For an excellent YouTube video on elective cardioversion of atrial fibrillation please see my link to Cardioversion Of Atrial Fibrillation – Dr. Mellick’s Great YouTube Video Posted on October 6, 2017 by Tom Wade MD.
Today’s study assignment for myself is to review some resources on unstable atrial fibrillation – Dr. Morganstern’s post and Dr. Weingart’s podcast and show notes.
I’ve linked to Dr. Morganstern’s post, Management of unstable atrial fibrillation in the emergency department: An approach to the initial management of the severely hypotensive atrial fibrillation patients, in a past post.
But I wanted to remind myself tofirst review Dr. Morganstern’s complete post again [Note to myself – do that now].
Case
You are finishing up your charts and getting ready to head home for the night, having already handed over to the night doc who is currently wrapped up with a moderately unwell trauma patient. The charge nurse asks you to just look at one patient who she thinks has SVT before you head home. You walk into the room and see a grey, diaphoretic man, who you later find out is 67 years old. The chart in your hand says that he has a history of hypertension and hyperlipidemia, but is otherwise healthy. The monitor reveals a heart rate of approximately 205, but it jumps around a lot from beat to beat, and a blood pressure of 86/43. He is satting 100%, but is on a nonrebreather. The ECG is narrow complex and irregularly irregular. His wife tells you this all started about 1 hour ago with complaints of dizziness and palpitations but no chest pain….
First question: Is the atrial fibrillation the cause of the problem, or just a symptom?
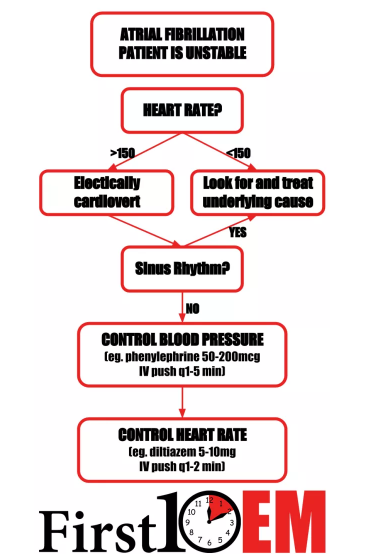
If the patient’s hypotension and tachycardia are due to sepsis or hemorrhage, controlling the rapid heart rate is not going to help. In fact, the rapid heart rate is probably necessary to maintain an adequate cardiac output. In these situations, the goal should be treating the underlying cause. However, it can be very difficult to determine whether rapid atrial fibrillation is the cause of, or the result of hypotension. The rule of thumb I have used is that if the rate is less than 150, hypotension is unlikely to be the result of atrial fibrillation, whereas if the rate is greater than 150, the arrhythmia is probably at least a component of the patient’s shock.
Cardiovert
According to the ACLS guidelines, management is very straight-forward. The patient is unstable, so electrically cardiovert him. Unfortunately, cardioversion never seems to work in these really sick patients. However, I will always give cardioversion a shot first. [And don’t forget sedation – Dr. Morganstern recommends etomidate. And don’t forget that you’ll need to have a pressor ready as all sedatives can drop the pressure.]
Unfortunately, cardioversion rarely works in truly unstable atrial fibrillation. At this point, the key question is: Is this WPW (Wolff-Parkinson-White syndrome)?
The main feature I watch for is bizarre appearing QRS complexes that change in width from beat to beat. Also, atrial fibrillation with a rate greater than 220-250 is not compatible with AV node conduction, but rather an accessory pathway.
If WPW, do not start any medications that could slow conduction through the AV node (amiodarone, beta-blockers, calcium channel blockers). This could paradoxically increase the rate of conduction through the accessory pathway, leading to ventricular rates of >300, which is also known as ventricular fibrillation. In the setting of WPW, electrical cardioversion is your best choice – and luckily, this is a subset a patients for whom electricity is likely to work. The only other safe option is probably procainamide (17mg/kg slow IV bolus).
For all other patients, the next step is to manage the hypotension:
Definitive therapy of hypotension requires correction of the arrhythmia. However, the patient is in shock and the rate control agents we need to use will worsen hypotension.
Management of hypotension almost always start with some fluids. With rapid atrial fibrillation resulting in cardiogenic shock, you have to be very careful of causing pulmonary edema. Also, there little reason to believe that this patient is significantly fluid depleted. However, the rate control agents are all vasodilatory, and therefore some fluid resuscitation may be helpful. I generally hang a small (500ml) normal saline bolus and reassess frequently.
The primary temporizing treatment of this patient’s hypotension will be a vasopressor. In general, I prefer controlled drips of pressors when I have the option. In this scenario, I want vasoconstriction with limited impact on heart rate (chronotropy). My go to agent would be norepinephrine, started at 5mcg/min and titrated to a diastolic blood pressure of 60.
