Today, I review, link to, and excerpt from Inflammation and Cardiovascular Disease: 2025 ACC Scientific Statement: A Report of the American College of Cardiology [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. J Am Coll Cardiol. 2025 Sep 29:S0735-1097(25)07555-2. doi: 10.1016/j.jacc.2025.08.047. Online ahead of print.
All that follows is from the above resource.
Abstract
The crucial role of inflammation in the pathogenesis and clinical outcomes of cardiovascular disease (CVD) has recently gained increased attention. In particular, residual inflammation, measured with high-sensitivity C-reactive protein (hsCRP) remains strongly predictive of recurrent events, even in statin-treated patients. Similarly, elevated hsCRP in apparently healthy individuals identifies a higher-risk group in whom statin therapy significantly reduces the risk of first major CVD events even if LDL-cholesterol is normal. This report provides an updated understanding of the role of chronic, low-grade inflammation in CVD and highlights new seminal research findings, especially in atherosclerosis, myocardial infarction, heart failure, and pericarditis. Consensus recommendations are summarized for screening, evaluation, and CVD risk assessment; inflammatory biomarkers in cardiovascular imaging; inflammation inhibition in behavioral and lifestyle risks; and anti-inflammatory approaches in primary and secondary prevention as well as in heart failure and other CVDs. This report also addresses current challenges and future opportunities. For example, it cautions that not all trials of anti-inflammatory therapy in secondary prevention have been successful and such trial evidence is needed before broad recommendations for other agents can be made. Additionally, in successful trials, the interplay between inflammation and key physiological systems often remains incompletely examined. Another promising area of research is the role that novel special pro-resolving bioactive lipid molecules play in promoting the resolution of inflammation and CVD risk reduction. In aggregate, the evidence linking inflammation with atherosclerotic CVD is no longer exploratory but is compelling and clinically actionable. The time for taking action has now arrived.Introduction
The American College of Cardiology (ACC) has a long history of developing documents to complement clinical practice guidelines. Among these documents, scientific statements represent a novel approach to inform clinicians about areas where the scientific evidence is new and evolving or where sufficient data are more limited. Recently, the role of inflammation in cardiovascular disease (CVD) has gained significant attention, prompting a reevaluation of traditional paradigms of the pathogenesis and clinical outcomes of CVD. This scientific statement provides clinicians with an updated understanding of the role inflammation plays in CVD. The statement’s scope includes new research findings on the role of inflammation in atherosclerosis, myocardial infarction, heart failure (HF), and pericarditis. It also emphasizes primary and secondary prevention and inflammatory pathways in behavioral and lifestyle risks.Definitions and Classifications
