m talking about so03:21review of systems I’m sure you guys have03:23all filled these out extensively for03:25every physician you’ve ever seen but03:26just so you know it’s a description of03:28symptoms related to a particular body03:30system so it can be related to the03:32cardiac system the pulmonary system or03:34the gastrointestinal system and then03:37comorbid conditions these are other03:39diagnoses or conditions that one has and03:42so when I see a patient in clinic and I03:46just sort of want to remind you that not03:48everyone I see initially knows that they03:50have a disorder of the autonomic nervous03:52system sometimes this is me picking it03:55up and sending them for confirmatory03:56diagnosis but many of you that come to03:59see me actually know you have already04:01have this diagnosis but what I do is I04:04start with a detailed history and04:06physical examination so wait well beyond04:09just gastrointestinal symptoms usually I04:11want to start when you first got sick04:13the vast majority are my patients are04:17female and they’ve already been seen by04:19usually a huge number of physicians in a04:22bunch of different specialties they04:25typically report a constantly04:26as symptoms and I’m sure none of these04:28are unusual for you I mean we can start04:30at the top with brain fog headache dry04:32mouth dry eyes palpitations shortness of04:36breath and numerous gastrointestinal04:38symptoms they usually range from04:40difficulty swallowing to even just like04:43what we call global sensation that’s04:45that persistent feeling that something’s04:47stuck in your throat and you kind of04:48keep swallowing to try and clear it but04:51you don’t have like a true impaction04:53within the esophagus all the way to04:56abdominal pain nausea vomiting04:58constipation diarrhea or some alteration05:01in between and so historically within05:05the realm of gastroenterology and even05:08when I came through training the05:10inclination has been to diagnose people05:12who come in with this constellation of05:14symptoms with a functional disorder such05:16as irritable bowel syndrome and this is05:20completely incorrect so that terminology05:22describes a cluster of symptoms but does05:25not give you a diagnosis and does not05:28impart any understanding to it to what05:30the underlying pathophysiology of your05:33symptoms are so typically functional05:37gastrointestinal disorders are symptoms05:39that do not have an identifiable05:40structure or biochemical basis and05:42everybody pretty much agrees on that05:44however many of these disorders we’ve05:46actually been able to resolve and we05:47understand what the cause is the reason05:51I’m showing this slide is I actually05:53find it’s helpful when I talk to other05:55physicians who think that the patients05:59that I’m seeing have a psychiatric06:02illness and so the point that I make06:06with this if we look at the innervation06:08of the autonomic nervous system it06:11innervates just about everything and so06:14when something with the autonomic06:15nervous system goes awry it’s not06:17surprising that you have all these06:19symptoms and so if you look at the the06:23sympathetic branches and then the06:25parasympathetic branches these two06:28systems have different functions and I06:30know many of you are probably familiar06:32with this but the sympathetic nervous06:34system is your fight-or-flight so when06:37this system is overactive it shut06:40down digestion and so what we see in06:42individuals with an overactive component06:44of the sympathetic nervous system we see06:47a lot of delay in different regions of06:50the gastrointestinal tract a lot of06:52difficulty with eating and then with the06:56parasympathetic nervous system you can06:59see the opposite so you can see a lot of07:01really persistent diarrhea that we have07:02a difficult time managing but again the07:05autonomic nervous system is innervating07:08everything it’s not unusual for you to07:10have all these symptoms it’s not unusual07:12if your symptoms are exacerbated by07:14stress that again does not mean that you07:16have a psychiatric illness no matter07:18what your physicians tell you what I07:22don’t understand when I am seeing you07:24guys in clinic is does the07:27gastrointestinal dysfunction come first07:29or does the dissident Omiya come first07:32is essentially a chicken or egg problem07:34and so the thing that I struggle with is07:37in order to make your gastrointestinal07:39symptoms better do I have to treat your07:41dissident Omiya and if your dissident07:44Omiya gets better can I expect your07:45gastrointestinal symptoms to get better07:47and I think that is the case and so I07:50think there are specific things that I07:52can do as a gastroenterologist but then07:54there are other things where we actually07:55really have to address the underlying07:57dissident Omiya one of the other08:00problems is I feel like it’s really08:02important to understand what comorbid08:05conditions you actually have and I know08:07there’s some debate about this but I08:09think it’s important to know whether you08:10have an underlying connective tissue08:12disorder whether it be EDS or some other08:14whether you have presence of mast cell08:17activation syndrome or a metabolic08:19disorder or an autoimmune disorder08:21because all of this is going to change08:23how I approach the symptoms that we have08:27to address for you so I recommend a08:31thorough evaluation so that I can put08:33together an entire clinical picture and08:35sort of make better recommendations and08:37so what I’m going to go through here is08:39the evaluation that I have most of my08:42patients undertake and not it’s not in08:44any specific order08:45I just tried to organize it so maybe if08:47we talked about one topic it would08:49relate to the topic before so we’re08:51going to start with motility testing08:53um and just so we’re all on the same08:56page a couple definitions so motility08:58describes movement and so essentially09:00when we’re talking about it in reference09:02to the gastrointestinal tract we’re09:03talking about coordinated movements so09:05we’re talking about appropriate09:07contractions in one segment relaxation09:09in another segment and then that09:11sequential change throughout time so as09:13you go through the entire09:14gastrointestinal tract transit time is09:17in reference to the time it takes to09:19move through a segment so the time it09:22takes your stomach to empty the time it09:24takes food and things like that to move09:26through your small intestine the time it09:28takes things to move through your colon09:30and then manometry it’s a measurement of