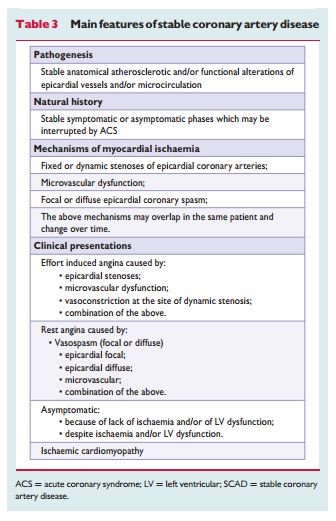
The following section from the 2013 ESC SCAD Guidelines (1) is an outstanding explanation of the principles of diagnostic testing in stable ischemic heart disease (SCAD):
6.2.3 Principles of diagnostic testing (pp 2962+3)
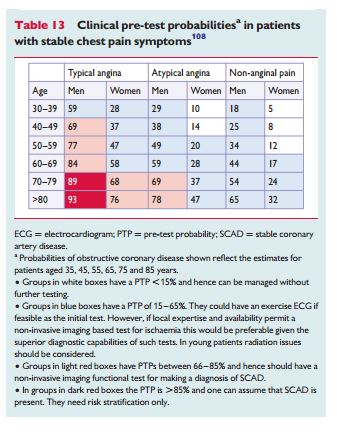
Interpretation of non-invasive cardiac tests requires a Bayesian approach to diagnosis. This approach uses clinicians’ pre-test estimates [termed pre-test probability (PTP)] of disease along with the results of diagnostic tests to generate individualized post-test disease probabilities for a given patient. The PTP is influenced by the prevalence of the disease in the population studied, as well as clinical features (including the presence of CV risk factors) of an individual.90 Major determinants of PTP are age, gender and the nature of symptoms.90
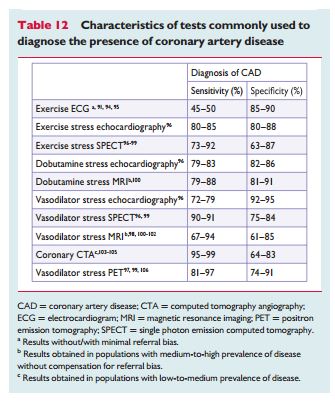
Sensitivity and specificity are often used to describe the accuracy of a given diagnostic method, but they incompletely describe how a test performs in the clinical setting. First, some diagnostic methods mayperform better in some patients than in others—such as coronary computed tomography angiography (CTA), which is sensitive to heart rate, body weight and the presence of calcification. Second, although sensitivity and specificity are mathematically independent from the PTP, in clinical practice many tests perform better in low-risk populations; in the example used above, coronary CTA will have higher accuracy values when low-likelihood populations—which are younger and have less coronary calcium—are subjected to the examination.
Because of the interdependence of PTP (the clinical likelihood that a given patient will have CAD) and the performance of the available diagnostic methods (the likelihood that this patient has disease if the test is positive, or does not have disease if the testis negative),recommendations for diagnostic testing need to take into account the PTP.
Testing may do harm if the number of false test results is higher than the number of correct test results. Non-invasive, imaging-based diagnostic methods for CAD have typical sensitivities and specificities of approximately 85% (Table 12). Hence, 15% of all diagnostic results will be false and, as a consequence, performing no test at all will provide fewer incorrect diagnoses in patients with a PTP below 15% (assuming all patients to be healthy) or a PTP above 85% (assuming all patients to be diseased). In these situations, testing should only be done for compelling reasons. This is the reason why this Task Force recommends no testing in patients with (i) a low PTP ,15% and (ii) a high PTP .85%. In such patients, it is safe to assume that they have (i) no obstructive CAD or (ii) obstructive CAD.The low sensitivity of the exercise ECG—only 50% (despite an excellent specificity of 90%, values obtained from studies avoiding verficationbias)91—is the reason why the number of false test results will become higher than the number of correct test results in populations with a PTP .65%.92 Therefore, this Task Force recommends not employing the exercise stress test in such higher-risk populations for diagnostic purposes. However, the test may nevertheless provide valuable prognostic information in such populations.93
In this new version of the Guidelines, more weight is given to testing based systematically on consideration of pre-test probabilities.107 This Task Force selected the most recent estimates of CAD prevalences as the basis of these Guidelines’ clinical algorithm,108 as discussed in the web addenda and shown in Table 13. The web addenda also contains more information about changes from the previous Stable Angina guidelines of the ESC and the reasons why ECG exercise testing was kept in the algorithm.
If the pain is clearly non-anginal other diagnostic testing may be indicated to identify gastrointestinal, pulmonary or musculoskeletal causes of chest pain (Figure 1). Nevertheless, these patients should also receive risk factor modification based on commonly applied risk charts such as SCORE (https://www.heartscore.org/Pages/welcome. aspx) or the Framingham risk score (https://hp2010.nhlbihin.net/atpiii/ calculator.asp). Patients with suspected SCAD, in whom comorbidities make revascularization inadvisable, should be treated medically but pharmacologic stress imaging may be an option if it appears necessary to verify the diagnosis. Patients with a reduced left ventricular ejection fraction (LVEF) of < 50% and typical angina are at high risk for cardiovascular events (see later in the text) and they should be offered ICA without previous testing (see Figure 1).
Patients in whom anginal pain may be possible but who have a very low probability of significant CAD < 15% should have other cardiac causes of chest pain excluded and their CV risk factors adjusted, based on risk score assessment.37 No specific non-invasive stress testing should be performed.92 In patients with repeated, unprovoked attacks of chest pain only at rest, vasospastic angina should be considered and diagnosed, and treated appropriately (see below). Patients with an intermediate PTP of 15–85% should undergo further non-invasive testing. In patients with a clinical PTP .85%, the diagnosis of CAD should be made clinically and further testing will not improve accuracy. Further testing may, however, be indicated for stratification of riskof events, especially if no satisfactory control of symptoms is possible with initial medical therapy (Figure 1). In patients with severe angina at a low level of exercise and those with a clinical constellation indicating a high event risk,109 proceeding directly to ICA is a reasonable option. Under such circumstances, the indication for revascularization should depend on the result of intraprocedural fractional flow reserve (FFR) testing when indicated.110
The very high negative predictive value of acoronaryCTA showing no stenoses can reassure patients and referring physicians that instituting medical therapy and not proceeding to further testing or invasive therapies is agoodstrategy.This makesthe testpotentially useful, especially for patients at low intermediate PTPs (Figure 2). One should remember that there may be overdiagnosis of stenoses in patients with Agatston scores .400,104,105 and it seems prudent to call a coronary CTA ‘unclear’ if severe focal or diffuse calcifications prevent an unambiguous identification of the vessel lumen (see Figure 2). To obtain optimal results, published professional standards need to be meticulously adhered to.111 With these caveats in mind, coronary CTA may be considered to be an alternative to ischaemia testing, especially in patients with chest pain symptoms at intermediate PTPs lower than 50%.112
Resources:
(1) 2013 ESC guidelines on the management of stable coronary artery disease. [Full Text PDF] European Heart Journal (2013) 34, 2949–3003.
(2) 2013 ESC guidelines on the management of stable coronary artery disease—addenda. [Full Text PDF] The European Society of Cardiology 2013.