Adaptive immune cell: A specialized immune cell that provides a specific, long-lasting immune response to pathogens. It recognizes unique antigens and can form immune memory, enabling faster and stronger response upon re-exposure.Augmented immunoinflammatory response: A heightened immune and inflammatory reaction that goes beyond what is necessary to protect the body, often leading to tissue damage, chronic inflammation, or exacerbation of disease. These responses have been linked with increased mortality and morbidity in chronic HF.Cardioimmunology: An emerging interdisciplinary field that studies the interactions between the immune system and the cardiovascular system, with a focus on how immune cells, molecules, and inflammatory processes influence cardiovascular function in health and disease.Clonal hematopoiesis of indeterminate potential: A condition characterized by the presence of somatic mutations in blood-forming (hematopoietic) stem cells, leading to the expansion of genetically identical blood cell clones, without evidence of blood cancer or other hematological disease.Efferocytosis: A specialized form of phagocytosis where apoptotic cells are cleared by immune cells—primarily macrophages and dendritic cells—without triggering inflammation, thus maintaining tissue homeostasis and promoting resolution of inflammation.Immune checkpoint inhibitor: A class of cancer immunotherapy drug that blocks inhibitory pathways (“checkpoints”) used by tumors to evade immune detection, thereby releasing the brakes on T cells and enhancing its ability to attack cancer cells.Immune dysregulation: An abnormally functioning immune system—one that is either overactive, underactive, or inappropriately responding to stimuli.Immunomodulatory strategy: A therapeutic approach that aims to alter or regulate the immune system’s activity—by enhancing, suppressing, or restoring balance—to treat diseases or promote health.Innate immune cell: The first line of defense in the immune system. It responds rapidly and nonspecifically to invading pathogens or tissue injury, without prior exposure or memory formation.Janus kinase inhibitor: A targeted small-molecule drug that blocks the activity of a family of intracellular tyrosine kinases (Janus kinases) involved in cytokine signaling. By inhibiting Janus kinases, this drug reduces the activity of proinflammatory and immune-related pathways.Parainflammation: A state of low-grade, chronic, subclinical inflammation that occurs when tissues are under mild or persistent stress—not enough to trigger full immune activation, but enough to disrupt normal cellular function. Tissue macrophages are important drivers of this response.Plasminogen activator inhibitor-1: A serine protease inhibitor that functions as the principal inhibitor of tissue-type plasminogen activator and urokinase-type plasminogen activator, the enzymes responsible for converting plasminogen to plasmin, the key enzyme in fibrinolysis.Perivascular fat attenuation index: A quantitative imaging marker derived from computed tomography scans that measures the density (attenuation) of fat surrounding blood vessels, especially coronary arteries.Perivascular fat phenotyping: The process of analyzing the characteristics of the fat tissue surrounding blood