In this post, I link to and excerpt from 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC) [PubMed Abstract] [Full Text HTML] [Full Text PDF]. European Heart Journal, Volume 41, Issue 3, 14 January 2020, Pages 407–477.
Here are the links to the above guidelines:
Article Contents
All that follows is from the above outstanding guidelines:
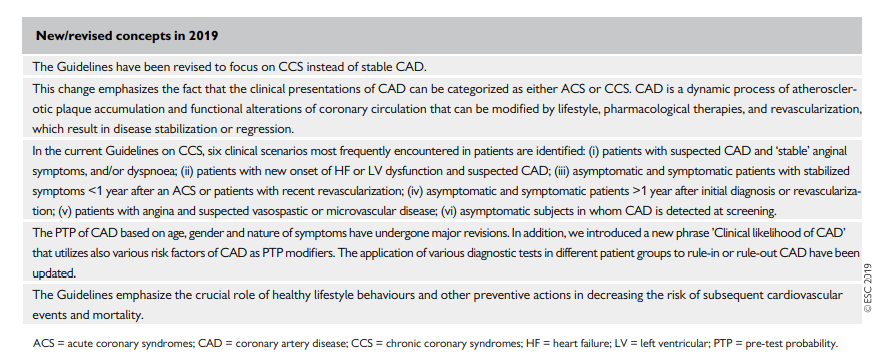
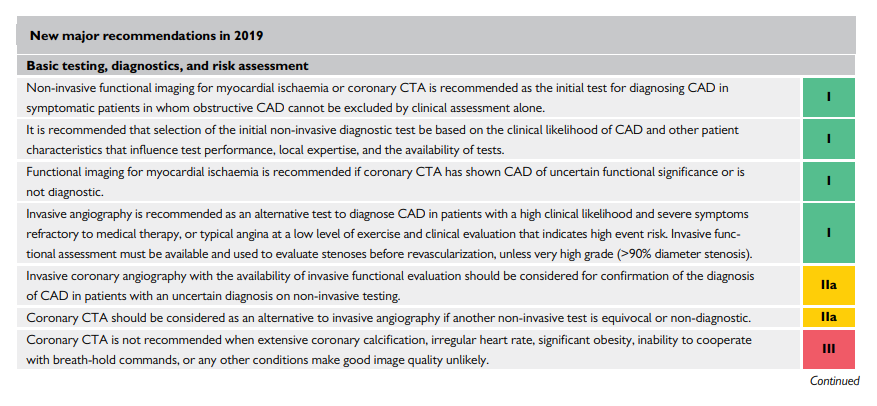
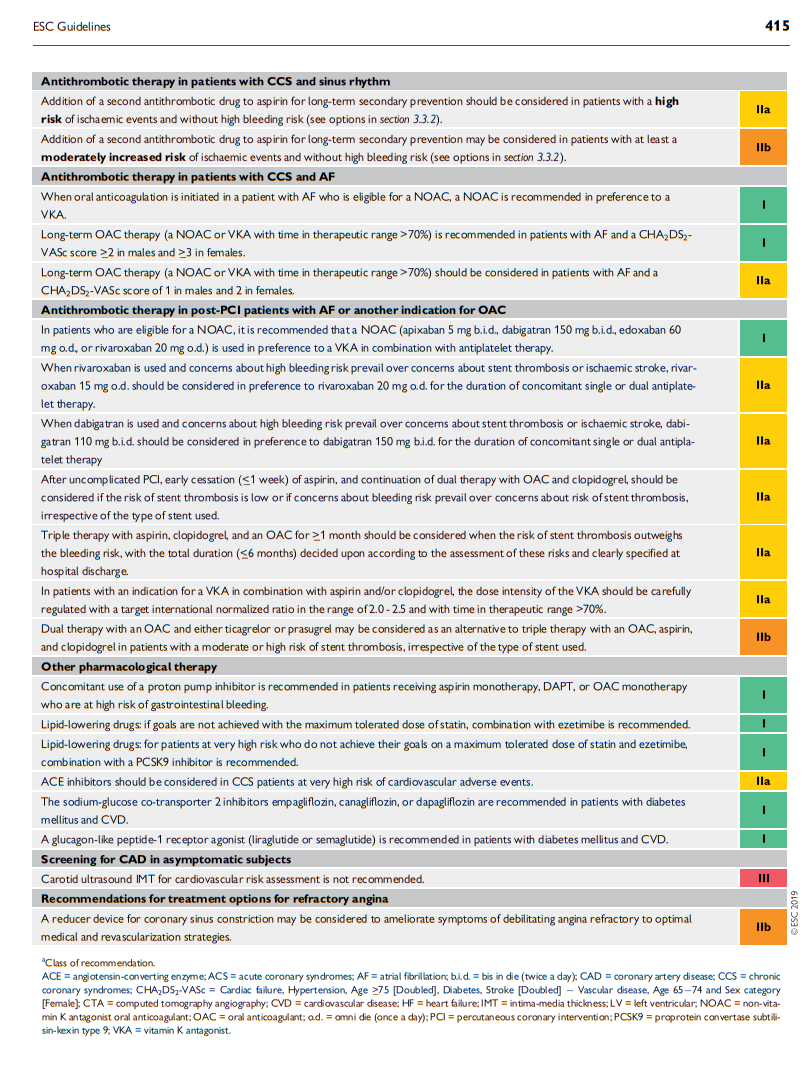
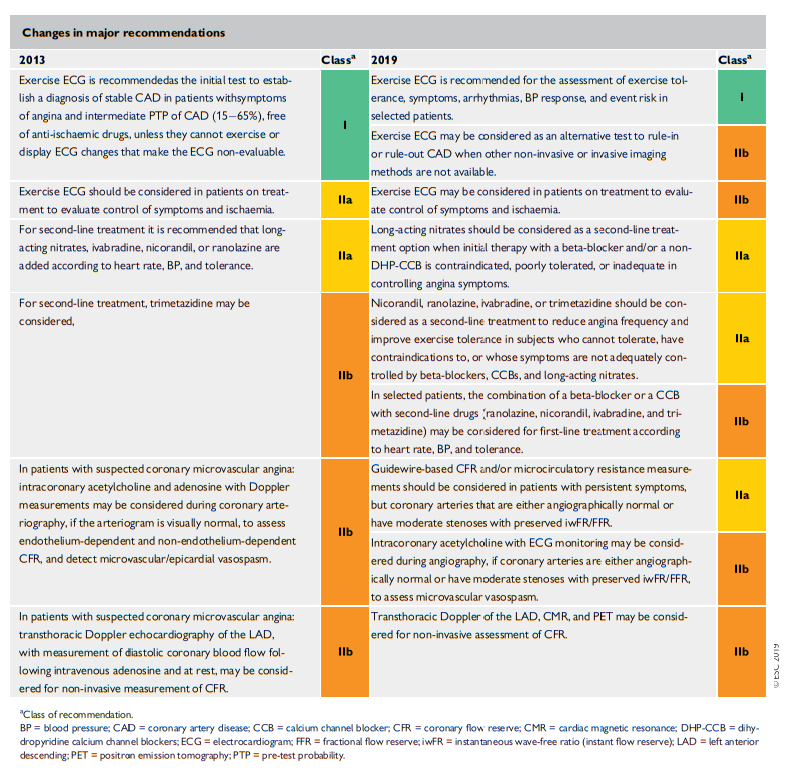
Changes From 2013
3 Patients with angina and/or dyspnoea, and suspected coronary artery disease [PDF pp 417 –
3.1 Basic assessment, diagnosis, and risk
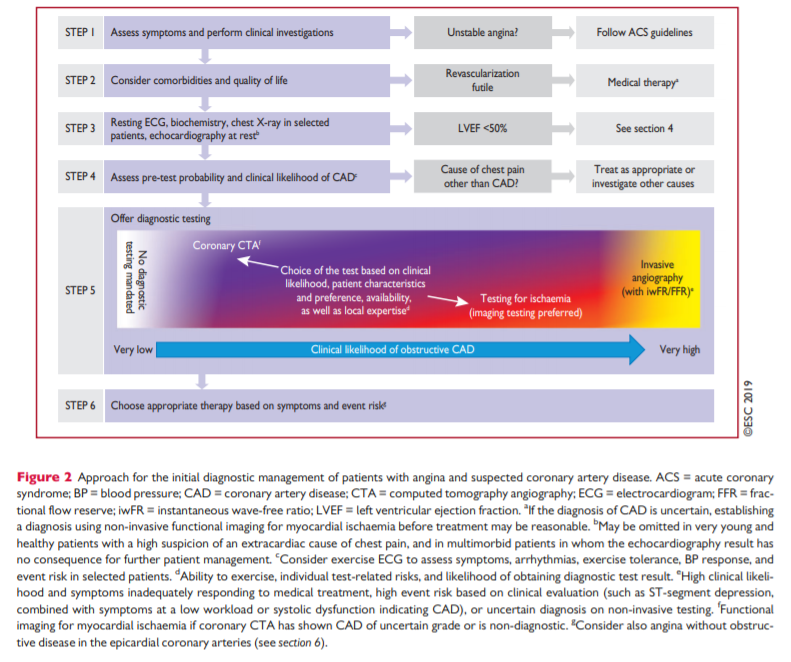
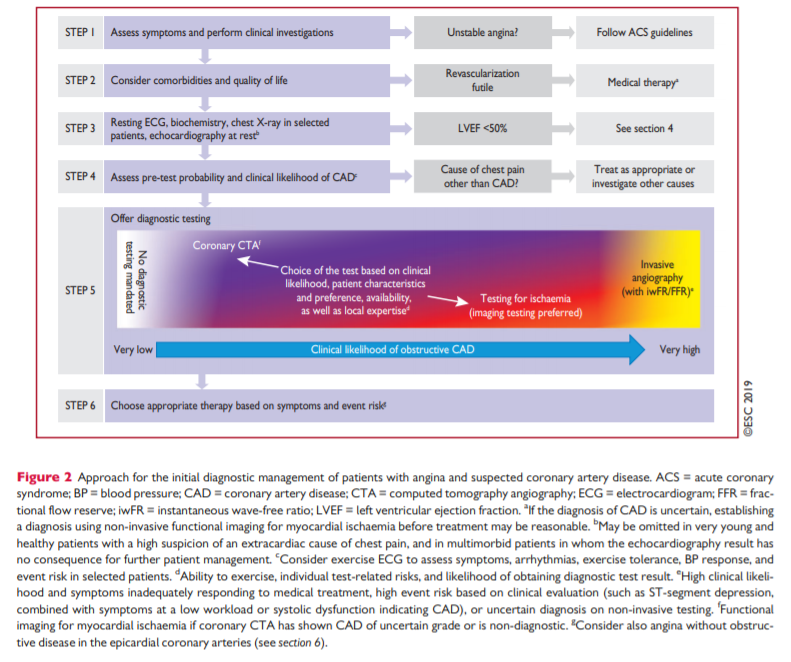
assessment [PDF pp 416 -417]The general approach for the initial diagnostic management of
patients with angina and suspected obstructive CAD is presented in Figure 2. The diagnostic management approach includes six steps.The first step is to assess the symptoms and signs, to identify patients with possible unstable angina or other forms of ACS (step 1). In patients without unstable angina or other ACS,
the next step is to evaluate the patient’s general condition and
quality of life (step 2). Comorbidities that could potentially influence therapeutic decisions are assessed and other potential
