All of what follows are figures, tables, and quotes from the 2009 European Society of Cardiology (ESC) Syncope Guidelines*:
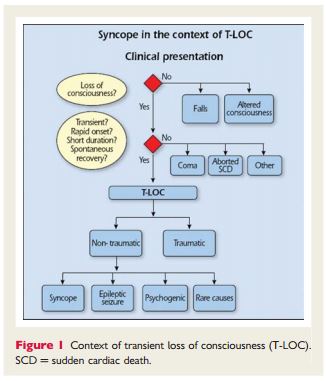
“Syncope is a Transient Loss of Conciousness (T-LOC) due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery.”
“This definition of syncope differs from others by including the cause of unconsciousness, i.e. transient global cerebral hypoperfusion. Without that addition, the definition of syncope becomes wide enough to include disorders such as epileptic seizures and concussion. In fact, the definition then becomes that of T-LOC, a term purposely meant to encompass all disorders characterized by self-limited loss of consciousness (LOC), irrespective of mechanism (Figure 1). By distinguishing both T-LOC and syncope, the present definition minimizes conceptual and diagnostic confusion. In the past, papers often did not define syncope, or did so in different ways.2 Syncope was sometimes used for T-LOC, thus including epileptic seizures and even stroke in ‘syncope’. This source of confusion may still be found in the literature.3,4 ”
“In some forms of syncope there may be a prodromal period in which various symptoms (e.g. lightheadedness, nausea, sweating, weakness, and visual disturbances) warn that syncope is imminent. Often, however, LOC occurs without warning. An accurate estimate of the duration of spontaneous episodes is rarely obtained. Typical syncope is brief. Complete LOC in reflex syncope lasts no longer than 20 s in duration. However, syncope may rarely be longer, even as much as several minutes.5 In such cases, the differential diagnosis between syncope and other causes of LOC can be difficult. Recovery from syncope is usually accompanied by almost immediate restoration of appropriate behaviour and orientation. Retrograde amnesia, although believed to be uncommon, may be more frequent than previously thought, particularly in older individuals. Sometimes the post-recovery period may be marked by fatigue.5”
“The adjective ‘pre-syncopal’ is used to indicate symptoms and signs that occur before unconsciousness in syncope, so its meaning is literal when used in this context and making it a synonym of ‘warning’ and ‘prodromal’. The noun ‘pre-syncope’ or ‘near-syncope’ is used often to describe a state that resembles the prodrome of syncope but which is not followed by LOC; doubts remain as to whether the mechanisms involved are the same as in syncope.”
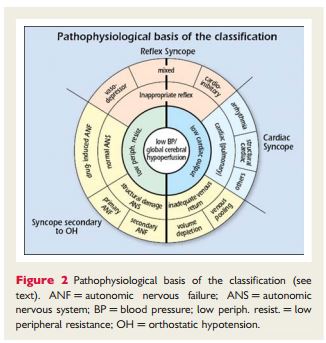
“Figure 2 shows how pathophysiology underpins the classification, with low BP/global cerebral hypoperfusion at the centre, adjacent to low or inadequate peripheral resistance and low CO.”
“Table 4 provides a pathophysiological classification of the principal causes of syncope, emphasizing large groups of disorders with a common presentation associated with different risk profiles. A distinction along pathophysiological lines centres on a fall in systemic blood pressure (BP) with a decrease in global cerebral blood flow as the basis for syncope. A sudden cessation of cerebral blood flow for as short as 6–8 s has been shown to be sufficient to cause complete LOC. Experience from tilt testing showed that a decrease in systolic BP to 60 mmHg or lower is associated with syncope.6 Systemic BP is determined by cardiac output (CO) and total peripheral vascular resistance, and a fall in either can cause syncope, but a combination of both mechanisms is often present, even if their relative contributions vary considerably. Figure 2 shows how pathophysiology underpins the classification, with low BP/global cerebral hypoperfusion at the centre, adjacent to low or inadequate peripheral resistance and low CO.”