vessels to understand its biological behavior and impact on cardiovascular health and disease.Residual inflammatory risk: Persistent, elevated risk of cardiovascular events that manifest as chronic, low-grade inflammation in some individuals despite optimal management of traditional risk factors. This risk is most commonly measured with high-sensitivity C-reactive protein (hsCRP).Specialized pro-resolving lipid mediator (SPM): A bioactive lipid molecule derived from polyunsaturated fatty acids—mainly omega-3 fatty acids—that actively promote the resolution of inflammation without causing immunosuppression.Vulnerable plaque: A type of atherosclerotic plaque that has a high risk of rupturing and triggering a thrombus formation that may lead to an acute cardiovascular event, such a myocardial infarction or stroke.Abbreviations
Abbreviation Meaning/Phrase ASCVD atherosclerotic cardiovascular disease CHD coronary heart disease CHIP clonal hematopoiesis of indeterminate potential CVD cardiovascular disease DHA docosahexaenoic acid EPA eicosapentaenoic acid HF heart failure HFpEF heart failure with preserved ejection fraction hsCRP high-sensitivity C-reactive protein IL interleukin LDL low-density lipoprotein LV left ventricular SMuRF standard modifiable risk factor SPM specialized pro-resolving lipid mediator Background
In March 2002, the Centers for Disease Control and Prevention and the American Heart Association convened a workshop to assess the state of the science on inflammation and provide guidance on the use of inflammatory markers for predicting CVD risk in clinical and public health practice.1 The resulting scientific statement identified hsCRP as the analyte of choice in specific clinical settings, such as in persons at intermediate CVD risk, where hsCRP might guide further evaluation and therapy; however, the 2002 statement discouraged inflammatory marker use in widespread population screening due to insufficient evidence. The statement further called for rigorous randomized clinical trials to clarify the utility of inflammatory markers in CVD treatment planning.Since that workshop, substantial progress has been made in the basic, clinical, and population science research in inflammation and CVD. It is now well established that chronic, silent, low-grade inflammation, together with key mediators like cytokines, chemokines, and acute-phase reactants, plays a pivotal role in atherosclerotic plaque formation, progression, rupture, and thrombogenesis that lead to acute coronary syndrome. Additionally, inflammatory pathways, driven by immunoregulatory influences, contribute to endothelial dysfunction, leukocyte infiltration of the subendothelial space, foam cell formation, and apoptosis that further contribute to atherogenesis. These advances have paved the way for several novel therapeutic avenues focused on modulating inflammation to reduce CVD burden and risk. In the following sections of this scientific statement, insights from seminal publications on these topics are discussed and consensus recommendations for clinical practice are summarized in Table 1.Table 1 Table of Consensus Recommendations
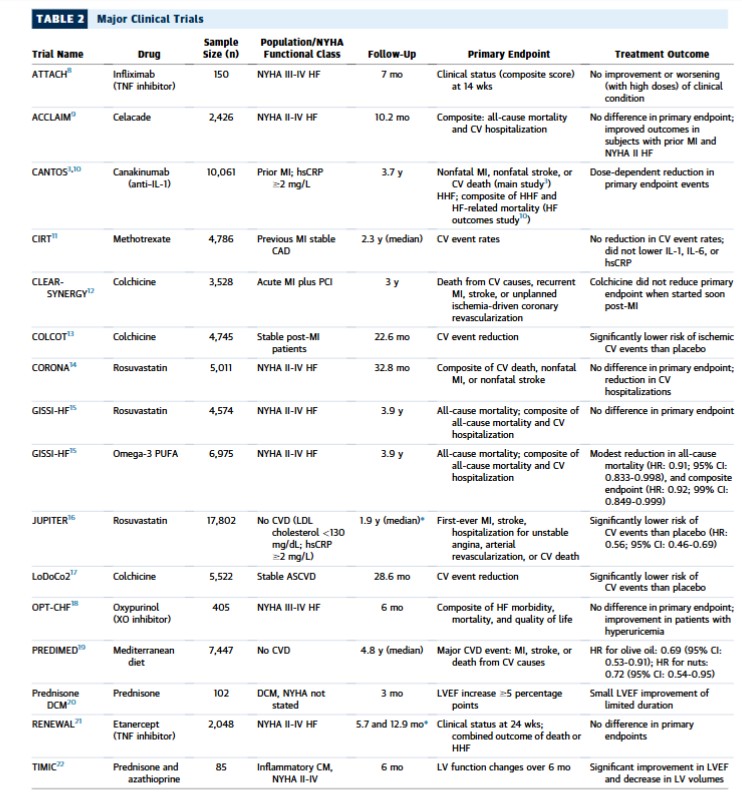
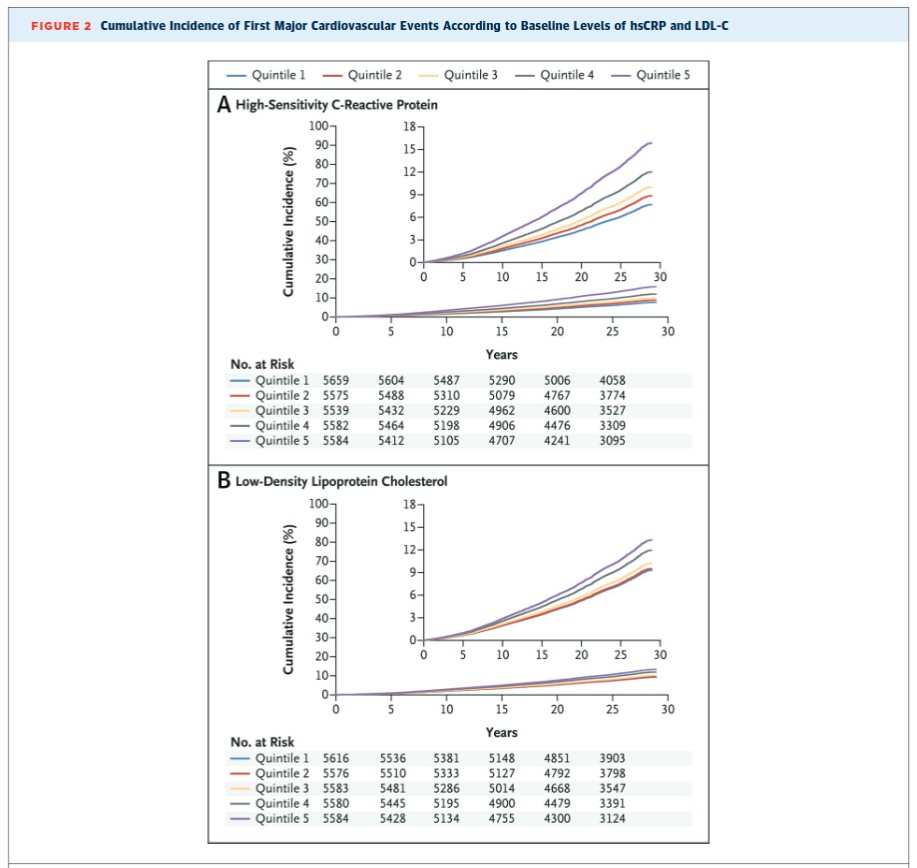
