In addition to today’s outstanding resource, please see and review Links To And Excerpts From “The challenge of posterior circulation stroke (PCIS)” From EMC’s Episode 171
Posted on July 6, 2022 by Tom Wade MD.
In this post, I link to and excerpt from EMU 2017 DIZZINESS AND VERTIGO By Walter Himmel MD from Emergency Medicine Cases Episode 99 Highlights from EMU 2017. Accessed 7-7-2022.
Dr. Himmel’s portion of the podcast runs from 48:00-1:07:00
All that follows is from the above show notes.
Acute Vestibular Syndrome Pitfalls & Fallacies from EMU 2017 with Walter Himmel
Vertigo has been discussed EM Cases before – Episode 6(Walter Himmel & Dan Selchen) and Episode 45 (Stuart Swadron), but here are some important highlights that will help you in the diagnosis and disposition of acute vestibular syndromes.
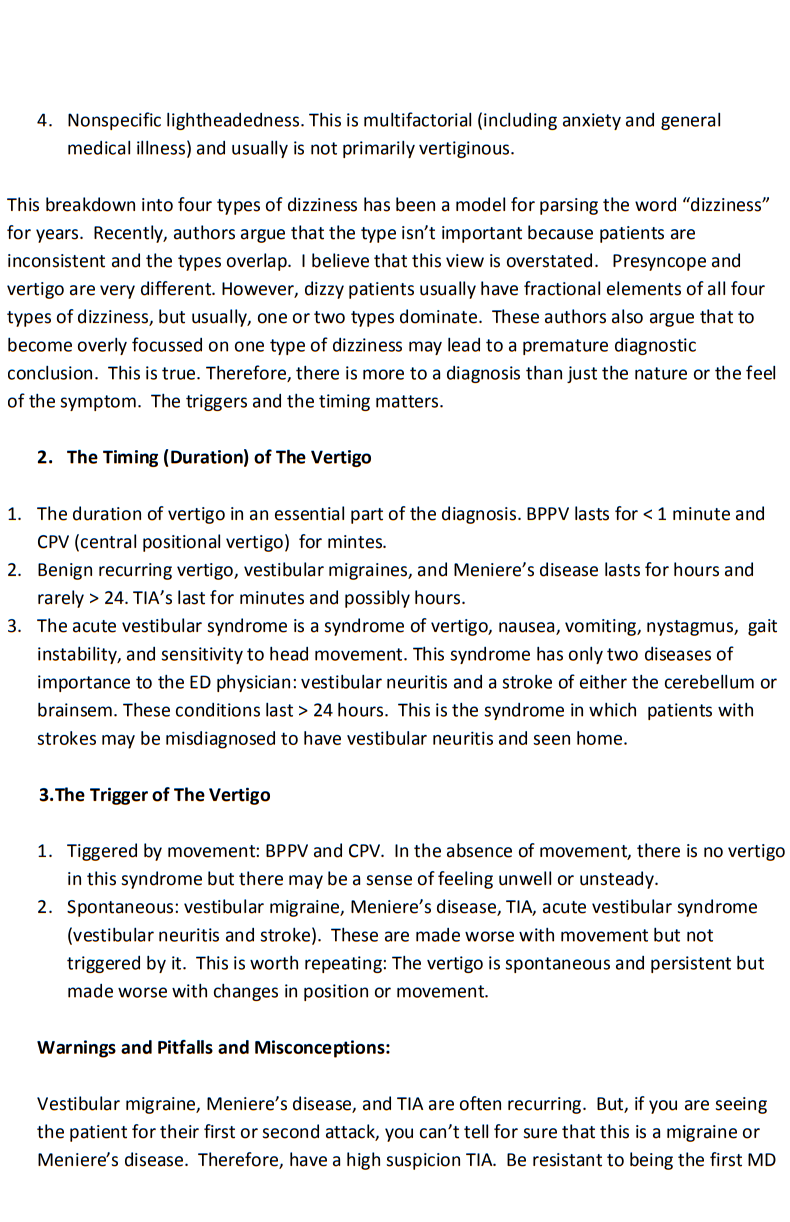
Acute vestibular syndrome is defined as continuous vertigo (ie. hours) with nausea, vomiting, movement intolerance and nystagmus. The challenge is to distinguish between the benign peripheral etiology of vestibular neuritis and the serious central etiology of stroke.