“A low or inadequate peripheral resistance can be due to inappropriate reflex activity depicted in the next ring, causing vasodilatation and bradycardia manifesting as vasodepressor, mixed, or cardioinhibitory reflex syncope, seen in the outer ring. Other causes of a low or inadequate peripheral resistance are functional and structural impairments of the autonomic nervous system (ANS) with drug-induced, primary and secondary autonomic failure (ANF) in the outer ring. In ANF, sympathetic vasomotor pathways are unable to increase total peripheral vascular resistance in response to the upright position. Gravitational stress, in combination with vasomotor failure, results in venous pooling of blood below the diaphragm, causing a decrease in venous return and consequently in CO.”
“The causes of transient low CO are 3-fold. The first is a reflex causing bradycardia, known as cardioinhibitory type of reflex syncope. The second is cardiovascular causes, due to arrhythmia and structural disease including pulmonary embolism/hypertension. The third is inadequate venous return, due to volume depletion or venous pooling. The three final mechanisms, reflex, secondary to orthostatic hypotension (OH), and cardiovascular, are shown outside the rings in Figure 2; reflex syncope and OH span the two main pathophysiological categories.”
1.2.2.1 Reflex syncope (neurally mediated syncope)
“Reflex syncope traditionally refers to a heterogeneous group of conditions in which cardiovascular reflexes that are normally useful in controlling the circulation become intermittently inappropriate, in response to a trigger, resulting in vasodilatation and/or bradycardia and thereby in a fall in arterial BP and global cerebral perfusion.7”
“Reflex syncope is usually classified based on the efferent pathway most involved, i.e. sympathethic or parasympathetic. The term ‘vasodepressor type’ is commonly used if hypotension, due to a loss of upright vasoconstrictor tone, predominates. ‘Cardioinhibitory’ is used when bradycardia or asystole predominate, and ‘mixed’ is used if both mechanisms are present.”
“Reflex syncope may also be classified based on its trigger, i.e. the afferent pathway (Table 4). It must be recognized that this is a simplification, because many different mechanisms can be present in the context of a specific situation, such as micturition or defaecation syncope. The triggering situations vary considerably in and between individual patients. In most cases the efferent pathway does not depend strongly on the nature of the trigger [e.g. both micturition syncope and vasovagal syncope (VVS) may present as cardioinhibitory or vasodepressor syncope]. Knowing the various triggers is clinically important, as recognizing them may be instrumental in diagnosing syncope:
-
‘Vasovagal’ syncope (VVS), also known as the ‘common faint’, is mediated by emotion or by orthostatic stress. It is usually preceded by prodromal symptoms of autonomic activation (sweating, pallor, nausea).
-
‘Situational’ syncope traditionally refers to reflex syncope associated with some specific circumstances. Post-exercise syncope can occur in young athletes as a form of reflex syncope as well as in middle-aged and elderly subjects as an early manifestation of ANF before they experience typical OH.
-
‘Carotid sinus’ syncope deserves special mention. In its rare spontaneous form it is triggered by mechanical manipulation of the carotid sinuses. In the more common form no mechanical trigger is found and it is diagnosed by carotid sinus massage (CSM).8
-
The term ‘atypical form’ is used to describe those situations in which reflex syncope occurs with uncertain or even apparently absent triggers. The diagnosis then rests less on history taking alone, and more on the exclusion of other causes of syncope (absence of structural heart disease) and on reproducing similar symptoms with tilt testing. Such less clear presentations may overlap with clear-cut occurrences within patients.”