Evaluation and Risk Assessment Biomarkers ▪ Because clinicians will not treat what they do not measure, universal screening of hsCRP in both primary and secondary prevention patients, in combination with cholesterol, represents a major clinical opportunity and is therefore recommended.▪ Other inflammatory biomarkers such as serum amyloid A, IL-6, fibrinogen, white blood cell count, neutrophil-to-lymphocyte ratio, and EPA/AA ratio also predict cardiovascular risk; however, routine evaluation of these adds little to hsCRP and only hsCRP is recognized by regulatory agencies and has consistently been used in major cardiovascular outcome trials.Imaging biomarkers ▪ Imaging biomarkers to detect vascular inflammation are promising in research but should not be used in routine clinical settings.hsCRP screening and inflammation inhibition in primary prevention ▪ A single measurement of hsCRP (>3 mg/L) can be used in routine clinical practice to identify individuals at increased inflammatory risk if the patient is not acutely ill.▪ In individuals with increased inflammatory burden, an early initiation of lifestyle interventions is recommended to reduce inflammatory risk.▪ In primary prevention, the finding of a persistently elevated hsCRP level should lead to consideration of initiation or intensification statin therapy, irrespective of LDL cholesterol.hsCRP screening and anti-inflammatory approaches in secondary prevention ▪ Among individuals with known cardiovascular disease both treated and not treated with statins, hsCRP is at least as powerful a predictor of recurrent vascular events as that of LDL cholesterol, demonstrating the importance of “residual inflammatory risk” in contemporary practice.▪ Among individuals taking statin therapy, consideration should be given to increase dosage into the higher intensity range if hsCRP levels remain >2 mg/L, irrespective of LDL cholesterol.▪ Low-dose colchicine reduces cardiovascular events among individuals with chronic stable atherosclerosis and is the first FDA approved anti-inflammatory agent for this purpose.▪ Low-dose colchicine is intended to be used as an adjunct to lipid lowering; however, colchicine has not proven effective when initiated at the time of acute ischemia and should be avoided among individuals with significant liver or renal disease.▪ Several novel anti-inflammatory agents, including IL-6 inhibitors, are now being evaluated in ongoing randomized trials in the settings of chronic kidney disease, dialysis, HFpEF, and acute coronary syndrome.Inflammatory pathways in behavioral and lifestyle risks ▪ Focus on anti-inflammatory patterns like the Mediterranean or DASH diet.○ Emphasize consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil.○ Increase dietary intake of omega-3 fatty acids; 2-3 fish meals/wk are recommended—preferably fatty fish high in EPA+DHA.○ Minimize red and processed meats, refined carbohydrates, and sugary beverages.▪ Engage in ≥150 min/wk of moderate exercise or 75 min/wk of intense exercise.▪ Quit smoking to reduce chronic low-grade inflammation.▪ Maintain a healthy weight to attenuate systemic inflammation.Inflammation in HF and other CVD ▪ Inflammatory and immune markers such as hsCRP and IL-6 may be used as risk predictors in chronic HF.