causes of the symptoms are considered. Step 3 includes basic testing and assessment of LV function. Thereafter, the clinical likelihood of obstructive CAD is estimated (step 4) and, on this basis, diagnostic testing is offered to selected patients to establish the diagnosis of CAD (step 5). Once a diagnosis of obstructive CAD has been confirmed, the patient’s event risk will be determined (step 6) as it has a major impact on the subsequent therapeutic decisions.3.1.1. Step 1: Symptoms and signs [PDF pp 417 – 418]
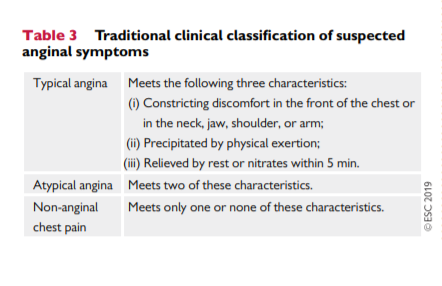
Definitions of typical and atypical angina are summarized in
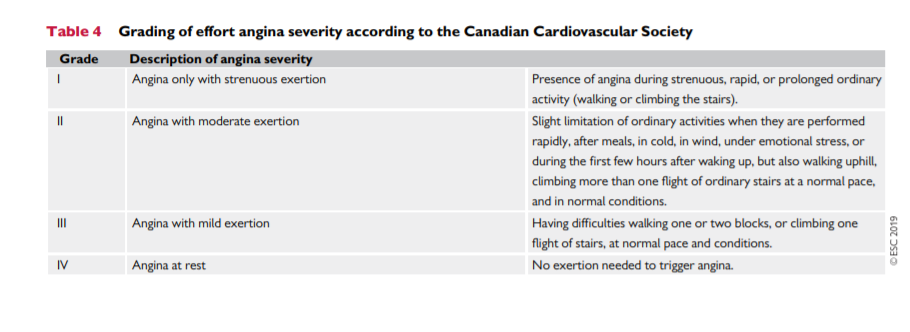
Table 3. The classification, although subjective, is practical and of proven value in determining the likelihood of obstructive CAD.2,3 Studies published since 2015 have reported that the majority of patients suspected of having CAD present with atypical or nonanginal chest pain,46 with as few as 10 – 15% presenting with typical angina.3,7,8 The Canadian Cardiovascular Society classification is still widely used as a grading system for angina,9 to quantify the threshold at which symptoms occur in relation to physical activities (Table 4).Physical examination of a patient with suspected CAD is important to assess the presence of anaemia, hypertension, valvular heart disease, hypertrophic