“The classical form of VVS usually starts in young subjects as an isolated episode and is distinct from other forms, frequently with an atypical presentation, starting in old age often associated with cardiovascular or neurological disorders possibly displaying orthostatic or post-prandial hypotension. In these latter forms, reflex syncope appears as an expression of a pathological process, mainly related to impairment of the ANS to activate compensatory reflexes, so there is an overlap with ANF.9“
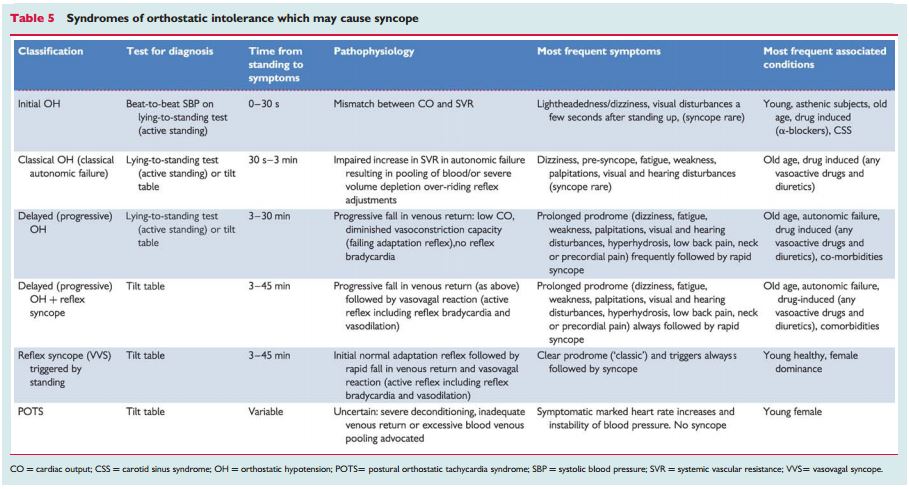
“A comparison with other conditions causing syncope in the standing position is presented in Table 5.”
1.2.2.2 Orthostatic hypotension and orthostatic intolerance syndromes
“In contrast to reflex syncope, in ANF sympathetic efferent activity is chronically impaired so that vasoconstriction is deficient. Upon standing, BP falls and syncope or pre-syncope occurs. OH is defined as an abnormal decrease in systolic BP upon standing.”
“Strictly from a pathophysiological point of view there is no overlap between reflex syncope and ANF, but the clinical manifestations of the two conditions frequently overlap, sometimes making differential diagnosis difficult. ‘Orthostatic intolerance’ refers to symptoms and signs in the upright position due to a circulatory abnormality. Syncope is one symptom, and others are: (i) dizziness/lightheadedness, pre-syncope; (ii) weakness, fatigue, lethargy; (iii) palpitations, sweating; (iv) visual disturbances (including blurring, enhanced brightness, tunnel vision); (v) hearing disturbances (including impaired hearing, crackles, and tinnitus); and (vi) pain in the neck (occipital/paracervical and shoulder region), low back pain, or precordial pain.10,11“
“Various clinical syndromes of orthostatic intolerance are given in Table 5. Among these, the forms of reflex syncope in which orthostatic stress is the main trigger are also included.
-
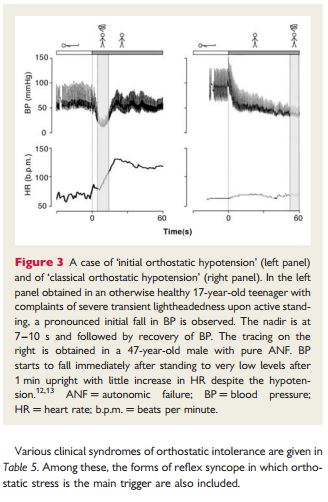
‘Classical OH’ is a physical sign defined as a decrease in systolic BP ≥20 mmHg and in diastolic BP ≥10 mmHg within 3 min of standing12(Figure 3), described in patients with pure ANF, hypovolaemia, or other forms of ANF.
-
‘Initial OH’13 is characterized by a BP decrease immediately on standing of >40 mmHg.13 BP then spontaneously and rapidly returns to normal, so the period of hypotension and symptoms is short (<30 s) (Figure 3).
