As an Indiana physician, I reviewed the outstanding Indiana Department of Health‘s resource, Tick-Borne Diseases. The resources and links on this page merit very careful review.
Today, I review, link to, and excerpt from The Cribsiders‘ #103: Tick-Talk: A Deet-ailed Look at Tick-Borne Illnesses*.
*Hanson RM and Ward B, Creech CB, Masur S, Chiu C, Berk J. “#103: Tick Talk: A Deet-ailed look at Tickborne Illnesses”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ February 14, 2024.
All that follows is from the above resource.
Summary:
Dr. Buddy Creech of Vanderbilt teaches us the core signs and symptoms of tick-borne illnesses, the importance of geographic variation in making a diagnosis, why doxycycline is the drug of choice for treatment, and not just what but also why we see lab abnormalities in Ehrlichiosis.
Tick-Borne Illnesses Pearls
- Fever, photophobia, headache, arthralgias, and rash without respiratory symptoms or sick contacts are classic symptoms that can be found in tick borne illnesses.
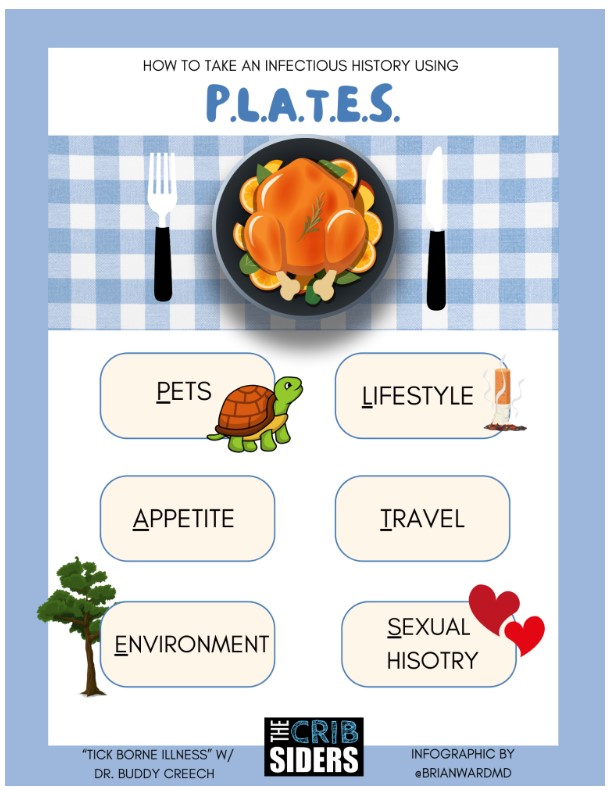
- Use the mnemonic ‘PLATES’ to take an ID history: Pets, Lifestyle, Appetite, Travel, Exposures, Sexual history.
- Lab findings such as lymphopenia, thrombocytopenia, and hyponatremia are common in tick-borne illnesses.
- Lab confirmation of tick-borne illnesses is not necessary for treatment. A clinical diagnosis can and should be made to provide effective and timely treatment.
- Doxycycline is the drug of choice for treatment of tick-borne illnesses and is safe for use in pediatric patients.
- Consider geographic distributions of tick-borne illnesses to narrow your differential. Lyme = NE, upper Midwest, and Atlantic seaboard. Rickettsial diseases = SE, Midwest, and Rocky Mountains*
- Prevention of tick-borne illnesses is primarily through prevention of tick bites. This includes DEET, permethrin, and picaridin
*For information on tick-borne diseases in your area, be sure to check with your state department of health’s website.
Tick-Borne Illnesses Notes
Taking a Tick History
How to take an ID history using PLATES:
Pets: Dogs, cats, and everything else that your patient loves
Lifestyle: Inside/Outside, x-box or woodland adventures
Appetite: Dirt, Pica, unpasteurized or exotic foods
Travel: domestic and abroad
Exposure: known exposures to communicable diseases
Sexual history: when applicable, but it’s applicable more than you’re asking
Geographic distribution dictates the likelihood of tick borne disease. This is specifically due to the regional nature of the infectious vectors. The CDC has great maps * to show what is prevalent in your area.