Timing is everything. A truly abrupt onset is more likely a stroke or TIA than vestibular neuritis. BPPV presents differently to acute vestibular syndromes, with only one minute of vertigo always triggered by movement, never coming on at rest, with relatively asymptomatic periods in between the episodes of vertigo. All vertigo, no matter what the cause is worsened by movement. The big pitfall is to diagnose BPPV just because the vertigo is worse with movement or when you do a Dix-Hallpike maneuver. BPPV only occurs with movement. If a patient describes a history of lying perfectly still and suddenly gets vertigo, that’s not BPPV.
Even with BPPV, the patient will say that they is constantly “dizzy” whether they move or not. However, after a minute and with no further movement, the vertigo will stop in BPPV. The history may be difficult to analyze. The spinning or delusion of movement will stop. However, the sense of unsteadiness or slight disequilibrium may persist. The important word in the history is “bed.” These patients get a sudden triggering of vertigo when they roll over or lift their head up in bed.
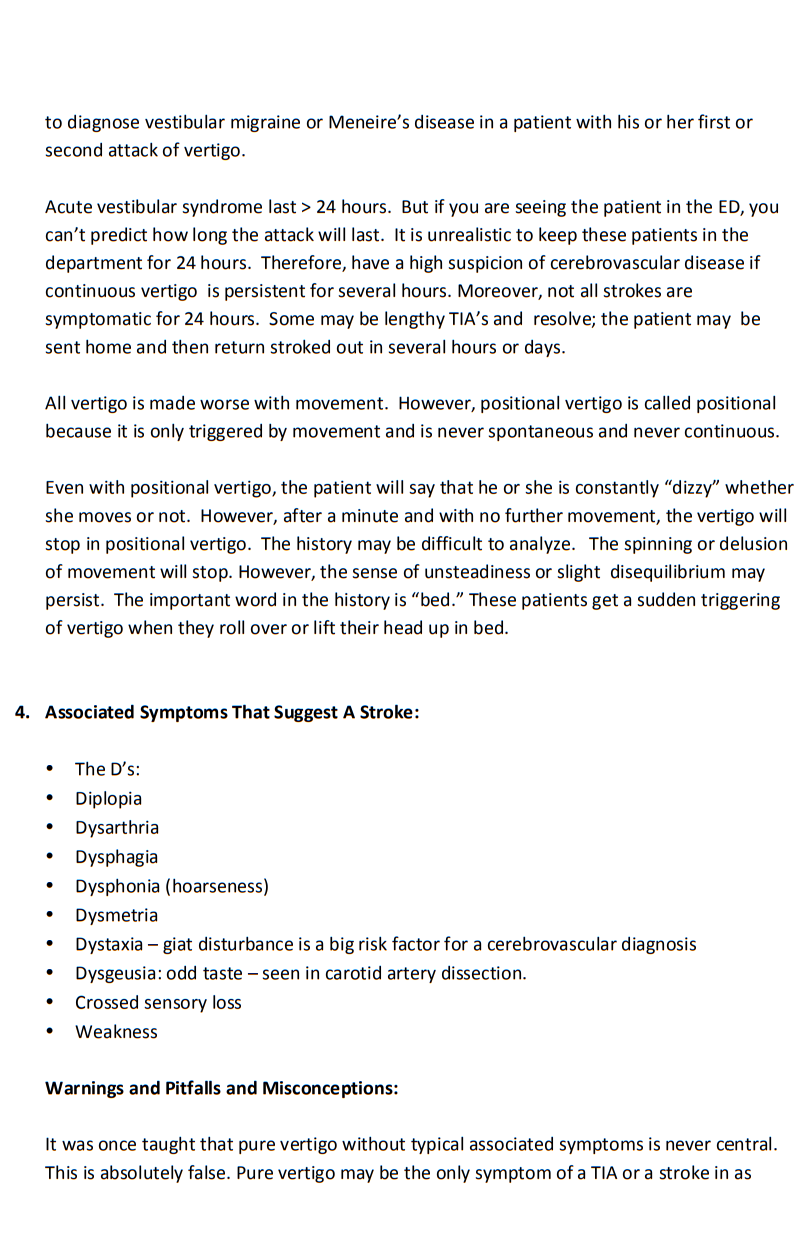
Fallacies of Vertigo
#1: Patients with central vertigo must have at least one of the 5 Ds (Dizziness, Diplopia, Dysarthria, Dysphagia and Dysmetria*) or long tract signs.