-
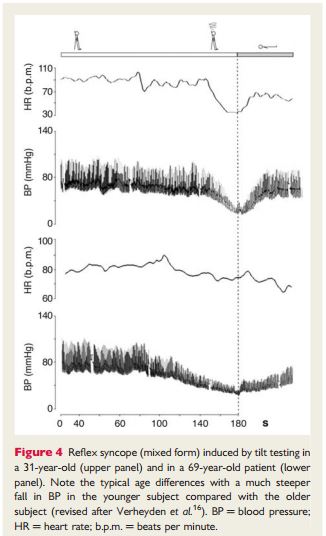
‘Delayed (progressive) OH’14–16 is not uncommon in elderly persons. It is attributed to age-related impairment of compensatory reflexes and stiffer hearts in the elderly sensitive to a decrease in preload.16 Delayed OH is characterized by a slow progressive decrease in systolic BP on assuming erect posture. The absence of a bradycardiac reflex (vagal) differentiates delayed OH from reflex syncope. Delayed OH may, however, be followed by reflex bradycardia, where, in the elderly, the fall in BP is less steep than in the young (Figure 4).
-
‘Postural orthostatic tachycardia syndrome’ (POTS). Some patients, mostly young women, present with severe complaints of orthostatic intolerance, but not syncope, with very marked heart rate (HR) increases [>30 beats per minute (b.p.m.) or to >120 b.p.m.] and instability of BP.17 POTS is frequently associated with chronic fatigue syndrome. The underlying pathophysiology remains to be determined.”
1.2.2.3 Cardiac syncope (cardiovascular)
Arrhythmia
“Arrhythmias are the most common cardiac causes of syncope. They induce haemodynamic impairment, which can cause a critical decrease in CO and cerebral blood flow. Nonetheless, syncope often has multiple contributory factors, including HR, type of arrhythmia (supraventricular or ventricular), left ventricular function, posture, and adequacy of vascular compensation. The latter include baroreceptor neural reflexes as well as responses to OH induced by the arrhythmia.18,19 Regardless of such contributing effects, when an arrhythmia is the primary cause of syncope, it should be specifically treated.”
“In intrinsic sick sinus syndrome, the sinoatrial node is damaged, because of either abnormal automaticity or sinoatrial conduction abnormalities. In this situation syncope is due to long pauses caused by sinus arrest or sinoatrial block and a failure of escape mechanism. These pauses are most frequently encountered when an atrial tachyarrhythmia suddenly stops (brady-tachy syndrome).19“
“As a rule, the more severe forms of acquired atrioventricular (AV) block (Mobitz II block, ‘high grade’, and complete AV block) are most closely related to syncope. In these cases, the cardiac rhythm may become dependent on subsidiary or escape (often unreliable) pacemaker sites. Syncope occurs because the delay before these pacemakers begin to ‘fire’ is long. In addition these subsidiary pacemaker sites typically have relatively slow rates (25–40 b.p.m.). Bradycardia also prolongs repolarization and predisposes to polymorphic ventricular tachycardia (VT), especially of the torsade de pointes type.”
“Syncope or near-syncope occurs at the onset of paroxysmal tachycardia, before vascular compensation develops.18,19 Consciousness is, in general, restored before tachycardia terminates. If haemodynamics remain inadequate due to tachycardia, unconsciousness is maintained. Recovery is then not spontaneous, no longer classified as syncope, and constitutes cardiac arrest.”
“Several drugs can cause brady- and tachyarrhythmias. Many antiarrhythmic drugs can cause bradycardia as a consequence of their specific effect on sinus node function or AV conduction. Syncope due to torsade de pointes is not uncommon, especially in women, and is caused by drugs prolonging the QT interval. It is particulary frequent in patients affected by the long QT syndrome. QT-prolonging drugs belong to different categories, i.e. antiarrhythmics, vasodilators, psychotropics, antimicrobials, non-sedating antihistamines, etc. Much has been learned about the inherited long QT syndrome through the collection of data in an international registry. Far less is known about the drug-induced syndrome because of the absence of a comprehensive database. Only 1% of serious adverse reactions to drugs are ever reported to the Food and Drug Administration (FDA).20,21 Owing to the wide variety of these drugs and the need for continuous updating, this TF recommends accessing a dedicated website (www.qtdrugs.org).”
