In this post, I link to and excerpt from CORE IM’s 5 Pearls Podcast,
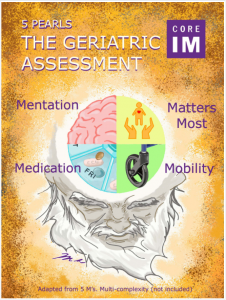
5 Pearls on The Geriatric Assessment.*
*Posted: October 31, 2021
By: Dr. Minali Nigam, Dr. Andrea Schwartz, Dr. Laura Perry and Dr. Shreya P. Trivedi
Graphic: Dr. Michelle Lo
Audio: Max Had
Peer Review: Dr. Amy Shaw, Dr. Colleen Christmas. Accessed 11-11-2021.
All that follows is from the above resource.
Time Stamps
- 02:25 Initial Office Visit
- 08:08 Mobility Assessment
- 13:25 Cognitive Evaluation
- 19:27 Medications
- 26:29 Throwback Pearl
Show Notes
Pearl 1: Approach to the initial office visit
- First understand what matters most to the patient.
- What do they value?
- What does a good day look like?
- Functional status is the ability to perform daily activities to meet basic life needs (ADLs).
- There are basic and instrumental ADLs.
- Assess baseline function, which can be used to later track disease onset and progression.
- Think of toenail length as the hemoglobin A1c of functional independence.
- If toenails are too long (>2mm increase in length per month) consider broad differential:
- Loss of executive function
- Decreased flexibility/muscle strength
- Caregiver burnout, social isolation
- Poor vision
Pearl 2: “Moves” for mobility
- Falls are the leading cause of injury-related death in adults over 65 years old
- Think of gait speed as a vital sign and important predictor for fall risk.
- Stratify fall risk by assessing mobility.
- Slowed gait speed increases risk
- Timed get up and go test (TUG): Time how long it takes for a patient to stand up from chair without pushing off with arms, walk to a line on the floor (10 feet away), turn, walk back to the chair and sit down.
- If the patient takes longer than 12 seconds to complete TUG they’re at risk for falling.
- Chair stand: Have the patient cross arms over chest and stand up from chair. If they can’t stand up without using hands for support, they’re at higher fall risk.
- Interventions to decrease fall risk are most effective when combined together and include physical and occupational therapy, home modifications (safe furniture, remove environmental hazards), use of appropriate assistive devices for ambulation and medication review.
Pearl 3: Cognitive evaluation
- Cognitive decline is a common concern in the primary care setting
- Cognitive Screening Tests
- The Mini-Cog is a quick screening test which assesses the ability to recall three words and draw a clock. If unable to complete successfully, need a more elaborate test
- Montreal Cognitive Assessment (MOCA): Scored out of 30 points and evaluates naming, memory, attention, language, delayed recall, among other domains.
- Delirium is an acute change in mental status from baseline.
- Start with quick orientation and attention questions. Ask the patient to name days of the week or months of the year backwards
- If cognitive tests show impairment, rule out reversible causes like hearing loss, medications, hypoglycemia, nutritional deficits, thyroid disorders, or electrolyte abnormalities.
Pearl 4: How to manage medications
- Ask patients to bring all their meds to the initial visit, including over the counter medications. Figure out what they’re actually taking. May need collateral from pharmacy, family members or home health aid.
- Match the medications to the problem list. Consider de-prescribing.
- Are there extra medications that don’t match anything on the problem list?
- Are there medications with side effects that are contributing to the problem list?
- Is there a less frequent alternative? Example: switching metoprolol tartrate to metoprolol succinate
- Are the medications consistent with the person’s goals of care and life expectancy?
- Underprescribing is a problem too
- Osteoporosis often goes undertreated. Use bisphosphonates.
- Pain control with tylenol can significantly improve quality of life
- Oral anticoagulants require weighing stroke risk versus fall risk
Throwback Pearl: PPIs
- Divide adverse effects of PPIs into two big buckets: Malabsorption (Vitamin B12 deficiency, Hypomagnesemia and Osteoporosis) AND Infection (C difficile colitis).
- Strategies to take patients off PPIs include short, finite prescriptions to begin with, managing expectations and using rescue meds.
*The above is a direct link to the transcript section of the outstanding show notes.