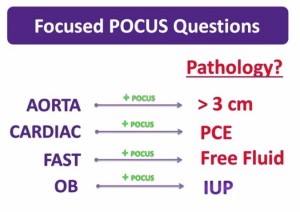
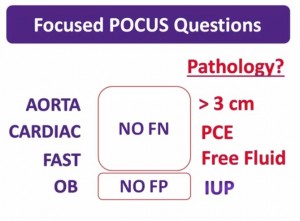
POCUS means Point of Care Ultrasound.
Be sure to click Additional Resources for an outstanding online free Ob-Gyn Ultrasound Text.
Basic Applications : Female Pelvis – Positive OB Study. [This link is to YouTube Site] Jun 30, 2013 by Westernsono, 20:24.
What follows are the slides from this video (for quick review):
Goal of this vid is to define a positive study.
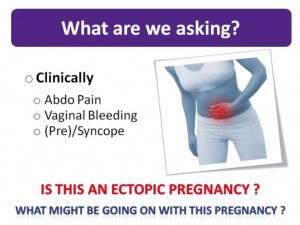
What patients do we need to ask the question: Is this an ectopic pregnancy?
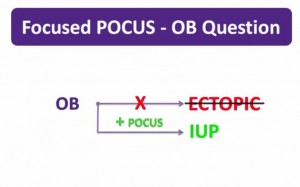
The OB question in focused POCUS is not–Is this an ectopic pregnancy? as they can be very hard to diagnose when present even for the best sonographers.
And ectopic pregnancy can develop complications before we can diagnose the ectopic on US.
So the hunt for ectopic is not a realistic goal for bedside ultrasound.
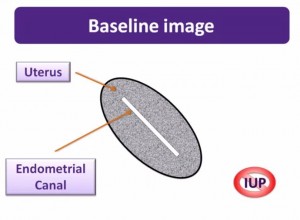
The good news is that a normal IUP is something that usually can be seen with a bedside ultrasound “with the obvious caveat that gestational age matters.
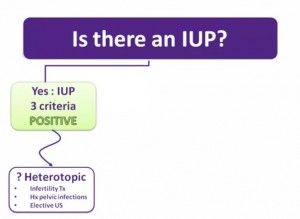
In most cases once you have confidently diagnosed an IUP, the diagnosis of ectopic pregnancy is effectively excluded as the cause for their presenting symptoms.
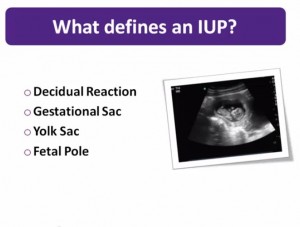
Therefore a positive bedside ob study is achieved when an IUP is diagnosed [with
certain exceptions].
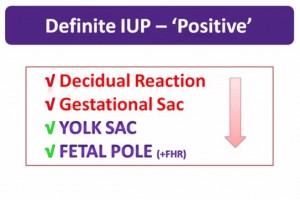
The bedside OB study has tremendous consequence if you err. Therefore you
must not diagnose IUP unless all the criteria are met.
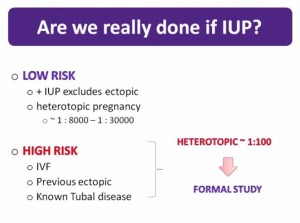
A heterotopic pregnancy is an intrauterine pregnancy and an ectopic pregnancy. In pts at low risk of ectopic pregnancy a + IUP excludes a heterotopic pregnancy as in these patients the incidenc of ectopic in pt with an IUP is said to be about 1:8000 to 1:10,000.However, there are patients at much higher risk. These High Risk Patients include: -pts undergoing invitro fertilation -pts with a previous hx of ectopic pregnancy -pts with known tubal disease
The risk in the above patients may be as hig h as one in one hundred.
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
Next
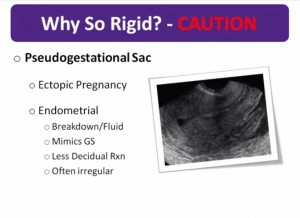
The slide below gives one the reason we must be incredibly careful about not over calling an intrauterine pregnancy–Pseudogestational Sac.