Structural disease
“Structural cardiovascular diseases can cause syncope when circulatory demands outweigh the impaired ability of the heart to increase its output.Table 4 lists the most frequent cardiovascular diseases that can cause syncope. Syncope is of great concern when it is associated with conditions in which there is fixed or dynamic obstruction to left ventricular outflow. The basis for the faint is inadequate blood flow due to mechanical obstruction. Nonetheless, in several cases, syncope is not solely the result of restricted CO, but may be in part due to an inappropriate reflex or OH. For instance, in the setting of valvular aortic stenosis, syncope is not solely the result of restricted CO, but may be in part due to inappropriate reflex vasodilation and/or primary cardiac arrhythmia. Furthermore, arrhythmias, particularly atrial fibrillation, are frequently important causes of faint. Thus, the mechanism of syncope may be multifactorial. To recognize the heart as the cause of the problem is justified by the need to correct the underlying structural disease, when possible.”
1.3.1 Prevalence of syncope in the general population
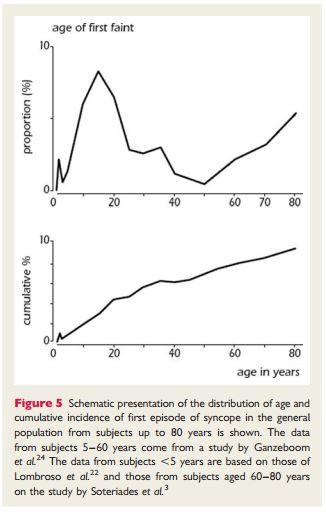
“Syncope is common in the general population and the first episode presents at characteristic ages (Figure 5). About 1% of toddlers may have a form of VVS.22,23 There is a very high prevalence of first faints in patients between 10 and 30 years, with a peak of ∼47% in females and 31% in males around the age of 15.24,25 Reflex syncope is by far the most common cause. In contrast, the frequency of epileptic seizures in a similar young age group is much lower (<1%) and syncope from cardiac arrhythmia is even less common.26 In a cohort study, only 5% of adults in the community have a first syncope over the age of 40 years. The majority have experienced reflex-mediated episodes as teenagers and adolescents.26 Finally, there appears to be a peak above the age of 65 years in both males and females. In the Framingham study the incidence of syncope shows a sharp