▪ EPA+DHA may be considered as part of the management of patients with NYHA functional class II-IV HF, irrespective of etiology or LVEF.▪ Statins may be considered as a part of management for patients with ischemic HF and >60 years of age.Anti-inflammatory therapy for recurrent pericarditis ▪ IL-1 blockade may be considered among select patients with multiple recurrent episodes of colchicine- and steroid-resistant pericarditis, with hsCRP levels >10 mg/L, in the absence of tuberculosis.▪ Novel anti-inflammatory therapies for recurrent pericarditis represent an important therapeutic advance for high-risk patients.AA = arachidonic acid; CVD = cardiovascular disease; DASH = Dietary Approaches to Stop Hypertension; DHA = docosahexaenoic acid; EPA = eicosapentaenoic acid; FDA = U.S. Food and Drug Administration; HF = heart failure; HFpEF = heart failure with preserved ejection fraction; hsCRP = high-sensitivity C-reactive protein; IL-1 = interleukin-1; IL-6 = interleukin-6; LDL = low-density lipoprotein; LVEF = left ventricular ejection fraction.Based on these biological advances on consistent epidemiological replications in both primary and secondary prevention, and a series of robust, high-quality randomized clinical trials, near-universal screening for hsCRP along with targeted chronic low-grade inflammation inhibition is today warranted in the prevention and clinical management of CVD.2,3 There is now compelling evidence of adverse CVD outcomes in the setting of elevated markers of inflammation and that targeting inflammation significantly reduces recurrent CVD events. This is true in the setting of cardiovascular health promotion in apparently healthy individuals, in primary prevention among persons with CVD risk factors, and in secondary prevention strategies in individuals with established CVD. Inflammation also plays a pivotal role in the lifestyle choices and behavioral risks, as well as the social and environmental determinants that predispose to CVD.Although most of the compelling clinical trial evidence for the role of inflammation in CVD originates from coronary atherosclerosis and myocardial infarction, there is emerging evidence in several other CVDs that provides hope for improved therapeutic targeting for CVD prevention and treatment. For example, evidence from preclinical and clinical studies in both HF and recurrent pericarditis have increased our understanding of the role of inflammation and immune dysregulation in specific treatment strategies.4-7 Emerging evidence also exists for other CVD and cardiovascular imaging. Additional supporting clinical trials are summarized in Table 2.2,3 Remaining gaps in knowledge that present opportunities for research in basic, clinical, and population science are identified, and a call to action is highlighted for clinical practice and research.Table 2 Major Clinical Trials
Evaluation and risk assessment
Biomarkers
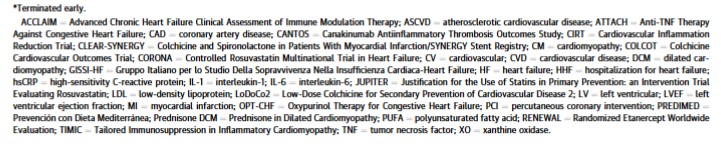
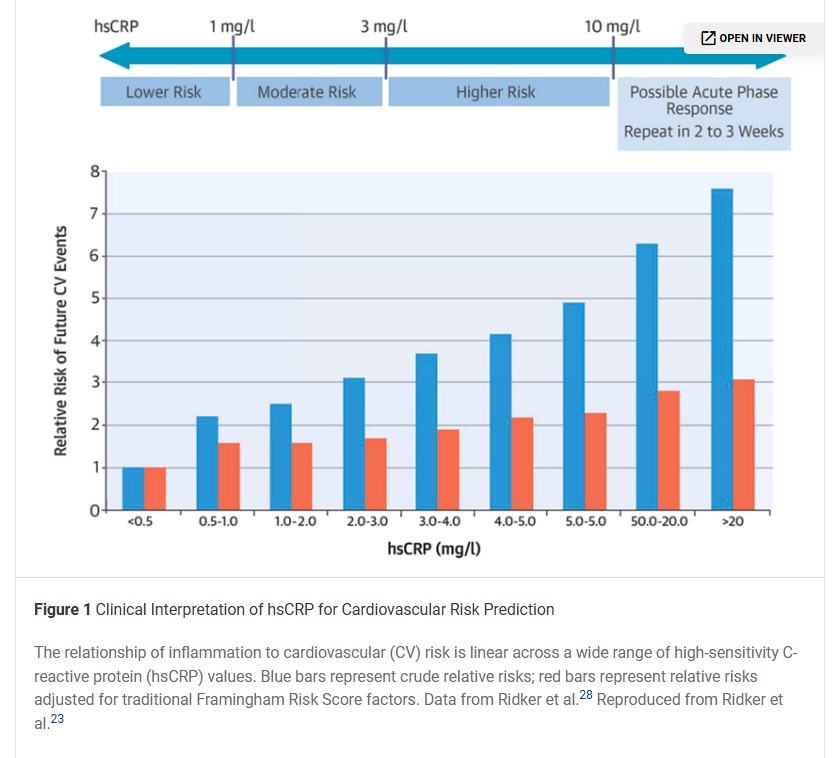
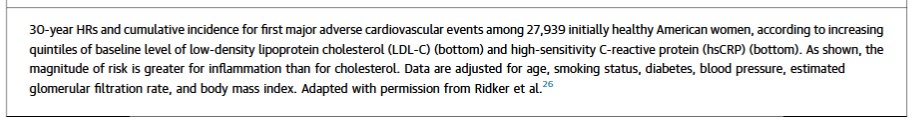