cardiomyopathy, or arrhythmias. It is also recommended that practitioners obtain the body mass index (BMI) andvsearch for evidence of noncoronary vascular disease, which may be asymptomatic [includes palpation of peripheral pulses, and auscultation of carotid and femoral arteries, as well as assessment of the
ankle-brachial index (ABI)], and other signs of comorbid conditions such as thyroid disease, renal disease, or diabetes.3.1.1.1 Stable vs. unstable angina [PDF p 418]
Unstable angina may present in one of three ways: (i) as rest
angina, i.e. pain of characteristic nature and location occurring at rest and for prolonged periods (>20 min); (ii) new-onset angina, i.e. recent (2 months) onset of moderate-to-severe angina (Canadian Cardiovascular Society grade II or III); or (iii) crescendo angina, i.e. previous angina, which progressively increases in severity and intensity, and at a lower threshold, over a short period of time. Management of angina fulfilling these criteria is dealt with in the ESC Guidelines for the management of ACS.*11,12
*2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). [PubMedAbstract] [Full Text HTML] [Full Text PDF]. European Heart Journal, Volume 42, Issue 14, 7 April 2021, Pages 1289–1367
New-onset angina is generally regarded as unstable angina; however, if angina occurs for the first time with heavy exertion and subsides at rest, the suspected condition falls under the definition of CCS rather than unstable angina. In patients with unstable angina identified as being at low risk, it is recommended that the diagnostic and prognostic algorithms presented in these Guidelines be applied once the period of instability has subsided.11 Low-risk patients with unstable angina are characterized by no recurrence of angina, no signs of HF, no abnormalities in the initial or subsequent electrocardiogram (ECG), and no rise in troponin levels.11 In this setting, a non-invasive diagnostic strategy is recommended before deciding on an invasive strategy. Based on the definition above, stable and unstable angina may overlap, and many
CCS patients pass through a period of experiencing unstable
angina.3.1.1.2 Distinction between symptoms caused by epicardial vs. microvascular/vasospastic disease [PDF p 419]
A distinction between symptoms caused by an epicardial stenosis and symptoms caused by microvascular or vasospastic disease cannot be made with reasonable certainty. Reliance on ischaemia testing or depiction of the coronary anatomy is often unavoidable to exclude obstructive CAD, which can be absent in symptomatic patients.13,14 A diagnostic workup for microvascular or vasospastic disease is discussed in section 6 of these Guidelines.
