In addition to today’s resource please review
- “Cardiac Cases in Emergency Medicine” Redux From MetroHealth Emergency Ultrasound
Posted on March 24, 2024 by Tom Wade MD. The Cardiac Cases in Emergency Medicine post goes through 4 cardiac cases using the 5 Es to analyze each case.
Today I review and excerpt from the Introduction Section:
- The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652. Epub 2015 Apr 22.
All that follows is from the above resource.
Abstract
Emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) has been increasingly recognized as a crucial tool to help clinicians diagnose and treat potentially life-threatening conditions. The existing literature demonstrates a variety of EP FOCUS applications and protocols; however, EP FOCUS is not taught, practiced, or interpreted consistently between institutions. Drawing on over 12 years of experience in a large-volume, high-acuity academic emergency department, we have developed a protocol for teaching and performing EP FOCUS known as “The 5Es,” where each E represents a specific assessment for immediately relevant clinical information. These include pericardial effusion, qualitative left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava diameter and respirophasic variation). Each of these assessments has been well described in the emergency medicine literature and is within the scope of EP-performed echocardiography. This approach provides a reliable and easily recalled framework for assessing, teaching, and communicating EP FOCUS findings that are essential in caring for the patient in the emergency setting.
It has been recognized for more than 25 years that emergency physician (EP)-performed focused cardiac ultrasound (EP FOCUS) is an important skill for the care of patients with potentially life-threatening presentations.
We have found that the proximal thoracic aorta can be reliably assessed, providing vital information about potential aortic pathology in patients presenting with acute symptoms.7 We thus propose the “5Es” to assess for the presence of a pericardial effusion, left ventricular ejection, ventricular equality, exit (aortic root diameter), and entrance (inferior vena cava [IVC] diameter and respirophasic variation). The 5Es protocol provides an easy-to-teach, evidence-based, and standardized approach to EP FOCUS for the rapid identification and management of time-sensitive pathologic conditions.
Approach to exam
Typically EP FOCUS uses one or more of three windows and five views: a parasternal long-axis (PSLA), a parasternal short-axis (PSSA), an apical four-chamber (A4C), a subcostal long-axis (SCLA), and a subcostal four-chamber (SC4C) view. While pertinent findings are optimally confirmed in at least two views, it is understood that time constraints, patient acuity, patient mobility, and patient habitus may limit views.6, 8 For images in this article, we will use an emergency medicine convention for cardiac imaging with the probe marker oriented to the patient’s right, which keeps the anatomic right on the screen-left, as is the convention for other US imaging.9 This is in contrast with image and probe orientation utilized in traditional cardiology-performed US, but has been recognized as an accepted convention that we find to be conceptually easier, particularly when performing EP FOCUS as part of an integrated examination such as the focused assessment with sonography for trauma (FAST) or the rapid US for shock and hypotension.3, 6
Conclusions
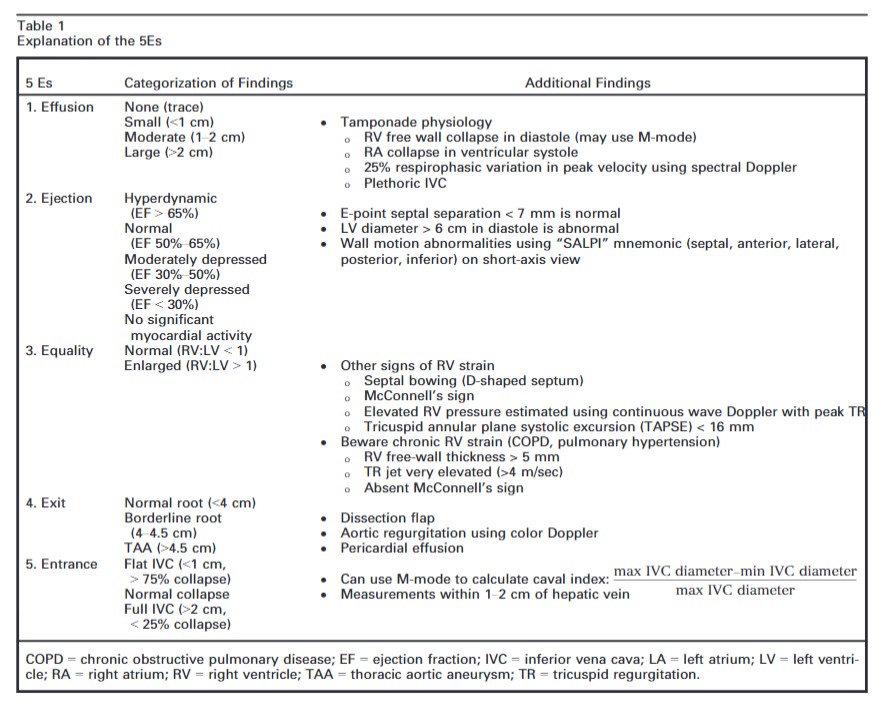
The intent of this article is to codify elements of the cardiac US exam that we have found to be most relevant to patients presenting with acute or emergent complaints (Table 1). A recent international consensus statement defined FOCUS as being goal-directed, problem-oriented, limited in scope, simplified, time-sensitive and repeatable, qualitative and semiquantitative, performed at the point of care, and usually performed by clinicians.6 The 5Es described in this article meet all of these criteria. However, the international statement addressed the use of FOCUS in “all clinical settings” and included the assessment of chronic cardiac disease, as well as gross valvular abnormalities and large intracardiac masses, without assessment of the thoracic aorta.
In our experience the 5Es encompass the cardiac US findings most applicable in patients who present emergently with hypotension, dyspnea, syncope, penetrating thoracic trauma, chest pain, or other acute complaints where diagnosis may be aided by visualization of the heart. While gross valvular abnormalities and intracardiac masses are important if they are seen, they are less common and less acute and tend to be less immediately deadly than acute thoracic aortic disease, which accounts for more than twice as many deaths as abdominal aortic aneurysm rupture.51The 5Es are not meant to provide an absolute boundary for EP FOCUS, which will likely continue to evolve, but are intended to provide a framework for the acquisition and interpretation of the most relevant and applicable components of echocardiography in the emergent setting. We hope that adoption and subsequent application of the 5Es in EDs will help to standardize and effectively teach the echo findings that may allow EPs to save lives and expedite the care of patients with potentially life-threatening illness. We thank Jane Hall, PhD, for preparing Figures 4, 6, and 8. We also thank Daniel Wadsworth Groves, MD, for manuscript review.