In this month’s Circulation [May 2017], there is an article recommending that we consider screening for atrial fibrillation to prevent stroke. (Ref 1)
It does need to be recognized that AF-SCREEN (the group writing this article) received financial support from pharmaceutical companies and medical device companies with a financial interest in the treatment or diagnosis of atrial fibrillation. In addition, a number of the authors have received significant financial support from those same companies.
With the above in mind, what follows are excerpts from the article:
Abstract:
Approximately 10% of ischemic strokes are associated with atrial fibrillation (AF) first diagnosed at the time of stroke. Detecting asymptomatic AF would provide an opportunity to prevent these strokes by instituting appropriate anticoagulation. . . . These key points [in the report] emphasize that screen-detected AF found at a single timepoint or by intermittent ECG recordings over 2 weeks is not a benign condition and, with additional stroke factors, carries sufficient risk of stroke to justify consideration of anticoagulation. With regard to the methods of mass screening, handheld ECG devices have the advantage of providing a verifiable ECG trace that guidelines require for AF diagnosis and would therefore be preferred as screening tools. Certain patient groups, such as those with recent embolic stroke of uncertain source (ESUS), require more intensive monitoring for AF. . . . Based on current knowledge, this white paper provides a strong case for AF screening now while recognizing that large randomized outcomes studies would be helpful to strengthen the evidence base.
Risk of Stroke and Death in Untreated Screen Detected
AFNo data specifically address the risk of stroke and death in untreated screen-detected AF in the general population. The closest approximation includes cohort studies of individuals with AF detected incidentally in the absenceof symptoms.
In 5555 patients with asymptomatic clinical AF detected incidentally in general practice, the adjusted stroke rate in the 1460 untreated patients was 4% and all-cause mortality 7% over 1.5 years of follow-up compared with 1% and 2.5%, respectively, in matched controls without AF.22,23 In the EORP AF registry (Eurobservational Research Programme), mortality at 1 year was ˃2-fold higher in asymptomatic versus symptomatic AF (9.4% versus 4.2%, P<0.0001).24 In the Belgrade AF study,
survival free of AF progression or ischemic stroke was worse in those with an asymptomatic presentation.25Key Point 1
Screen-detected AF as found on single-timepoint screening or intermittent 30-second recordings over 2 weeks is not a benign condition and, with additional stroke risk factors, carries sufficient risk of stroke to justify consideration of screening and therapy to prevent stroke.
Response to Treatment of Screen-Detected AF
In the cohort study of 5555 asymptomatic patients with AF detected incidentally in general practice, OAC therapy (n=2492) compared with no antithrombotic therapy (n=1460) was associated with significantly reduced adjusted risk of stroke from 4% to 1% and death from 7% to 4% in only 1.5 years, suggesting that screen-detected AF may respond similarly.22,23
Screen-detected AF (single-timepoint screening or patient initiated recording) is likely to have the same response to OAC therapy as incidentally detected AF and symptomatic AF, with significant reduction in stroke and death.
Role of AF in Ischemic Stroke
In stroke registries, at least a third of patients with ischemic
stroke have either previously known31,32 or newly detected AF at the time of stroke.33 Stroke was the first manifestation of AF in ˃25% of AF-related strokes.31 The association with AF is even higher if prolonged poststroke external or implanted monitoring is performed.34,35 In theSwedish Riks-Stroke register of ˃94000 ischemic strokes, ≈9% were associated with previously unknown AF and 20% with known but undertreated AF,31,32 whereas in a global registry 10% were caused by previously unknown AF.36It is likely that both unknown and undertreated AF contribute
to a substantial proportion of all strokes, which could be prevented by screening strategies. Regarding the role of AF in stroke, it is likely that AF is both a risk factor and a strong risk marker for stroke.Which Patients or Individuals to Screen?
If the screening procedure is inexpensive and easy to
use (eg, pulse palpation or single-timepoint handheld devices),47,48 screening can be nonselective and just agebased.
A threshold ≥65 years of age (a CHA2DS2-VASc score of at least 1 in a male and 2 in a female) will detect undiagnosed AF in 1.4% in clinic or population settings,3 in which case European Society of Cardiology (ESC)guidelines recommend that OAC be considered (Class IIa); OACs are recommended (Class I) for a score of 2 in a male or 3 in a female.30 Opportunistic screening in all patients contacting the health system ≥65 years of age
has been adopted in the ESC AF guidelines30 but might be more efficient if an older age threshold is chosen or an additional stroke risk factor is required.49 Superiority over a simple age-based criterion, however, needs to be proven.Key Point 2
Single-timepoint screening of people ≥65 years of age in
the clinic or community appears justified based on yield
of screening and likely cost-effectiveness. For those ˃75
years of age or in younger age groups at high risk of AF
or stroke, 2 weeks of twice-daily intermittent AF screening
may be warranted.Ischemic Stroke and ESUS
Randomized controlled trials and observational studies have established the effectiveness of ECG monitoring after stroke for improving AF detection (number needed to screen=8–14), 33,52 with longer monitoring durations increasing AF detection probability. ECG monitoring after stroke is likely cost-effective.53,54 However, randomized controlled trials have not been powered to assess the effect of prolonged ECG monitoring on stroke or mortality.
After an acute ischemic stroke/transient ischemic attack
in patients not known to have AF and without contraindications
to OACs, a tiered AF ECG monitoring approach is advised.
