In this post I link to and excerpt from the excellent 2017 Clinical Practice Guidelines for the management of Depression from the Indian Journal of Psychiatry. [No Abstract Available] [Full-Text HTML] [Full-Text PDF]. Indian J Psychiatry. 2017 Jan;59(Suppl 1): S34-S50.
All that follows is from The Guidelines:
Introduction
Depression is a common disorder, which often leads to
poor quality of life and impaired role functioning. It is
known to be a major contributor to the global burden
of diseases and according to World Health Organization
(WHO), depression is the fourth leading cause of disability
worldwide and it is projected that by 2020, it will be
the second most common leading cause of disability.
Depression is also associated with high rates of suicidal
behaviour and mortality. When depression occurs in the
context of medical morbidity, it is associated with increased
health care cost, longer duration of hospitalization, poor
cooperation in treatment, poor treatment compliance and
high rates of morbidity. Depression is also known to be
associated with difficulties in role transitions (e.g., low
education, high teen child-bearing, marital disruption,
unstable employment) and poor role functioning (e.g.,
low marital quality, low work performance, low earnings).
It is also reported to be a risk factor for the onset and
persistence of a wide range of secondary disorders.
Available data also suggests that between one-third
and one-half of patients also experience recurrence of
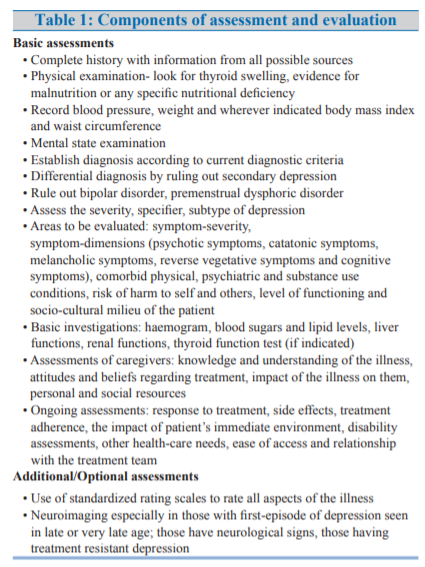
depressive episodes.ASSESSMENT AND EVALUATION (table-1)
FORMULATING A TREATMENT PLAN (FIGURE-1)
EVALUATE THE SAFETY OF PATIENT AND OTHERS
A careful assessment of the patient’s risk for suicide should
be done. During history inquiry for the presence of suicidal
ideation and other associated factors like presence of
psychotic symptoms, severe anxiety, panic attacks and
alcohol or substance abuse which increases the risk of suicide
need to be evaluated. It has been found that severity of
depressive symptomatology is a strong predictor of suicidal
ideation over time in elderly patients. Evaluation also includes
history of past suicide attempts including the nature of those
attempts. Patients also need to be asked about suicide in their
family history. During the mental status examinations besides
enquiring about the suicidal ideations, it is also important to
enquire about the degree to which the patient intends to act
on the suicidal ideation and the extent to which the patient has
made plans or begun to prepare for suicide. The availability
of means for suicide be inquired about and a judgment may
be made concerning the lethality of those means. Patients
who are found to possess suicidal or homicidal ideation,
intention or plans require close monitoring. Measures such as
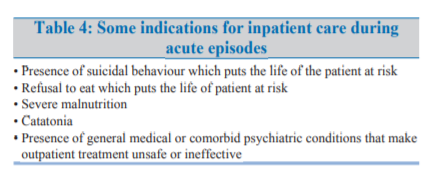
hospitalization may be considered for those at significant risk.CHOICE OF TREATMENT SETTINGS
Majority of the cases of depression seen in the clinical
setting are of mild to moderate severity and can be managed at the outpatient setting. However, some patients have
severe depression which may be further associated with
psychotic symptoms, catatonic symptoms, poor physical
health status, suicidal or homicidal behaviour etc. In such
cases, careful evaluation is to be done to decide about the
treatment setting and whenever necessary inpatient care
may be offered. In general, the rule of thumb is that the
patients may be treated in the setting that is most safe and
effective. Severely ill patients who lack adequate social
support outside of a hospital setting may be considered
for admission to a hospital whenever feasible. The optimal
treatment setting and the patient’s ability to benefit
from a different level of care may be re-evaluated on an
ongoing basis throughout the course of treatment. Some
of the common indications for inpatient care are shown
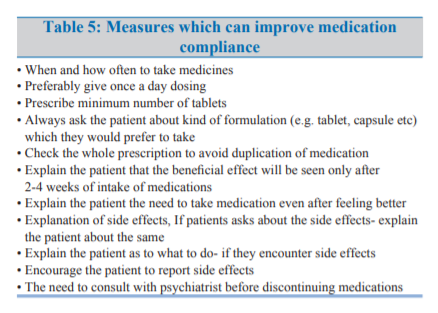
in Table-4.ENHANCED TREATMENT COMPLIANCE
The successful treatment of major depressive disorder
requires adequate compliance to treatment plan. Patients
with depressive disorder may be poorly motivated and
unduly pessimistic over their chances of recovery with
treatment. In addition, the side effect or requirements of
treatment may lead to non-adherence. Patients are to be
encouraged to articulate any concern regarding adherence
and clinicians need to emphasize the importance of
adherence for successful treatment. Simple measures
which can help in improving the compliance are given in
table-5.ADDRESS EARLY SIGNS OF RELAPSE
Many patients with depression experience relapse.
