This post is just my study notes (my peripheral brain) on the treatment of syncope. I find that creating these posts really helps me fix the subject in my mind and helps me when I want to do a rapid review.
Primary care physicians in many practice settings (office, urgent care, and emergency department) may all be called upon to treat syncope. Just as TIA can be a warning of an increased risk of stroke, so can syncope be a warning sign of an increased risk of sudden death.
Thus, careful treatment of syncope is critical to prevention of the tragedy of sudden death no matter what your practice setting is.
Resources (1) through (4) provide the best framework for the treatment of syncope that I have seen.
What follows are extracts from Resource (1) 2018 ESC Guidelines for the diagnosis and management of syncope:
5. Treatment
5.1 General principles of treatment of syncope
The general framework of treatment is based on risk stratification and the identification of specific mechanisms when possible (Figure 8). The following three general principles should be considered:
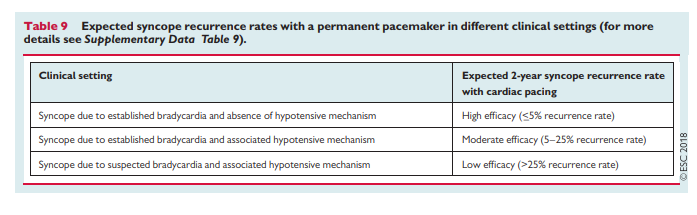
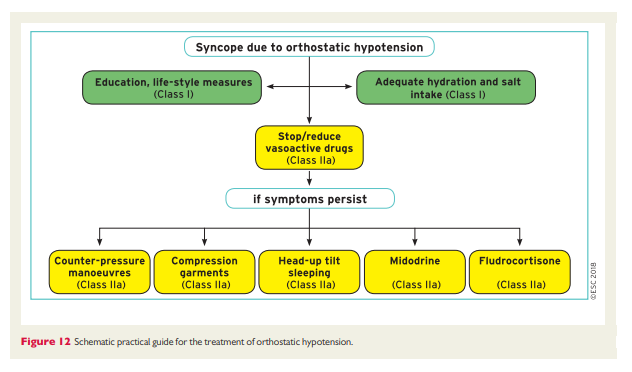
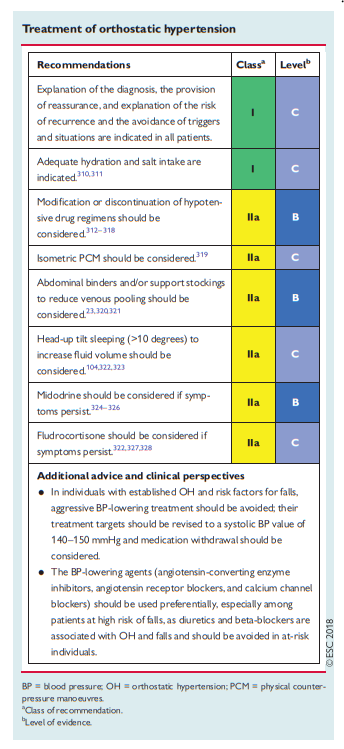
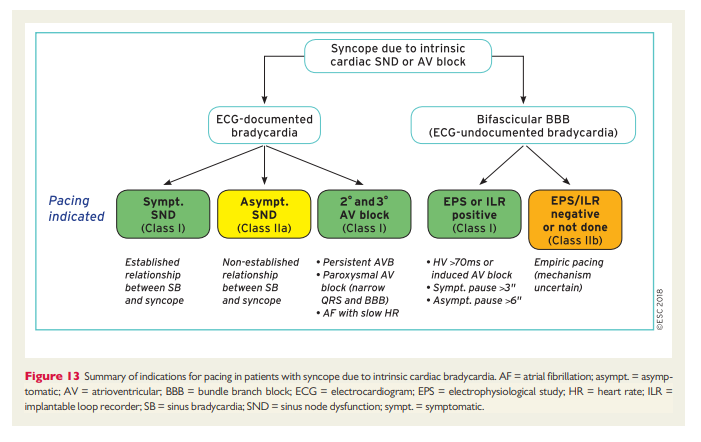
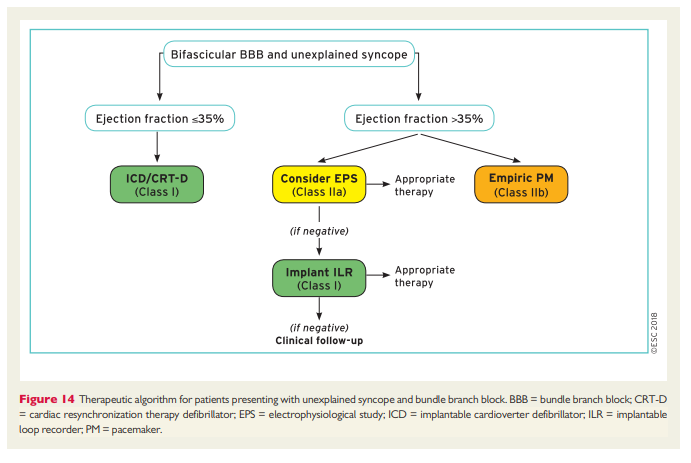
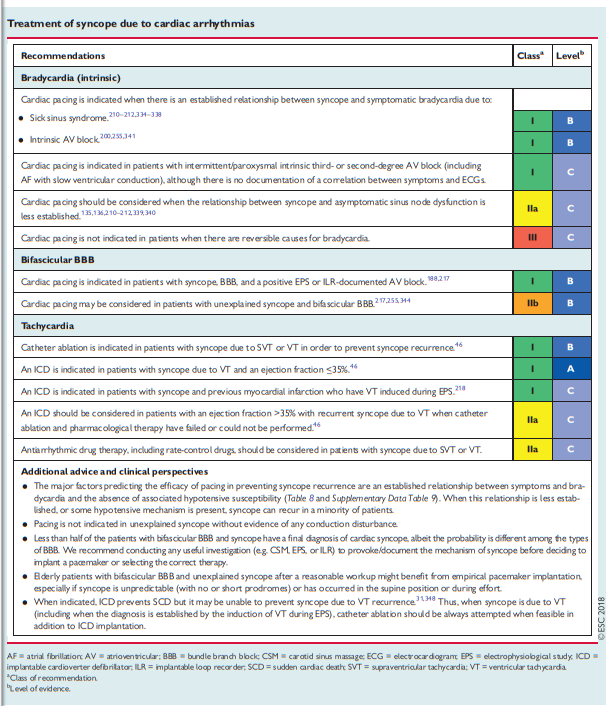
• The efficacy of therapy aimed at preventing syncope recurrence is largely determined by the mechanism of syncope rather than its aetiology. Bradycardia is a frequent mechanism of syncope. Cardiac pacing is the most powerful therapy for bradycardia but its efficacy is less if hypotension coexists (see Table 9 andSupplementary Data Table 9). The treatment of syncope due to a hypotensive reflex or to OH is more challenging because specific therapies are less effective.
• Often, therapy to prevent recurrence differs from that for the
underlying disease. The management of patients at high risk of
SCD requires careful assessment of the individual patient’s risk