However, we all know that starting drips in emergent situations can take much too long. In practice, my go to vasopressor is often going to be push dose phenylephrine:
Draw up 1ml of phenylephrine (10mg/ml) into a syringe
Inject the entire 1ml (or 10mg) into a 100ml bag of normal saline
You now have 10mg in a total of 100ml, or 100mcg/ml
Inject 0.5-2ml (50-200mcg) every 1-5minutes, as needed
Goal of diastolic blood pressure of ≥ 60
Don’t just read about it, watch Dr. Scott (Hollywood) Weingart show you how to mix push dose phenylephrine:Mixing Epinephrine for Push-Dose Pressors from Scott from EMCrit on Vimeo.
Once the blood pressure is temporized, it’s time to start the real treatment of this patient’s shock: getting control of the heart rate. The two options I would consider are diltiazem and amiodarone. (Some people would consider beta-blockers here, but I think there is ample evidence that calcium channel blockers are more effective at rapidly achieving rate control, which is exactly what I want here.) I actually don’t think there is much of a difference between amiodarone and diltiazem, but the cardiologists I work with always seem to prefer amiodarone. Personally, I think diltiazem does a better job of rapidly achieving rate control.
Diltiazem
I give this is one of two ways:
Diltiazem 25 mg in a minibag and slowly dripped in over about 10-15 minutes
Diltiazem 5-10mg (small doses) pushed by me every 1-2 minutes
After an appropriate heart rate is reached (for these very sick patients I am generally happy to get them to less than 130), I switch to either the conventional diltiazem drip at 5-15mg/hr or 30-60mg of PO diltiazem
There may be some value to giving IV calcium (1 or 2 grams of calcium gluconate) before starting the diltiazem to reduce the hypotensive effects of the medication
The atrial fibrillation still isn’t controlled – what now?The good news is that unlike electrical cardioversion, rate control with diltiazem is almost always effective. If the patient remains unstable and you have not been able to control the heart rate, it is time to rapidly involve the expertise of a cardiologist. While waiting for them to arrive, I would consider adding magnesium or digoxin.
Magnesium
2-4 grams IV over 10-15 minutes
Has been shown to modestly decrease heart rate and also possible increase the rate of spontaneous reversion to sinus rhythmDigoxin
500mcg IV over 20 minutes
Generally takes to long to be really useful in an unstable patientThe most common alternate management strategy I have encountered focuses on just using fluid boluses to support the pressure while loading amiodarone. There is no evidence that vasopressors help patients, so I can’t argue, but I have a hard time not temporarily making the numbers better while I wait for rate control to occur. Maybe I am treating my own anxiety more than the patient.
[But all the other experts also recommend defending the MAP with a pressor while we deal with whatever is causing the hypotension.]
So I’ve reviewed his excellent post and now I’ll go over the other FOAMed resources he recommends in his blog post:
EMCrit Podcast 20 – The Crashing Atrial Fibrillation Patient
The podcast is only 9:00 minutes long. Also his show notes are a great review and quickly cover and reinforce Dr. Morganstern’s post.
For your cardioversion, Dr. Weingart recommends:
You need to give your patient something to disguise the fact that you are electrocuting them. Yet you don’t want to drop their pressure. Ketamine is ok in disassociative dosing, but then your patient is loopy and you lose your mental status exam. Consider 5-7 mg of etomidate along with a pain dose of ketamine, 10-15 mg.
Screen for WPW
If you have a. fib with a wide QRS and a rate > 250-300, be scared, very scared. This is WPW and these patients just love to ruin your day by going into v. fib. Shock early, shock often, light them up.Get the BP Up
So you made sure it’s not WPW and the cardioversion has failed, as it so often does in chronic a. fib. Now you need to raise the BP before anything else. Use push-dose phenylephrine. 50-200 mcg every minute or so until you get the blood pressure above a diastolic of 60; this will temporize the situation and make the patient’s heart more likely to slow down.Though things look better, you have not really fixed the problem, you have just temporized.
Slow them them down
Give either amiodarone 150 mg bolus and then the drip (may repeat the bolus x 1)
Or
Use diltiazem, but not as a push. Drip it in at 2.5 mg/minute until HR < 100 or you get to 50 mg. (Resuscitation 52:167, 2002) See here for more.
Update:
This study would indicate that perhaps we are doing more harm than good when we aggressively try to control rate or rhythm in stable (non-crashing) patients (Ann Emerg Med 2015;65(5):511)
Calcium before Diltiazem may reduce hypotension in rapid atrial dysrhythmias and Atrial Fibrillation Rate Control in the ED: Calcium Channel Blockers or Beta Blockers? on ALiEM
Magnesium infusions for atrial fibrillation and torsade on PulmCrit/EMCrit
A-Fib Unleashed! and Atrial flutter, fibrillation and ablation on ERCast
Episode 20: Atrial Fibrillation, Best Case Ever 7: Atrial Fibrillation, and Episode 57: The Stiell Sessions 2 – Update in Atrial Fibrillation 2014 on Emergency Medicine Cases
Fast atrial fibrillation on EM Tutorials
SGEM#133: Just Beat It (Atrial Fibrillation) with Diltiazem or Metoprolol? and SGEM#88: Shock Through the Heart (Ottawa Aggressive Atrial Fibrillation Protocol) on The Skeptics Guide to EM