rise after the age of 70 years, from 5.7 events per 1000 person-years in men aged 60–69, to 11.1 in men aged 70–79.3,26 However, in older adults and elderly subjects (>60 years) the lifetime cumulative incidence of syncope becomes increasingly difficult to obtain due to recollection bias of fainting episodes decades ago.26,27“
1.3.2 Referral from the general population to medical settings
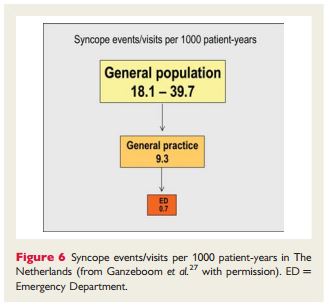
“A very small fraction of patients with syncope in the general population, present in any clinical setting (Figure 6). In the Framingham offspring study, 44% of the participants (mean age 51 years, range 20–96 years) with an episode of LOC reported that they did not seek medical advice.3The proportion of patients not seeking medical evaluation in the younger population is much higher.25,26“
“In The Netherlands the prevalence of the complaint of fainting in general practice is estimated at 9.3 per 1000 encounter-years.26,28 Recent studies report a remarkably constant frequency of syncope in community-based Emergency Departments (EDs) in Europe, with an incidence of ∼1% of all attendances (range 0.9–1.7%).29–35“
1.3.3 Prevalence of the causes of syncope
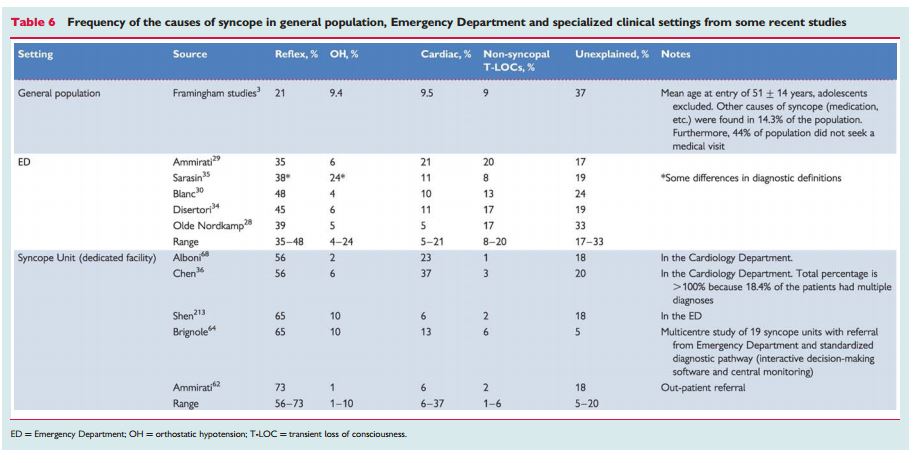
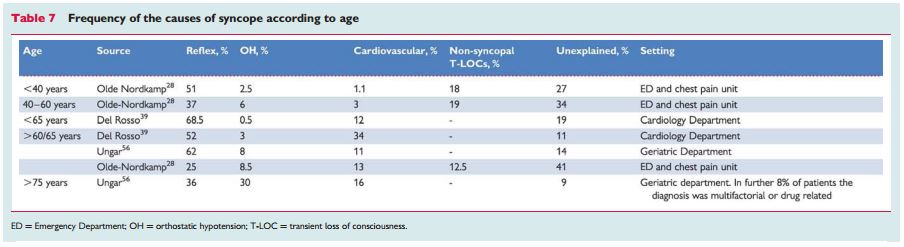
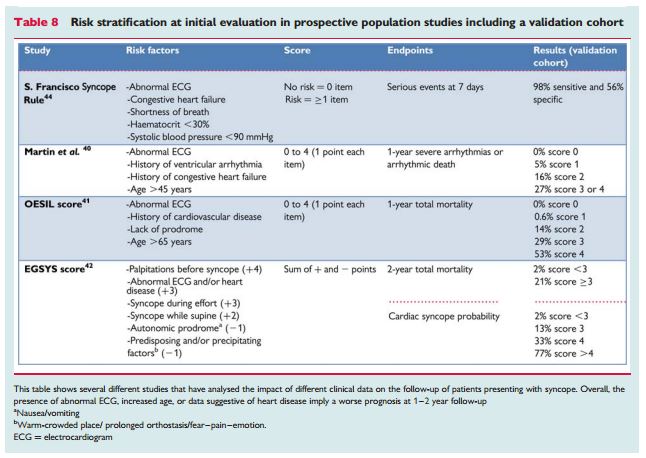
“The prevalence of the causes of syncope is different depending on the clinical settings in which the patient is evaluated (Table 6) and the age of the patients (Table 7). Furthermore, other differences depend on diagnostic definitions, geographical factors, and local care pathways, making a comparison between different studies difficult.”
“Some general comments are however possible:
-
Reflex syncope is the most frequent cause of syncope in any setting.
-
Syncope secondary to cardiovascular disease is the second most common cause. The number of patients with a cardiovascular cause varies widely between studies; higher frequencies are observed in emergency settings mainly in older subjects, and in settings oriented toward cardiology.