Stroke may present as isolated vertigo with only minor gait disturbance without any of the 5 Ds or long tract signs.
*Dysmetria: What Is It, Causes, Diagnosis, Treatment, and More:
“Dysmetria is the inability to control the distance, speed, and range of motion necessary to perform smoothly coordinated movements. Dysmetria is a sign of cerebellar damage, and often presents along with additional signs, such as loss of balance and poor coordination of walking, speech, and eye movements.”
“Presentation: Inability to control the distance, speed, or range of motion needed for co-ordinated movements.”
“Cause: Damaged Cerebellum possibly resulting from
- Brain Trauma
- Brain Tumors
- Metabolic Diseases
- Demyelinating or Degenerative Disorders”
“Diagnostic Tests
- Finger to Nose Test
- Heel to Shin Test”
Fallacies of Vertigo (continued)
#2: Unidirectional nystagmus is always a sign of peripheral vertigo.
While unidirectional nystagmus usually points to a peripheral cause, it can occur with central causes of vertigo. Unidirectional nystagmus does not, on it’s own, rule in a peripheral cause. If nystagmus is definitely multidirectional, or purely vertical with no rotatory component the cause is almost certainly central. The HINTS exam can help differentiate a peripheral vs. central cause of acute vestibular syndrome, although this is not perfect
#3: Perform a Dix Hallpike test on every vertigo patient.
- This test is only useful for patients with truly paroxysmal, positional vertigo
- Only perform this on those patients who have a good story for BPPV
- POSITIVE test if 1) onset of vertigo + 2) vertical rotatory nystagmus
- All vertiginous disorders will worsen with movement, regardless of the cause
#4: Young patients do not have strokes.
While strokes are certainly less common in patients <50 years of age, about 1/4 of strokes are caused by vertebral artery dissections in young patients.
High Risk Scenarios in Acute Vestibular Syndrome
Be cautious of the patient with vertigo plus pain.
- Headache – consider plain head CT to rule out a cerebellar hemorrhage
- Neck pain – consider CT angiogram or MR angiogram of the head and neck to rule out vertebral artery dissection (note that not everyone with vertigo needs an angiogram. Angiograms still need to be done selectively based on all the pearls and misconceptions that we’ve just reviewed here)
- 50% of vertebral artery dissections are painless
Discharge diagnosis: vertigo NYD.
- Vertigo is a symptom, not a diagnosis
- If you can’t describe a specific diagnosis, the patient should probably not go home
Can’t ambulate, can’t discharge.
- This rule is true for nearly all emergency department dispositions
- If this is the case, you will certainly need imaging as well as a discussion with your consultants
These two links are to Dr. Newman-Toker’s site describing beautifully the HINTS tests that he
has extensively written about in multiple articles.
http://content.lib.utah.edu/cdm/ref/collection/ehsl-dent/id/6 or
http://www.kaltura.com/tiny/2jsvu