3.1.2 Step 2: Comorbidities and other causes of symptoms
Before any testing is considered, one must assess the patient’s generalhealth, comorbidities, and quality of life. If revascularization is unlikely to be an acceptable option, further testing may be reduced to a clinically indicated minimum and appropriate therapy should be instituted, which may include a trial of antianginal medication even if a diagnosis of CAD has not been fully demonstrated. Non-invasive functional imaging for ischaemia may be an option if there is need to verify the diagnosis (Figure 2).
If the pain is clearly non-anginal, other diagnostic testing may be indicated to identify gastrointestinal, pulmonary, or musculoskeletal causes of chest pain. Nevertheless, these patients should alsoreceive Guideline-based risk-factor modification based on commonly applied risk charts such as SCORE (Systematic COronary Risk Evaluation) (www.heartscore.org*).15
*HeartScore-The interactive tool for predicting and managing the risk of heart attack and stroke from The European Association of Preventive Cardiology: “Our mission is to promote excellence in research, practice, education and policy in cardiovascular health, primary and secondary prevention.”
3.1.3 Step 3: Basic testing [PDF p 419]
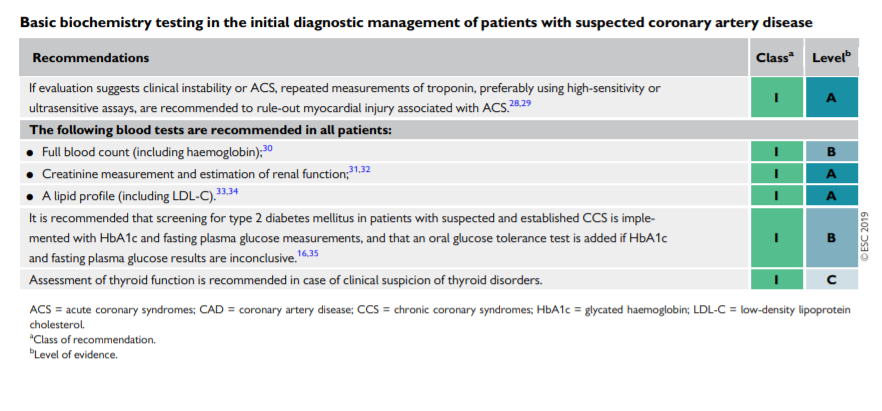
Basic (first-line) testing in patients with suspected CAD includes standard laboratory biochemical testing, a resting ECG, possible ambulatory ECG monitoring, resting echocardiography, and, in selected patients, a chest X-ray. Such testing can be done on an outpatient basis.3.1.3.1 Biochemical tests [PDF p 419]
Laboratory investigations are used to identify possible causes of
ischaemia, to establish cardiovascular risk factors and associated conditions, and to determine prognosis. Haemoglobin as part of a full blood count and—where there is a clinical suspicion of a thyroid disorder—thyroid hormone levels provide information related to possible causes of ischaemia. Fasting plasma glucose and glycated haemoglobin (HbA1c) should be measured in every patient with suspected CAD. If both are inconclusive, an additional oral glucose tolerance test is recommended.16 Knowledge of glucose metabolism is important because of the well-recognized association between diabetes and adverse cardiovascular outcome. Patients with diabetes should be managed according to specific Guidelines.15,16 A lipid profile, including total cholesterol, highdensity lipoprotein cholesterol, low-density lipoprotein cholesterol
(LDL-C), and triglycerides, should also be evaluated in any patient with suspected CAD to establish the patient’s risk profile and ascertain the need for treatment.15,17 To characterize severe dyslipidaemia or follow-up on high triglyceridaemia, fasting values are recommended.17Peripheral artery disease (PAD) and renal dysfunction increase the likelihood of CAD, and have a negative impact on prognosis.1820 Hence, baseline renal function should be evaluated with estimation of the glomerular filtration rate (GFR). It may also be reasonable to measure the uric acid level, as hyperuricaemia is a frequent comorbid condition and may also affect renal function.