-
In patients <40 years OH is a rare cause of syncope; OH is frequent in very old patients.
-
Non-syncopal conditions, misdiagnosed as syncope at initial evaluation, are more frequent in emergency referrals and reflect the multifactorial complexity of these patients.
-
The high unexplained syncope rate in all settings justifies new strategies for evaluation and diagnosis.”
“While in the young reflex syncope is by far the most frequent cause of T-LOC, in the elderly multiple causes are often present and the medical history may be less reliable than in the young.36–39“
1.4.2 Recurrence of syncope and risk of physical injury
“In population studies, approximately one-third of patients have recurrence of syncope in 3 years follow-up. The number of episodes of syncope during life is the strongest predictor of recurrence. For example, in patients with uncertain diagnosis, low risk and age >40 years, a history of one or two episodes of syncope during life predicted a recurrence of 15 and 20% after 1 and 2 years, respectively, whereas a history of three episodes of syncope during life predicted a recurrence of 36 and 42% after 1 and 2 years, respectively.53“
“A psychiatric disease and age <45 years are also associated with higher rates of pseudosyncope. Conversely, gender, tilt test response, severity of presentation, and presence or absence of structural heart disease have minimal or absent predictive value.1,53
“Major morbidity, such as fractures and motor vehicle accidents, were reported in 6% of patients, and minor injury, such as laceration and bruises, in 29%. Recurrent syncope is associated with fractures and soft tissue injury in 12% of patients.1 In patients presenting to an ED, minor trauma were reported in 29.1% and major trauma in 4.7% of cases; the highest prevalence (43%) was observed in older patients with carotid sinus syndrome (CSS).54“
“Morbidity is particulary high in the elderly and ranges from loss of confidence, depressive illness, and fear of falling, to fractures and subsequent institutionalization.55,56
The diagnosis of syncope from the 2009 ESC Syncope Guidelines is covered in the next post.
________________________________________________________________
Resources
*Guidelines for the diagnosis and management of syncope (version 2009) (PDF) The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC)
AHA/ACCF Scientific Statement on the Evaluation of Syncope AHA Scientific Statements. Circulation 2006; 113: 316-327.
ACCA Clinical Decision-Making Toolkit
A key instrument for quality improvement and clinical training. Acute Cardiovascular Care Association: a community of the European Society of Cardiology for all clinicians involved in the acute care of cardiovascular patients.
CRITICAL CONCERNS IN SPORTS MEDICINE
Audio-Digest Family Practice
Volume 62, Issue 12
March 28, 2014
Screening Young Athletes for Heart Conditions (Summary) – John R. Dylewski, MD
Postconcussion Syndrome: A Clinical Update – Chantel Debert, MD
Resources for Non-invasive Hemodynamic Monitoring
Real-time Continuous Beat-to-Beat Noninvasive Blood Pressure (NIBP100D). This is a commercially available system and on the company’s website is a PDF article, Continuous non-invasive arterial pressure shows high accuracy in comparison to invasive intra-arterial blood pressure measurement. Unfortunately, it’s usefulness is seriously compromised because it is undated and apparently not published in any journal.
Noninvasive continuous hemodynamic monitoring J Clin Monit Comput. Aug 2012; 26(4): 267–278. Published online Jun 14, 2012. doi: 10.1007/s10877-012-9375-8. The above link is to the free full-text article archived in PubMed Central (PMC) [PMC has a number of unique advantages for researcher and clinician].
Resources for the Prevention of Sudden Death
Guidelines for Risks and Prevention of Sudden Cardiac Death (JCS 2010) –Digest Version – JCS Joint Working Group. Circulation Journal, Official Journal of the Japanese Circulation Society.
American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008 Sep 30;118(14):1497-1518. (Full Text HTML) (Full Text PDF).
ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death–executive summary. Eur Heart J. 2006 Sep;27(17):2099-140.
ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). European Heart Journal (2006) 8, 746-837.