Although thankfully very rare, cardiac arrest in pregnancy can occur. Thus all practioners caring for pregnant women need to review Cardiac arrest in pregnancy: the perimortem cesarean section: A simplified approach to the initial emergency department assessment and management of pregnant patients in cardiac arrest by Dr. Justin Morgenstern
Posted on April 29, 2015 on from First10EM.
In Dr. Morganstern’s post he links to the following resources on perimortem C-Section:
Peri-mortem c-section at EMCrit
Perimortem C-section explained on Intensive Care Network
Emergency Obstetrics: Vertical C-section on YouTube
Resuscitation in Pregnancy from EM in 5
Resuscitation of the pregnant patient: Pearls and Pitfalls on emDocs
https://www.tamingthesru.com/blog/grand-rounds/recap1152014
Added may 2016: https://foamshed.co.uk/peri-mortem-c-section/
And Vimeo has four videos on perimortem C-Section.
Prompt recognition and treatment of maternal distress in pregnancy can often prevent cardiac arrest.
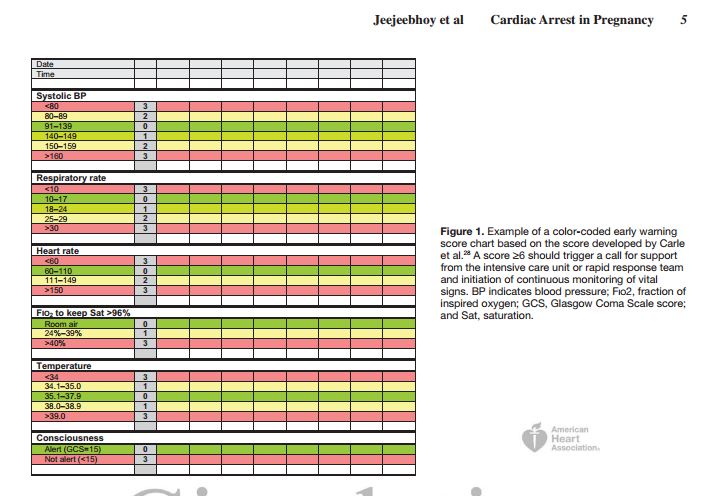
. . . Carle et al28 described . . . the development and validation of a new obstetric score and demonstrated excellent discrimination between survivors and
nonsurvivors for this new score (area under the receiver-operating characteristic curve, 0.995). These scores can be used to monitor patients by clinical use of an early warning score chart (Figure 1) and can accurately identify patients at high risk of mortality, although not specifically mortality resulting from cardiac arrest. Therefore, they are of value in patient management and triage.
The the above and the following is from Circulation 2015 Cardiac Arrest in Pregnancy: A Scientific Statement From the American Heart Association. [PubMed Abstract] [Full Text PDF]:
Severity of Illness and Early Warning Scores [in Pregnant Patients]
The British Center for Maternal and Child Enquiries report
of 2011 (2006–2008 triennium) has stated that timely recognition of pregnant women at risk of potentially life-threatening conditions plays an important role in the appropriate institution of treatment.27 Brief checklists are provided for the identification of a number of conditions, including sepsis, respiratory distress, and neurological complications. Thereport also highlights the potential value of a modified early obstetric warning score. In a more recent publication, using a large British ICU data set, Carle et al28 described the evaluation of several preexisting obstetric early warning scores and the development and validation of a new obstetric score and demonstrated excellent discrimination between survivors and nonsurvivors for this new score (area under the receiver-operating characteristic curve, 0.995). These scores can be used to monitor patients by clinical use of an early warning score chart (Figure 1) and can accurately identify patients at high risk of mortality, although not specifically mortality resulting from cardiac arrest. Therefore, they are of value in patient management and triage.Management of the Unstable Pregnant Patient Rapid response to instability in the pregnant patient is essential for the prevention of cardiac arrest. Maternal hemodynamics must be optimized; hypoxemia must be treated; and intravenous access must be established.
Recommendations29
1. The patient should be placed in a full left lateral decubitus position to relieve aortocaval compression (Class I; Level of Evidence C). 2. Administration of 100% oxygen by face mask to treat or prevent hypoxemia is recommended (Class I; Level of Evidence C). 3. Intravenous access should be established above the diaphragm to ensure that the intravenously administered therapy is not obstructed by the gravid uterus (Class I; Level of Evidence C). 4. Precipitating factors should be investigated and treated (Class I; Level of Evidence C).
27. Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, Harper A, Hulbert D, Lucas S, McClure J, Millward-Sadler H, Neilson J, Nelson-Piercy C, Norman J, O’Herlihy C, Oates M, Shakespeare J, de Swiet M, Williamson C, Beale V, Knight M, Lennox C, Miller A, Parmar D, Rogers J, Springett A. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006–2008: the Eighth Report of the Confidential Enquiries Into Maternal Deaths in the United Kingdom [published correction appears in BJOG. 2014;122:e1]. BJOG. 2011;118(suppl 1):1–203.
28. Carle C, Alexander P, Columb M, Johal J. Design and internal validation of an obstetric early warning score: secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme database. Anaesthesia. 2013;68:354–367. doi: 10.1111/anae.12180.
29. Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, Jeejeebhoy FM, Gabrielli A. Part 12: cardiac arrest in special situations: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care [published correction appears in Circulation. 2011;123:e239 and Circulation. 2011;124:e405]. Circulation. 2010;122(suppl 3):S829–S861. doi: 10.1161/CIRCULATIONAHA.110.971069. 30. Einav S, Shleifer A, Kark JD, Landesberg G,