Today, I reviewed and link to Guidelines for reasonable and appropriate care in the emergency department 3 (GRACE-3): Acute dizziness and vertigo in the emergency department [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Acad Emerg Med. 2023 May;30(5):442-486. doi: 10.1111/acem.14728.
There are 100 similar articles in PubMed.
GRACE – 3 Guidelines is a brief summary of the guidelines from Core EM.
SGEM#403: UNOS, DOS, TRES – VERTIGO: THE GRACE-3 GUIDELINES is a podcast and show notes about the guidelines from The Skeptic’s Guide To Emergency Medicine.
The above article has been cited by 8 articles in PubMed.
All that follows is from the above article.
Abstract
This third Guideline for Reasonable and Appropriate Care in the Emergency Department (GRACE-3) from the Society for Academic Emergency Medicine is on the topic adult patients with acute dizziness and vertigo in the emergency department
(ED). A multidisciplinary guideline panel applied the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to assess the certainty of evidence and strength of recommendations regarding five questions for adult ED patients with acute dizziness of less than 2 weeks’ duration. The intended population is adults presenting to the ED with acute dizziness or vertigo. The panel derived 15 evidence-based recommendations based on the timing and triggers of the dizziness but recognizes that alternative diagnostic approaches exist, such as the STANDING protocol and nystagmus examination in combination with gait unsteadiness or the
presence of vascular risk factors.As an overarching recommendation, (1) emergency
clinicians should receive training in bedside physical examination techniques for patients with the acute vestibular syndrome (AVS; HINTS) and the diagnostic and therapeutic maneuvers for benign paroxysmal positional vertigo (BPPV; Dix–Hallpike test and Epley maneuver).To help distinguish central from peripheral causes in patients
with the AVS, we recommend: (2) use HINTS (for clinicians trained in its use) in patients with nystagmus,(3) use finger rub to further aid in excluding stroke in patients with nystagmus,
(4) use severity of gait unsteadiness in patients without nystagmus,
(5) do not use brain computed tomography (CT),
(6) do not use routine magnetic resonance imaging (MRI) as a first-line test if a clinician trained in HINTS is available,
and (7) use MRI as a confirmatory test in patients with central or equivocal HINTS examinations.
In patients with the spontaneous episodic vestibular syndrome: (8) search for symptoms or signs of cerebral ischemia,
(9) do not use CT, and
(10) use CT angiography or MRI angiography if there is concern for transient ischemic attack.
In patients with the triggered (positional) episodic vestibular syndrome, (11) use the Dix–Hallpike test to diagnose posterior canal BPPV (pc-BPPV),
(12) do not use CT, and
(13) do not use MRI routinely, unless atypical clinical features are present.
In patients diagnosed with vestibular neuritis, (14) consider short-term steroids as a treatment option.
In patients diagnosed with pc-BPPV, (15) treat with the Epley maneuver.
It is clear that as of 2023, when applied in routine practice by emergency clinicians without special training,
HINTS testing is inaccurate, partly due to use in the wrong patients and partly due to issues with its interpretation.Most emergency physicians have not received training in
use of HINTS. As such, it is not standard of care, either in the legal sense of that term (“what the average physician would do in similar circumstances”) or in the common parlance sense (“the standard action typically used by physicians in routine practice”).AT-A-GLANCE SUMMARY
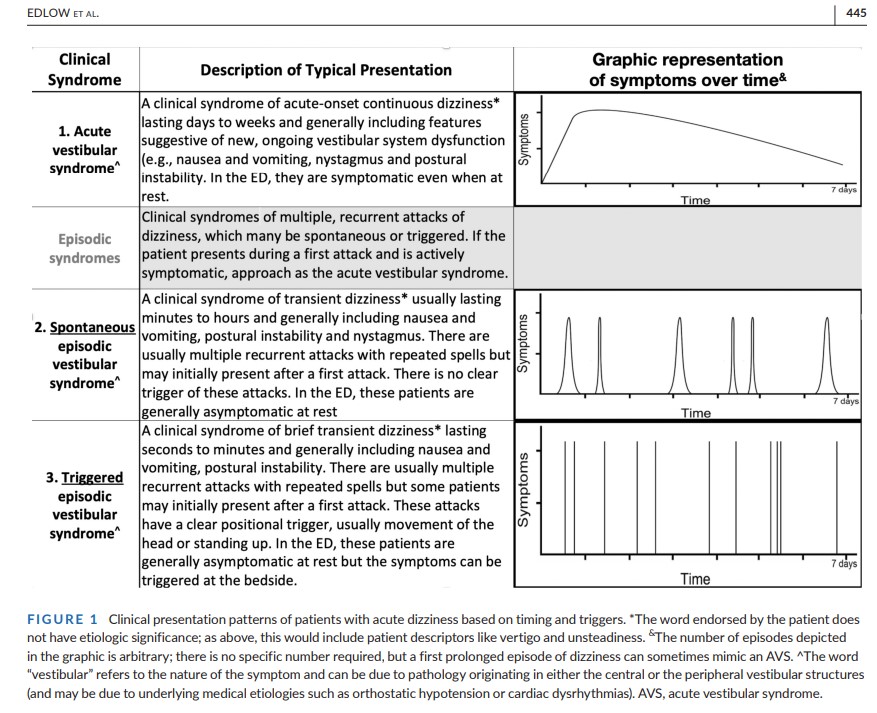
In emergency department (ED) patients with new dizziness or vertigo without an obvious medical or neurological cause, the first step is to try to determine which presenting syndrome the patient has, based on the timing and triggers of symptoms (see Figure 1). As with any patient with any chief complaint, some patients are not able to unambiguously report the timing and triggers of their symptoms. In situations in which the timing and triggers category is unclear, other diagnostic frameworks, such as the STANDING protocol and various combinations of HINTS components and gait unsteadiness or vascular risk factors, may also be diagnostically useful. Because these
physical examination elements are not commonly used in routine emergency medicine practice, their incorporation into practice is aspirational and represents a forward-looking policy to improve care of these patients.a. Acute vestibular syndrome (AVS): acute onset of continuous, persistent dizziness or vertigo lasting longer than 24 h (see Figure 1).
b. Spontaneous episodic vestibular syndrome (s-EVS): one or more
discrete episodes of untriggered, spontaneous dizziness or vertigo (see Figure 1).c. Triggered (positional) episodic vestibular syndrome (t-EVS): one or more discrete very brief episodes of triggered, positional dizziness or vertigo. (see Figure 1).