“The pseudogestational sac is present in 5 to 10% of ectopic pregnancies and may mimic a gestational sac.”
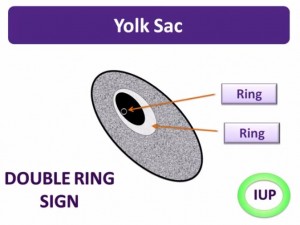
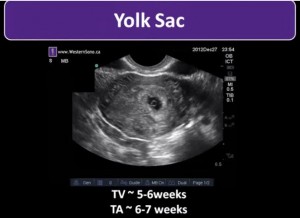
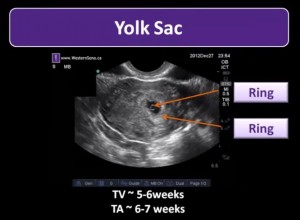
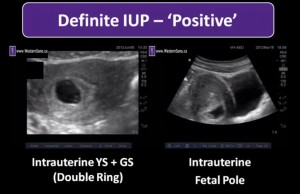
“Be careful! Without a clear cheerio of the yolk sac or a discreet fetal pole with structure, then one must not make the call of intrauterine pregnancy.”
[And we need to be sure that any pregnancy we do see is intrauterine–don’t get tricked into assuming a pregnancy is intrauterine.]
See 15:25 to 16:25.
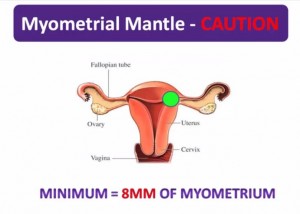
“One final area of risk exists when confirming IUPs. Rarely, a pregnancy can implant itself in the horn of the uterus–an area where there is little thickness to the myometrium. Imagine a pregnancy developing here [in the green area in the slide below]. As it grows there is a high risk of rupture of the thin myometrial mantle surrounding it posing significant hemorrhagic risk to the mother.”
“So how do you protect [the patient] against this risky scenario?”
“One must always be sure to measure the amount of myometrium surrounding the pregnancy and accept no less than 8 mm at any one point.”
“If you do find an equivocal or concerning area, be sure to have that patient properly imaged and referred as these are high risk pregnancies.
16:25 to 17:09
“Here is a scan showing us the cardinal findings of intrauterine pregnancy–but remember to find the bladder first to be sure that this is the uterus. However, there is some concern about the myometrial mantle surrounding it. This patient should be evaluated formally.
Next
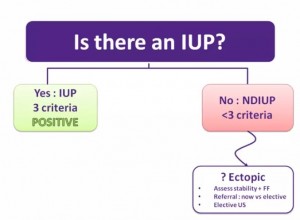
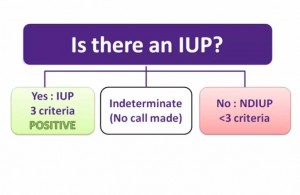
“So let’s review our overall approach to the first trimester scan.”
“We know we are not going to ask: Is there an ectopic pregnancy?”
“Rather, we are going to ask: Is there confirmatory evidence of an IUP?”
“If we can clearly see the entire uterus, but not meet the criteria to be certain that there is an IUP, then we interpret our scan as NDIUP. In this case, the broader clinical picture must be considered and the potential risk of ectopic must weigh into the decision making.”
And clinical suspicion and clinical judgement must reign supreme.
“It may very well be that our generated images are not adequate enough to make a call. This usually occurs when scanning a patient with an empty bladder and the scatter artifact from bowel does not allow the full assessment of the uterus.”
“To make a determinant call as either an IUP or a NIUP, you must first be sure that you can see the entire uterus.”
“Not infrequently you will ask that patient to fill her bladder and repeat the scan.”
Ultrasound in Obstetrics and Gynecology: A Practical Approach. 2014. A Abuhamad MD. [Free Full Text PDF available online] [Link to Free Download]