ESC guidelines recommend ≥72 hours ECG monitoring
in all stroke survivors,30 but more research is required
to identify non-ESUS subgroups benefitting most from more
prolonged monitoring.Key Point 3
Long-term continuous rhythm monitoring using either
external or implanted devices or extended intermittent patient-activated recordings may diagnose clinically important AF in individuals with recent ESUS.Overview of Screening Methods
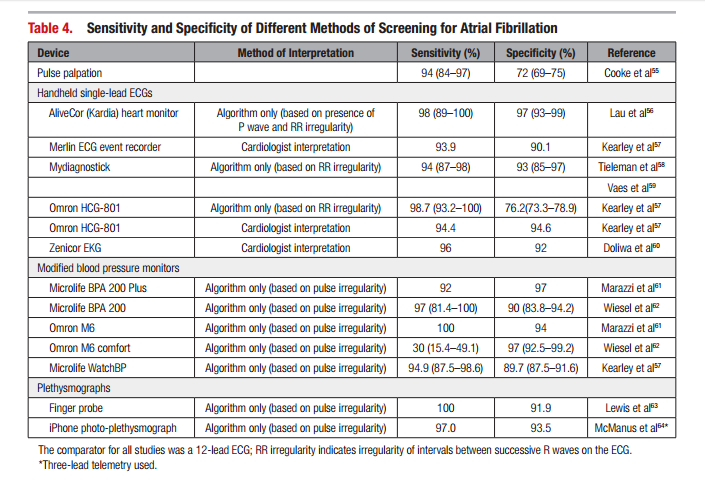
Innovation in technology has produced new screening
devices that improve feasibility and cost-effectiveness of widespread screening (Table 4). These devices are recognized as valid for AF detection by the European Primary Care Cardiovascular Society66 and could be used to complement traditional screening by pulse palpation.A range of handheld devices produce diagnostic quality lead 1 single-lead ECGs, most with automated algorithms more accurate than pulse palpation (sensitivity 94% to 99% and specificity 92% to 97%).57,58,60,71 These devices have been widely used for single-timepoint AF screening.48,58 Repeated handheld ECG recordings over 14 to 28 days have diagnostic accuracy equivalent to standard event recorders, superior to 12-lead ECG and 24-hour Holter for paroxysmal AF,5,60,72 and have been used successfully in large-scale AF screening studies.4,5 Although single-lead ECGs may not always show P-waves, the advantages outweigh this limitation. The accepted arbitrary episode duration for defining AF is 30 seconds.
Continuous monitoring coupled with a diagnostic algorithm
will detect paroxysmal AF more effectively than repeated
patient-activated devices, although the prognostic significance of brief episodes is uncertain. Continuous monitoring can be accomplished by noninvasive devices (eg, prolonged Holter monitoring, a wearable nonadhesive dry-electrode belt,73 or a wearable-patch: feasible for 2 to 4 weeks74 and superior to 24-hour Holter).Key Point 4
Mass or opportunistic screening for AF can be accomplished
by pulse palpation; oscillometric (blood pressure) or photoplethysmographic (smartphone camera) devices;and handheld ECG devices providing a rhythm strip. Because
ECG confirmation is mandated by guidelines for the diagnosis of AF, handheld ECG devices have the advantage of providing a verifiable ECG trace and would therefore be the preferred screening tool. Prolonged continuous ECG monitoring with external or subcutaneous recorders will diagnose more paroxysmal AF but requires further evaluation: cost-effectiveness will be limited by expense and detection of AF with lower absolute stroke risk.Key Point 5
The setting for AF screening needs to be individualized
according to country- and healthcare system-specific
requirements and resources and must be linked to a
pathway for appropriate diagnosis and management for
screening to be effective. Settings that have been used effectively
include some that are community-based and others
based in primary care, specialist practices, or general
or specialist clinics. Primary care and outpatient clinics
have the advantage of offering a direct link with treatment
and a potentially sustainable workflow (see online-only
Data Supplement for country-specific considerations).Current Guidelines
The ESC recommends opportunistic pulse-taking in all patients ≥65 years of age or in high-risk subgroups, followed by an ECG if irregular, to allow for timely AF detection.30,89 Pulse taking in practice is recommended by the National Institute for Health and Care Excellence (UK) guidelines but only for symptoms. However, the new 2016 ESC guideline30 also includes an ECG rhythm strip as an alternative to pulse palpation, at least 72
hours of ECG monitoring after a transient ischemic attack or stroke with additional longer term monitoring considered, and consideration of systematic screening in patients ≥75 years of age or those at high stroke risk. An additional recommendation is to interrogate CIEDs for atrial high-rate episodes and, if detected, prompt further ECG monitoring to document AF before initiating therapy.The American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines1 make no recommendation on the topic of screening but do state that early detection and treatment of asymptomatic AF before the first complications occur is a recognized priority for the prevention of stroke.
Guidelines address specific subgroups where screening may be worthwhile, including high-risk patients (eg, poststroke, ˃75 years of age), in whom prolonged monitoring is more likely to detect AF.
Reference:
(1) Screening for Atrial Fibrillation: A Report of the AF-SCREEN International Collaboration [PubMed Abstract] [Full Text HTML] [Download PDF]. Circulation. 2017 May 9;135(19):1851-1867. doi: 10.1161/CIRCULATIONAHA.116.026693