All that follows is from Treatment of Sepsis and Septic Shock in Children from Emedicine/Medscape accessed 1/31/2015:
Recommendations and Regimens for Pediatric Sepsis and Septic Shock
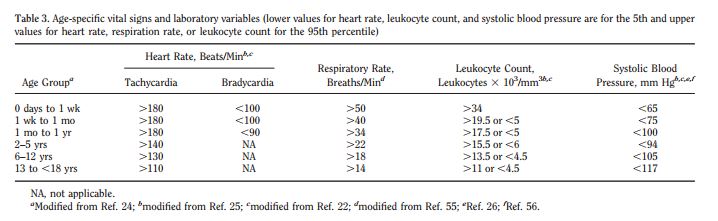
The definition of severe sepsis and septic shock in children is similar to that in adults. However, in pediatric patients, a systemic inflammatory response includes an abnormal temperature or abnormal leukocyte count as part of the clinical presentation. In addition, there are age-specific normative values for vital signs.[1]
Time-sensitive, goal-directed therapy is the rule. Consensus guidelines and reviews are available.[2, 3] Most guidelines are available online through the Pediatric Sepsis Initiative.[4] The Pediatric Advanced Life Support (PALS) Pocket Reference Card provides a summary algorithm.[5] International guidelines, despite weak evidence for many therapies, have recently been updated.[6]
Use of a triage protocol to recognize sepsis in children leads to more appropriate resuscitation management and shorter length of stay.[7] Additionally, clinician adherence to sepsis resuscitation guidelines also results in shorter length of stay for children.[8]
Recent reports question whether a fluid resuscitation – focused strategy is ideal in resource limited areas,[9] but resource-poor pediatric sepsis resuscitation data remain limited.[10]
Details of early recognition and treatment of sepsis and septic shock are provided below.
1. Recognize signs of poor perfusion (0-5min)
-
Decreased mental status
-
Cold extremities
-
Delayed capillary refill
-
Weak pulses, differential central and peripheral pulses
-
Low urine output
-
Hypotension or low BP: Minimum systolic BP by age: < 1mo: 60 mmHg; 1mo to 10y: 70 + (2 × age in years); ≥10y: 90 mmHg
2. Assess ABCs (0-5 min)
-
Provide 100% oxygen at high flow rate (15L)
-
Early intubation may be necessary in neonates and infants
-
Breathing assistance as necessary, including mechanical ventilation
3. Establish IV access and place on monitor (0-5min)
-
2 large-bore peripheral IVs (PIVs) preferred: if difficult IV, place IO access per PALS guidelines; 1 PIV may be sufficient unless vasoactive drugs needed (see Step No. 6, below)
-
Consider labs on IV placement: blood gas, lactate, glucose, ionized calcium, CBC, cultures (glucose check through finger stick preferred for rapid result)
4. Fluid and electrolyte resuscitation (5-15min)
Fluids:
-
Push 20 mL/kg fluid (isotonic crystalloid) IV/IO over 5-20min or faster if needed (reassess for signs of shock; see Step No. 11, below)
-
Repeat 20 mL/kg bolus push of fluid (up to 60 mL/kg) until clinical symptoms improve or patient develops respiratory distress/rales/ hepatomegaly
-
May continue to require additional fluid above 60 mL/kg (fluid refractory) (see Step No. 6, below)
-
Fluid needs may approach 200 mL/kg in warm septic shock (warm extremities, flash capillary refill)
Correct hypoglycemia:
-
Glucose levels in hypoglycemia: Neonates < 45 mg/dL; infants/children < 60 mg/dL
-
Glucose dosage: 0.5-1 g/kg IV/IO (max that can be administered through a peripheral vein is 25% dextrose in water) (see alternative treatments immediately below)
-
Treatment options to provide 0.5-1 g/kg glucose: For infant/child: dextrose 25% in water: 2-4 mL/kg IV/IO; dextrose 10% in water: 5-10 mL/kg IV/IO; for neonate: dextrose 10% in water: 2-4 mL IV/IO; consider maintenance fluid containing dextrose
Correct hypocalcemia for low ionized calcium:
-
Calcium gluconate 100 mg/kg IV/IO (max 2g) PRN
-
Calcium chloride 20 mg/kg IV/IO PRN (Note: central line administration preferred over 60min in nonarrest situation)
5. Infection control (5-60min)
Immediate considerations:
-
Administer antibiotics immediately after cultures obtained (blood, urine, +/- CSF/ sputum)
-
Do not delay antibiotics because of delay in obtaining cultures; initial antibiotics should be given within 1h
General treatment recommendations:
-
Empiric therapy should be used for unknown etiology of sepsis;
-
Tailoring of therapy to address suspected pathogens or to achieve adequate drug penetration may be necessary;
-
Broader initial coverage may be needed for initial stabilization
-
Dosing varies by age and weight (see specific recommendations and dosages immediately below)
Neonates < 2kg:
-
Consult institution pharmacist and primary medication references for your institution practice and for preterm infants and neonates < 2kg
Neonates >2kg:
-
Ampicillin plus gentamicin: Ampicillin for 0-7d: 50 mg/kg IV/IM/IO q8h; ampicillin >7d: 50 mg/kg IV/IM/IO q6h plus gentamicin (dosing institution dependent): 4mg/kg IV/IO/IM q24h (alternative for 0-7d: 2.5 mg/kg IV/IO/IM q12h; alternative for >7d: 2.5 mg/kg IV/IO/IM q8h) or
-
Ampicillin plus cefotaxime: Ampicillin for 0-7d: 50 mg/kg IV/IM/IO q8h; ampicillin >7d: 50 mg/kg IV/IM/IO q6h plus cefotaxime 50 mg/kg IV/IO q8h