If there is a clinical suspicion of CAD instability, biochemical
markers of myocardial injury—such as troponin T or troponin I—should be measured, preferably using high-sensitivity assays, and management should follow the Guidelines for ACS without persistent ST-segment elevation.11 If high-sensitivity assays are employed, low levels of troponin can be detected in many patients with stable angina. Increased troponin levels are associated with adverse outcome2125 and small studies have indicated a possible incremental value in diagnosing CAD,26,27 but larger trials are needed to verify the utility of systematic assessment in patients suspected of CAD. While multiple biomarkers may be useful for prognostication (see section 5), they do not yet have a role in diagnosing obstructive CAD.3.1.3.2 Resting electrocardiogram and ambulatory monitoring [PDF p 420]
The paradigm of diagnosing myocardial ischaemia has, for almost a century, been based on the detection of repolarization abnormalities,
mainly in the form of ST-segment depressions. Thus, the resting 12 lead ECG remains an indispensable component of the initial evaluation of a patient with chest pain without an obviously non-cardiac cause. Two scenarios of clinical evaluation are encountered: (i) a patient without symptoms of chest pain or discomfort, and (ii) a patient with ongoing anginal symptoms.The former situation is far more prevalent and a normal resting
ECG is frequently recorded. However, even in the absence of repolarization abnormalities, an ECG can demonstrate indirect signs of CAD, such as signs of previous MI (pathological Q waves) or conduction abnormalities [mainly left bundle branch block (LBBB) and impairment of atrioventricular conduction]. Atrial fibrillation (AF) is a frequent finding in patients with chest pain (usually atypical). ST segment depression during supraventricular tachyarrhythmias is not predictive of obstructive CAD.3639The ECG can be crucial for diagnosing myocardial ischaemia if
dynamic ST-segment changes are recorded during ongoing angina. The diagnosis of Prinzmetal and vasospastic angina is based on the detection of typical transient ST-segment elevation or depression during an angina attack (usually at rest).Long-term ambulatory ECG monitoring and recording should not be used to replace exercise testing; however, 12 lead ECG monitoring can be considered in selected patients to detect anginal episodes unrelated to physical exercise. Ambulatory ECG monitoring may reveal evidence of silent myocardial ischaemia in patients with CCS, but rarely adds relevant diagnostic or prognostic information that cannot be derived from stress testing.40 ECG changes suggesting ischaemia on ambulatory ECG monitoring are very frequent in
women, but do not correlate with findings during stress testing.41 Most importantly, therapeutic strategies targeting silent ischaemia detected by ambulatory monitoring have not demonstrated clear survival benefits.42,43Place fig10 here when server not busy
Place fig11 here when server not busy