Accordingly, patients as well as their families if appropriate may be educated about the risk of relapse. They can be educated
to identify early signs and symptoms of new episodes. Patients
can also be asked to seek adequate treatment as early in the
course of a new episode as possible to decrease the likelihood
of a full-blown relapse or complication.TREATMENT OPTIONS FOR MANAGEMENT FOR DEPRESSION
Treatment options for management of depression can be
broadly be divided into antidepressants, electroconvulsive
therapy (ECT) and psychosocial interventions. Other less
commonly used treatment or treatments used in patients
with treatment resistant depression include repetitive
transcranial magnetic stimulation (rTMS), light therapy,
transcranial direct stimulation, vagal nerve stimulation,
deep brain stimulation and sleep deprivation treatment.
In many cases benzodiazepines are used as adjunctive
treatment, especially during the initial phase of treatment. Additionally in some cases, lithium and thyroid supplements
may be used as an augmenting agent when patient is not
responding to antidepressants.Antidepressants
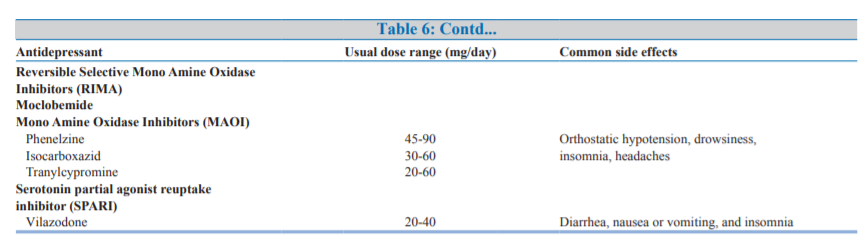
Large numbers of antidepressants (Table-6) are available for
management of depression and in general all the antidepressantshave been shown to have nearly equal efficacy in the management of depression. Antidepressant medication may be used as initial treatment modality for patients with mild, moderate, or severe depressive episode.The selection of antidepressant medications may be based on patient specific and drug specific factors, as given in Table-7.
In general, because of the side
effect and safety profile, selective serotonin reuptake inhibitors
(SSRIs) are considered to be the first line antidepressants. Other
preferred options include tricyclic antidepressants, mirtazapine,
bupropion, and venlafaxine. Usually the medication must be
started in the lower doses and the doses must be titrated,
depending on the response and the side effects experienced.Dose and duration of antidepressants
Visits may be kept frequent enough to monitor [side effects] and address suicidality and to promote treatment adherence.
Improvement with pharmacotherapy can be observed after
4-6 weeks of treatment. If at least a moderate improvement is
not observed in this time period, reappraisal and adjustment
of the pharmacotherapy should be considered.Psychotherapeutic Interventions
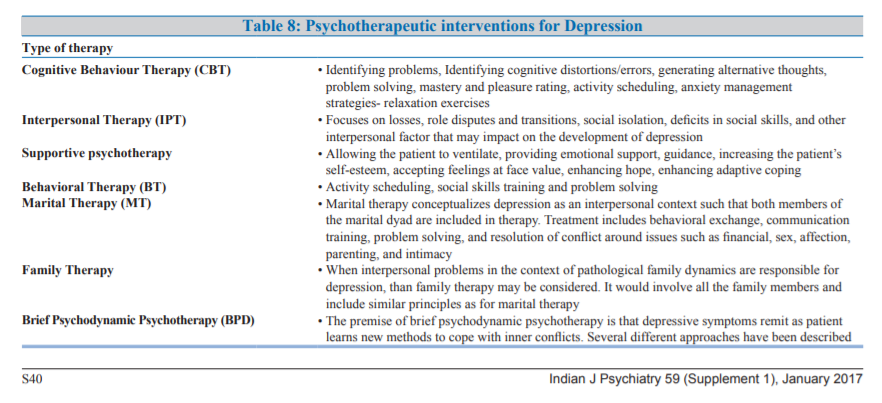
Various psychotherapeutic interventions which may be considered based on feasibility, expertise available and affordability are shown in Table-8.
Cognitive behavioral therapy (CBT) and interpersonal therapy are the psychotherapeutic approaches that have the best documented efficacy in the literature for management of depression.
Psychoeducation to the patient and, when appropriate, to
the familyEducation concerning depression and its treatments can
be provided to all patients. When appropriate, education
can also be provided to involved family members.Education regarding available treatment options will help patients make informed decisions, anticipate side effects and adhere to treatments.
Another important aspect of providing education is informing the patient and especially family about the lag period of onset
of action of antidepressants. Important components of
psychoeducation are given in Table-9.Combination of pharmacotherapy and Psychotherapy
There is class of patients who may require the combination
of pharmacotherapy and psychotherapy. In general, the
same issues that influence the choice of medication or
psychotherapy when used alone should be considered
when choosing treatments for patients receiving combined
therapy.
One approach to depression and other mental health problems is the development and strengthening of problem-solving skills. See the 2017 Bright Ideas PROBLEM-SOLVING SKILLS TRAINING FOR EVERYDAY LIVING [Link is to the PDF].