Summary of Ultrasound For Postmenopausal Bleeding YouTube video [Reference (1)]:
Postmenopausal bleeding is endometrial cancer until proven otherwise. A negative blind endometrial biopsy does not rule out endometrial cancer. The speaker recommends that a woman with postmenopausal bleeding recieve a transvaginal ultrasound which if technically adequate and normal can rule out endometrial cancer.
Vaginal bleeding is the presenting signs in almost all cases [of endometrial cancer.
Incidence of endometrial cancer in studies of women with postmenopausal bleeding ranges from 1 – 14% (most are 3 – 7%).
Newest ACOG Guidance: July 2012
- References the fact that when cancer involves less than 50% of the endometrial cavity blind biopsy is not as reliable as previously thought.
- “A blind endometrial biopsy that does not show cancer or complex atypical hyperplasia cannot be considered an endpoint.”
Transvaginal Ultrasound
- Consistently, the finding of a thin distinct echo </= 4 to 5 mm was shown to effectively exclude significant tissue in postmenopausal women with bleeding.
Transvaginal U/S Validation of Early Studies
- For an Endometrial thickness of on Transvaginal U/S </= 4 mm incidence of malignancy 1 in 917
Is Endometrial Biopsy even still necessary?
- False negative rate to exclude cancer of TV U/S </= signficantly less than a “negative” blind biopsy.
- In one study of endometrial thickness < 5 mm: only 82% were successfully completed, and of those only 27% gave enough tissue to be adequate for a diagnosis.
- ACOG Committee Opinion (2/09, reaffirmed 2011) “When transvaginal ultrasound is performed for postmenopausal bleeding and Endometrial thickness </= is found Endometrial sampling is not required.”
- Occasionally the endometrial echo is not sufficiently visualized for technical reasons (coexisting fibroids, previous surgery, marked obesity, axial uterus, adenomyosis
- In such cases saline infusion sonohysterography (the installation of 10 – 20 cc) will distinguish:
- No pathology (was unable to appreciate for technical reasons)
- Global Process (Blind Biopsy Reliable)
- Focal Process (Requires Direct Vision Biopsy under Hysteroscopy)
So [above] we put some fluid into the uterine cavity and it distends the back and front wall and we can see that this woman has absolutely no abnormality. [No. 1 – No pathology. No further evaluation needed].
[Above] This woman has a polyp and so if you did a blind biopsy and you got a piece of the back wall and you would be misled
[So this, above, is No. 3 – Focal Process (Requires Direct Vision Biopsy under Hysteroscopy)]
[Above] This woman has an advanced tumor along the front wall but nothing along the back wall.
[So this, above, is also No. 3 – Focal Process (Requires Direct Vision Biopsy under Hysteroscopy)]
If the transvaginal ultrasound scan is nondiagnostic, then the next step is hysterosonography with endometrial sampling YouTube video [See Reference (2) for instructions on how to perform the procedure].
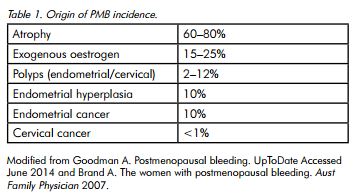
Causes of Postmenopausal Bleeding [Reference (3)]:
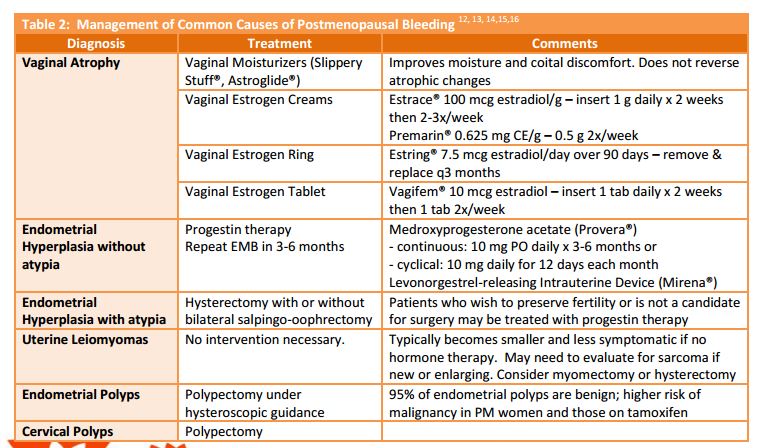
Treatment of Postmenopausal Bleeding [Reference (4)]:
Ultrasound For Postmenopausal Bleeding:
Resources:
(1) Ultrasound First and Postmenopausal Bleeding – Steven Goldstein, MD
(2) AIUM Webinar: Sonohysterography & Sonosalpingography
(3) Postmenopausal Bleeding [Full Text PDF]. Office Gynaecology, Vol 16 No 3 Spring 2014.
(4) An Overview of Postmenopausal Bleeding
By Marinelle Platon-Jones, DO, Gigi Kwok, MD, and Jennifer Keehbauch, MD