In this post, I link to and excerpt from The Cribsiders‘ #45: Neonatal Hyperbilirubinemia – Their Future’s So Bright, They Gotta Wear Shades!
MARCH 2, 2022 By SAM MASUR*
*Zhang AY, Holmes A, Shimotake T, Cruz M, Masur S, Chiu C, Berk J. “#45: Neonatal Hyperbilirubinemia – Their Future’s So Bright, They Gotta Wear Shades!”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ March 2, 2022.
All that follows is from the above resource.
Summary
Aren’t all babies a little jaundiced anyways?
What’s up with those phototherapy lights? Come for the answers, stay for this de-light of a conversation with pediatrician Dr. Alison Holmes and neonatologist Dr. Tom Shimotake, both of whom have extensive experience with commonly used guidelines for neonatal hyperbilirubinemia. We will cover common and rarer etiologies of neonatal hyperbilirubinemia, the whens and hows of working up and screening, and the ins and outs of treatment.
Neonatal Hyperbilirubinemia Pearls
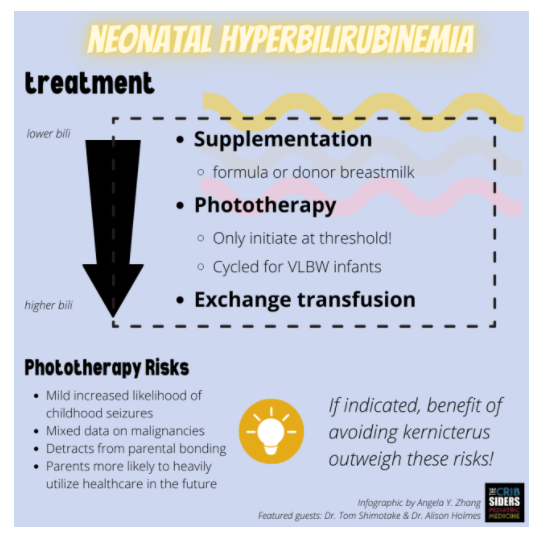
- Unconjugated neonatal hyperbilirubinemia is very common and can be benign, though frightening, to parents. When you have low concern for other pathophysiology, encourage feeding and supplementation to alleviate starvation jaundice. [Unconjugated hyperbiliruinemia is indirect bilirubin and can be treated with phototherapy. Direct hyperbilirubinemia is conjugated biliruin and is abnormal if approaching 20% of total bilirubin and is not treated or helped by phototherapy. It is urgent to diagnose elevated direct bilirubin.]
- Have a systematic approach to hyperbilirubinemia and keep an open mind, especially with an unexpected clinical course. A good history is key!
- Physical exam skills can identify sources of possible hemolysis, but aren’t always the best for jaundice.
- Equitable care practices include universal bilirubin screening at 24 hours of life, and ensuring robust follow-up after discharge from the birthing center, nursery, or NICU.
- Be judicious with interventions and don’t initiate subthreshold phototherapy.
Hyperbilirubinemia Show Notes
Pathophysiology & Risk Factors
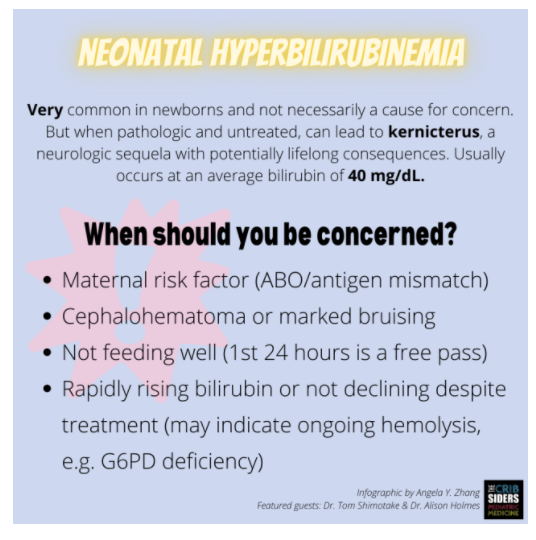
- Unconjugated hyperbilirubinemia is very common in the newborn period due to high turnover of fetal red blood cells shortly after birth. Reassure parents that jaundice (physical exam finding of hyperbilirubinemia) can be normal and, according to Dr. Holmes, seen in up to 80% of breastfed infants.
- Kernicterus, or bilirubin encephalopathy, is the main concern of neonatal hyperbilirubinemia. Kernicterus occurs when unconjugated bilirubin crosses the blood-brain barrier and deposits in the basal ganglia, causing acute and sometimes chronic neurologic damage. Clinical manifestations include lethargy, weak tone, altered mental status, and seizures.
Unconjugated Hyperbilirubinemia
Risk factors for unconjugated hyperbilirubinemia, resulting in a high indirect bilirubin, are varied and fall into several categories.
Parental Risk Factors
- ABO incompatibility between birthing parent and fetus.