Infants (>1mo) and children:
-
Ceftriaxone 75 mg/kg (max 2g) IV/IO/IM q24h plus vancomycin 15mg/kg (max 1g) IV/IO q8h
Immunosuppressed patients:
-
Vancomycin 15 mg/kg IV/IO (max 1 g/dose) q8h plus cefepime 50 mg/kg IV/IO (max 2g/dose) q8h; consider antifungal therapy
Duration of therapy:
-
Determined by ultimate source of infection; 7-10d is typically sufficient
-
Above regimens may be empiric therapy for 48-72h, until cultures and sensitivities are known, so as to accurately tailor treatment
-
If culture-negative sepsis, antibiotic choice and duration determined by severity of presentation and most likely pathogen
-
Infectious disease consultation may be necessary
6. Fluid-refractory shock (persisting after 60 mL/kg fluid) (15-60 min)
-
Continue fluid resuscitation and initiate vasopressor therapy titrated to correct hypotension/poor perfusion
-
Central line placement and arterial monitoring if not already established; vasopressors should not be delayed for line placements
-
Normotensive shock (impaired perfusion but normal blood pressure): Dopamine 2-20 mcg/kg/min IV/IO, titrate to desired effect; if continued poor perfusion, consider dobutamine infusion 2-20 mcg/kg/min IV/IO, titrate to desired effect (may cause hypotension, tachycardia)
-
Warm shock (warm extremities, flash capillary refill): Norepinephrine 0.1-2 mcg/kg/min IV/IO infusion, titrate to desired effect
-
Cold shock (cool extremities, delayed capillary refill): Epinephrine 0.1-1 mcg/kg/min IV/IO infusion, titrate to desired effect
7. Shock persists following vasopressor initiation (60 min)
-
Continued fluid replacement; obtain CVP measurement to guide
-
SvO2 < 70% (cold shock): Transfuse Hgb >10 g/dL; optimize arterial saturation through oxygen therapy, ventilation; epinephrine 0.1-1 mcg/kg/min IV/IO infusion, titrate to desired effect
-
SvO2 < 70% (normal BP but impaired perfusion): Transfuse Hgb >10 g/dL; optimize arterial saturation through oxygen therapy, ventilation; consider addition of milrinone 0.25-0.75 mcg/kg/min IV/IO (titrate to desired effect) ornitroprusside 0.3-5 mcg/kg/min IV/IO (titrate to desired effect)
-
SvO2 >70% (warm shock): Norepinephrine 0.1-2 mcg/kg/min IV/IO infusion, titrate to desired effect; consider vasopressin 0.2-2 mU/kg/min infusion, titrate to desired effect
8. Fluid refractory and vasopressor-dependent shock) (60 min)
-
Consider adrenal insufficiency
-
Hydrocortisone 2 mg/kg (max 100mg) IV/IO bolus; obtain baseline cortisol level; if unsure, consider ACTH stimulation test; duration depends on response, laboratory evaluation
9. Continued shock
-
Consider cardiac output measurement to direct further therapy
-
Consider extracorporeal membrane oxygenation (ECMO)
10. Supplemental therapies
-
Blood transfusion considered for Hgb < 10 g/dL (ideal threshold for transfusion unknown)
-
Sedation/analgesia while ventilated
-
Optimize oxygenation through ventilation
-
IV immunoglobulin can be considered (unknown benefit; see Step No. 6 Infection Control for dosing information)
11. Therapeutic endpoints
Clinical
-
Heart Rate normalized for age
-
Capillary refill < 2sec
-
Normal pulse quality
-
No difference in central and peripheral pulses
-
Warm extremities
-
Blood pressure normal for age
-
Urine output >1 mL/kg/h
-
Normal mental status
-
CVP >8 mmHg
Laboratory
-
Decreasing lactate
-
SvO2 >70%
Resources from the Emedicine/Medscape article above:
- Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. Jan 2005;6(1):2-8. [Medline].
- [Guideline] Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. Jan 2008;36(1):296-327. [Medline].
- Carcillo JA, Fields AI. Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med. Jun 2002;30(6):1365-78. [Medline].
- World Federation of Pediatric Intensive and Critical Care Societies. Pediatric Sepsis Initiative educational materials. Available at https://www.wfpiccs.org/education/doctors-nurses/documents/. Accessed June 23, 2013.
- American Heart Association. EC90-1053. Distributed by Channing Bete Co. Pediatric Advanced Life Support Pocket Reference Card. Available at https://shop.aha.channing-bete.com/onlinestore/storeitem.html?iid=180286. Accessed Nov 9, 2011.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. Feb 2013;41(2):580-637. [Medline].
- Larsen GY, Mecham N, Greenberg R. An emergency department septic shock protocol and care guideline for children initiated at triage. Pediatrics. Jun 2011;127(6):e1585-92. [Medline].
- Paul R, Neuman MI, Monuteaux MC, Melendez E. Adherence to PALS Sepsis Guidelines and Hospital Length of Stay. Pediatrics. Aug 2012;130(2):e273-80. [Medline].
- Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. Jun 30 2011;364(26):2483-95. [Medline].
- Murthy S, Kissoon N. After the FEAST–fluid resuscitation in pediatric sepsis. Indian J Pediatr. Feb 2013;80(2):151-4. [Medline].