Today, I review, link to, and excerpt from Society of Critical Care Medicine and the Infectious Diseases Society of America Guidelines for Evaluating New Fever in Adult Patients in the ICU. [PubMed Abstract] [Full-Text HTML] [Download Full-Text PDF]. Crit Care Med. 2023 Nov 1;51(11):1570-1586. doi: 10.1097/CCM.0000000000006022. Epub 2023 Oct 12
Each recommendation is followed in the article by the rationale for that recommendation.
All that follows is from the above resource.
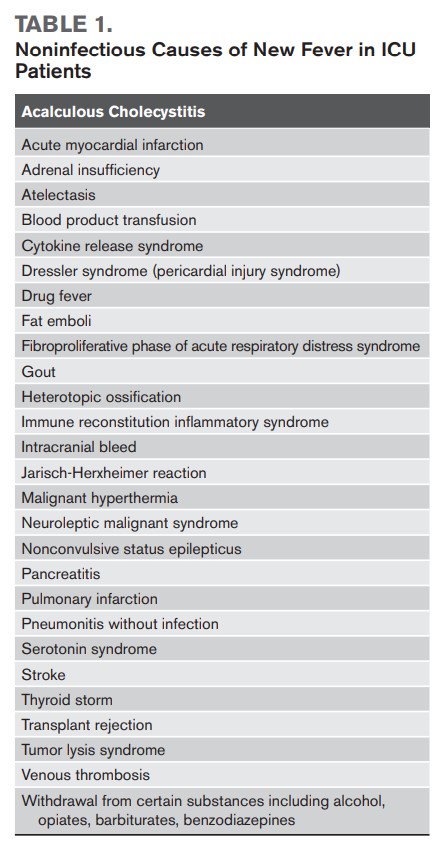
Fever, a frequent early indicator of infection, occurs in 26–88% of adult ICU patients, depending on the definition used and characteristics of the cohort studied (1). The range of potential etiologies of fever is vast and includes both infectious and noninfectious causes (2). Noninfectious causes of fever should be considered in the differential diagnosis (Table 1), but because early treatment initiation may improve outcomes of infections, initial evaluation of patients with new-onset fever is usually directed at potential microbial causes, and this is the primary focus of this guideline.
Recommendations and best-practice statements are listed in Table 2.
TABLE 2. – Consensus Recommendations
1. Central temperature monitoring methods, including thermistors for pulmonary artery catheters, bladder catheters, or esophageal balloon thermistors, are preferred when these devices are in place or accurate temperature measurements are critical to diagnosis and management. For patients without these devices in place, we suggest using oral or rectal temperatures over other temperature measurement methods that are less reliable (such as axillary or tympanic membrane temperatures, noninvasive temporal artery thermometers, or chemical dot thermometers) (weak recommendation, very low-quality evidence). 2. For critically ill patients with fever, we suggest avoiding routine use of antipyretic medications for the specific purpose of reducing the temperature (weak recommendation, moderate quality evidence). 3. For critically ill patients with fever who value comfort by reducing temperature, we suggest using antipyretics over nonpharmacologic methods to reduce body temperature (weak recommendation, low-quality evidence). 4. For patients who develop fever during ICU stay, we recommend performing a chest radiograph (best-practice statement). 5. For patients who have recently undergone thoracic, abdominal, or pelvic surgery, we recommend performing CT (in collaboration with the surgical service) as part of a fever workup if an etiology is not readily identified by initial workup (best practice statement). 6. For critically ill patients with fever in whom other diagnostic tests have failed to establish an etiology, we suggest either performing an 18F-fluorodeoxyglucose positron emission tomography/CT if the risk of transport is deemed acceptable (weak recommendation, very low-quality evidence). 7. The panel found insufficient evidence to issue a recommendation regarding the use of WBC scan for patients with fever without an established etiology. 8. For critically ill patients with fever and no abdominal signs or symptoms or liver function abnormalities, and no recent abdominal surgery, we recommend against the routine use of a regular abdominal ultrasound or point-of-care ultrasound (POCUS) as an initial investigation (best-practice statement). 9. In patients with fever and recent abdominal surgery or in any patient with either abdominal symptoms or suspicion of an abdominal source (e.g., abnormal physical examination/POCUS, increased transaminases, or alkaline phosphatase, and/or bilirubin), we recommend performing a formal bedside diagnostic ultrasound of the abdomen (best-practice statement). 10. For critically ill patients with fever and an abnormal chest radiograph, we suggest performing a thoracic bedside ultrasound when sufficient expertise is available to more reliably identify pleural effusions and parenchymal or interstitial lung pathology (weak recommendation, low-quality evidence). 11. Insufficient evidence was found to issue a recommendation regarding the use of thoracic bedside ultrasound for patients with fever without chest radiograph abnormalities. 12. For ICU patients with fever without an obvious source and who have a central venous catheter, we recommend simultaneous collection of central venous catheter and peripherally drawn blood cultures to allow calculation of differential time to positivity (Best practice statement). 13. In patients with fever in the ICU in whom central venous catheter cultures are indicated, we recommend sampling at least two lumens (best-practice statement). 14. For critically ill patients with a new fever of unclear origin, we suggest that if rapid molecular tests on blood are performed, they should only be used with concomitant blood cultures (weak recommendation, very low-quality evidence). 15. When performing blood cultures in adult ICU patients, we recommend collecting at least two sets of blood cultures (ideally 60 mL of blood total) one after the other, from different anatomical sites, without a time interval between them (best practice statement). 16. For febrile ICU patients with pyuria and in whom urinary tract infection is suspected, we recommend replacing the urinary catheter and obtaining urine cultures from the newly placed catheter (best-practice statement). 17 . For critically ill patients with a new fever and suspected pneumonia, or new upper respiratory infection symptoms (e.g., cough), we suggest testing for viral pathogens using viral nucleic acid amplification test panels (weak recommendation, very low-quality evidence). 18. There was insufficient evidence to allow a recommendation on performing routine blood testing for viral pathogens in immunocompetent patients in the ICU (e.g., herpesviruses, adenovirus). 19. For critically ill patients with a new fever, we recommend testing for severe acute respiratory syndrome coronavirus 2 by PCR based on levels of community transmission (best-practice statement). 20. If the probability of bacterial infection is deemed low to intermediate in a critically ill patient with a new fever and no clear focus of infection, we suggest measuring procalcitonin (PCT) in addition to bedside clinical evaluation vs bedside clinical evaluation alone (weak recommendation, very low-quality evidence). 21. If the probability of bacterial infection is deemed high in a critically ill patient with a new fever and no clear focus of infection, we suggest not measuring PCT to rule out bacterial infection. (Weak recommendation, very low-quality evidence). 22. If the probability of bacterial infection is deemed low to intermediate in a critically ill patient with a new fever and no clear focus of infection, we suggest measuring C-reactive protein (CRP) in addition to bedside clinical evaluation vs bedside clinical evaluation alone (weak recommendation, very low-quality evidence). 23. If the probability of bacterial infection is deemed high in a critically ill patient with a new fever and no clear focus of infection, we suggest not measuring CRP to rule out bacterial infection (weak recommendation, very low-quality evidence). 24. If the probability of bacterial infection is deemed low to intermediate in a critically ill patient with a new fever and no clear focus of infection, we suggest measuring serum PCT or CRP to rule out bacterial infection (weak recommendation, very low-quality evidence).