- Blood group antibody mismatch between birthing parent and fetus.
- Family history of hyperbilirubinemia.
- Birthing parent history of gestational diabetes.
Expert pearl: Obtain a thorough set of labs from birthing parent’s prenatal care from your obstetric and family medicine colleagues, including the minor blood group antigens which are often responsible for an antibody setup.
Processes Leading to Increased Production of Bilirubin
- Hereditary spherocytosis and other RBC membrane defects.
- G6PD deficiency, PK deficiency, and other erythrocyte enzymatic defects.
- Polycythemia.
- Source(s) of increased RBC breakdown, such as a cephalohematoma.
- Sepsis.
Expert pearl: Although G6PD deficiency is classically taught to occur more often in darker-skinned populations, it is in fact a global concern and can happen in many populations that ethnic categorizations are not adequate for. Because a large percentage of kernicterus cases can be attributed to G6PD deficiency (up to 30%), it is important not to let bias determine screening and workup, especially as hemolysis from G6PD deficiency may not occur in the first few days of life.
Decreased Clearance
- Crigler-Najjar
- Gilbert syndrome
Increased Enterohepatic Circulation leading to increased bilirubin gut absorption
- Breastmilk jaundice
- Intestinal obstruction or ileus
Finally, a common risk factor is any feeding difficulty, through which an infant does not receive enough nutrition. The pathophysiology of this starvation jaundice is unclear. Expert practice: Although sometimes termed “breastfeeding jaundice”, this term is inaccurate since this type of hyperbilirubinemia can occur with failure to feed either with breastmilk or formula.
Conjugated Hyperbilirubinemia
Conjugated hyperbilirubinemia results from cholestasis and an impaired ability to form or excrete bile. The conjugated, or direct, bilirubin should be less than 20% of the total bilirubin measurement; anything more is considered elevated. Causes include:
- Anatomical (biliary atresia, Alagille syndrome).
- Metabolic (Galactosemia).
- Infectious (hepatitis, other TORCH infections).
Screening and Work-Up
Physical Exam
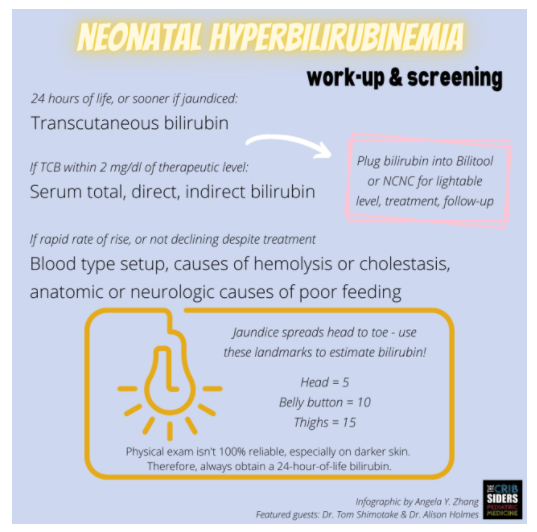
- Jaundice spreads cephalo-caudally, i.e. head-to-toe.
- On skin exam, good rule of thumb for correlating bilirubin levels to the line between jaundice and unjaundiced skin: head = 5; belly button = 10; legs = 15.
- Look for jaundice in conjunctivae, nail beds, and sublingual mucosa.
- Be sure to look for findings that indicate risk for hemolysis, such as bruising or cephalohematoma. Expert pearl: in contrast to normal findings of scalp edema which will depress, a cephalohematoma feels like a water balloon that bounces back.
- Just because you don’t see any clinical findings doesn’t mean that there isn’t any hyperbilirubinemia – have a low suspicion to check a bilirubin, and/or implement universal 24-hour of life screening as below.
Labs
- Obtain cord blood at birth if you’re concerned about an ABO/antigen setup.
- If an infant looks jaundiced before 24 hours of life, obtain a transcutaneous bilirubin.
- At 24 hours of life, all newborns should have a transcutaneous bilirubin screen. Expert opinion: this may reduce health inequities seen in the underdiagnosis of jaundice in darker-skinned infants, although more root-cause solutions would be needed to mitigate disparities in outpatient management (Darling et al., 2017).
Expert opinion: Consider obtaining a TcB meter in your outpatient practice (Kilmarten et al, 2020).
When to check a serum bilirubin?
- Transcutaneous bilirubin is reliable for lower bilirubin levels under 13, and usually predicts bilirubin within 2 points. Therefore, if bilirubin level is either 1) within 2 points of a “lightable” level as determined by Bilitool or NCNC (below), and/or 2) over 13, check a serum bilirubin.
- Although TcBs can be inaccurate for darker-skinned infants (Taylor et al., 2014), the rules above will help mitigate any health inequity resulting from device error.
When you need to check a serum bilirubin, it seems reasonable to me to check the total bilirubin and the direct (conjugated) and indirect (unconjugated) bilirubin.
What to do with the bilirubin measurement?
Stat here.