(see section 5.5).• Syncopal recurrences often decrease spontaneously after medical assessment, even in the absence of a specific therapy; in general, syncope recurs in <50% of patients within 1–2 years (see Supplementary Data Table 10). The decrease seems to be more evident when there is a lack of a clear anatomical substrate for syncope, such as in the case of reflex syncope and unexplained syncope. The reason for this decrease is not known. Several potential clinical, statistical, and psychological explanations have been provided and all probably play a role (see Supplementary Data Table 10). Whatever the reason, the possibility of spontaneous improvement has major practical importance for treatment that can be postponed in low-risk conditions. The consequence of the spontaneous decrease is that any therapy for syncope prevention appears to be more effective than it actually is, which makes the results of observational data on therapy questionable in the absence of a control group.
Continue with table on p 43.
Resources:
(1) 2018 ESC Guidelines for the diagnosis and management of syncope [PubMed Citation] [Full Text HTML] [Access the Full Text PDF from the Full Text HTML link]. Eur Heart J. 2018 Mar 19. doi: 10.1093/eurheartj/ehy037. [Epub ahead of print]
(2) Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope [PubMed Citration] . Eur Heart J. 2018 Mar 19. doi: 10.1093/eurheartj/ehy071.
(3) Practical Instructions for the 2018 ESC Syncope Guidelines [a summary of the above article from the American College of Cardiology]. Apr 04, 2018 | Debabrata Mukherjee, MD, FACC.
(4) 2018 ESC Guidelines for the diagnosis and management of syncope – Supplementary Data [Full Text PDF]. European Heart Journal (2018) 00, 1–12 doi:10.1093/eurheartj/ehy037.
(5) The Evaluation Of Syncope In Primary Care – Help From The “2018 ESC Guidelines for the diagnosis and management of syncope” Posted on May 3, 2018 by Tom Wade MD.