*Tickborne Diseases of the United States
Oftentimes, ticks exposures are not actually known. As Dr. Creech noted, there’s always a tick even if the patient doesn’t remember removing one themselves. Similarly, it is estimated that many minor diseases (in the right areas) may be a presentation of tick-borne diseases. In Dr. Creech’s expert opinion, it is OK to empirically treat in the summer in the right clinical setting.
(Note, Dr. Creech stated there’s also always a cat, but Bartonella is out of the scope of this episode)
Laboratory Findings Suggestive of Tick Borne Diseases:
In General, look for lymphopenia, thrombocytopenia, hyponatremia, elevated liver enzymes.
Rickettsial diseases (Ehrlichia and Rickettsia) cause vasculitis which can lead to SIADH and DIC, causing the findings of hyponatremia and thrombocytopenia. Ehrlichia classically presents with elevated liver enzymes.
Treatment (Doxycycline. That’s it. That’s the Tweet.)
Doxycycline is the mainstay of treatment for all tick borne diseases.
Because we do not have a timely and effective serologic diagnosis, diagnosing tick borne illness is a clinical diagnosis. Moreover, the mortality for Ehrlichia and Rickettsia increases after 4 days without treatment. Empiric coverage may be given to patients with sepsis if time of year and location fits.
The treatment course is quite simply “treat until a couple days beyond symptom improvement” for Rickettsial illnesses. Lyme disease treatment is typically 2 weeks.
Lyme Disease Follows Its Own Path:
Unlike other tick borne illnesses which either get better or get significantly worse, Lyme disease, caused by the spirochete Borrelia burgdorferi, acts strangely and has multiple phases. Because it is challenging to test for, we deal with it separately here.
Lyme phases:
- Early Localized: erythema migrans
- Early Disseminated: flu-like illness
- Mid/late: Carditis, facial palsy, culture negative lymphocytic meningitis
- Late finding: Septic arthritis
Similar to other tick borne diseases, doxycycline is always the drug of choice for Lyme, with the exception of pregnancy and CNS disease, for which ceftriaxone is used. Duration is related to the response to treatment.
Lyme confirmatory testing: two-tiered approach with ELISA first, then confirmed with Western Blot. The first test is sensitive, the second test is specific. Providers may only see positive or negative test results. Families may also see results before providers do. When sending these tests, Dr. Creech typically tells families that testing is complicated and will need expertise to interpret.
Lyme prophylaxis may be given in high endemic areas (Zhou et al., 2021) if these criteria are met:
- Endemic area
- Engorged Tick
- Black legged/Ixodes tick
- Doxycycline is otherwise clinically safe (not pregnant or breastfeeding)
Dose for prophylactic doxycycline is one “double-dose”:
- 200mg for adults
- 4.4mg/kg for children
Co-infections
Babesiosis is associated with Lyme disease, though is very rare. Consider babesiosis when the previously diagnosed disease (like Lyme) is not responding to typical therapies. Risk factors to babesiosis include asplenia, immunocompromised, chronic liver or kidney disease. Babesiosis treatment is similar to malarial disease.
One last coinfection is that of skin flora. A tick bite is a break in the skin, which can introduce skin flora to deeper tissues causing, for example, cellulitis.
Removal
Remove ticks with tweezers when found. Apply gentle pressure to remove the entirety of the tick. Try to avoid bursting the tick!
Prevention
Understand the geographic distribution of tick-borne illnesses to know when to implement prevention strategies– tick bites are more common in overgrown areas, less common in cities and fairways.
Chemical bug repellent is effective, especially deet. Treat clothes with permethrin. Other tick prevention chemicals/compounds include picaridin, lemon oil, and eucalyptus. And, as a fail-safe, perform tick checks. Look at the hairline, axilla, and skin folds. Assess your clothes for ticks and wash your clothes when done exploring.