In clinical practice, silent vascular inflammation is commonly evaluated through blood measurement of hsCRP, which adds prognostic information about cardiovascular risk comparable with that of blood pressure and cholesterol. In general, levels of hsCRP <1, 1 to 3, and >3 mg/L connote lower, average, and higher relative cardiovascular risk, respectively, when interpreted in the context of other traditional factors (Figure 1).23,24 hsCRP levels >10 mg/L may reflect a transient infectious process or other acute-phase response and thus should be repeated in 2 to 3 weeks with the lower value, not the average, used for risk prediction;23,25 however, persistently high hsCRP values may be seen and do not necessarily represent false-positive findings, because many individuals with chronic autoinflammatory disorders also suffer from premature atherosclerosis.26When measured in stable outpatients, the long-term stability and variability of hsCRP is comparable with that of low-density lipoprotein (LDL) cholesterol and blood pressure. Moreover, the long-term information content implicit in hsCRP appears to be at least as large as that associated with LDL cholesterol. For example, in a recent prospective study inclusive of 27,939 initially healthy U.S. women, a single random assessment of hsCRP provided a greater spread of risk for future cardiovascular events during the next 30 years when directly compared with either LDL cholesterol or lipoprotein(a) (Figure 2).27 Similar contemporary data demonstrating the independent and additive clinical utility of LDL, hsCRP, and lipoprotein(a) have recently been presented from the EPIC (European Prospective Investigation into Cancer)-Norfolk study inclusive of 17,087 men and women followed for 20 years.28Alternative inflammatory biomarkers, including fibrinogen, lipoprotein-associated phospholipase-A2, myeloperoxidase, serum amyloid A, total white blood cell count, neutrophil-to-lymphocyte ratio, eicosapentaenoic acid (EPA)/arachidonic acid ratio, and interleukin-6 (IL-6), have also found predictive value but generally have not proven superior to hsCRP and often are not widely available in standardized commercial formats. As will be described in the following text, several novel approaches to inflammation imaging hold promise for the detection of silent vascular inflammation. Further, imaging for coronary artery calcium is an efficient method to detect underlying atherosclerotic disease and the strongest risk predictor. Yet, although coronary artery calcium can tell clinicians who to treat, it cannot tell clinicians what to use for treatment. As such, universal screening for hsCRP, along with LDL cholesterol and lipoprotein(a), among individuals suspected to have atherosclerotic risk is becoming a common approach to vascular disease evaluation and risk assessment.29 hsCRP screening should be done when patients are stable and not during an acute infection or during other acute clinical events.Consensus recommendations: evaluation and risk assessment, biomarkers
▪ Because clinicians will not treat what they do not measure, universal screening of hsCRP in both primary and secondary CVD prevention represents a major clinical opportunity and is therefore recommended.▪ Whereas several other inflammatory biomarkers, such as IL-6, fibrinogen, and neutrophil-to-lymphocyte ratio, also predict risk, routine evaluation of these adds little to hsCRP.Imaging biomarkers
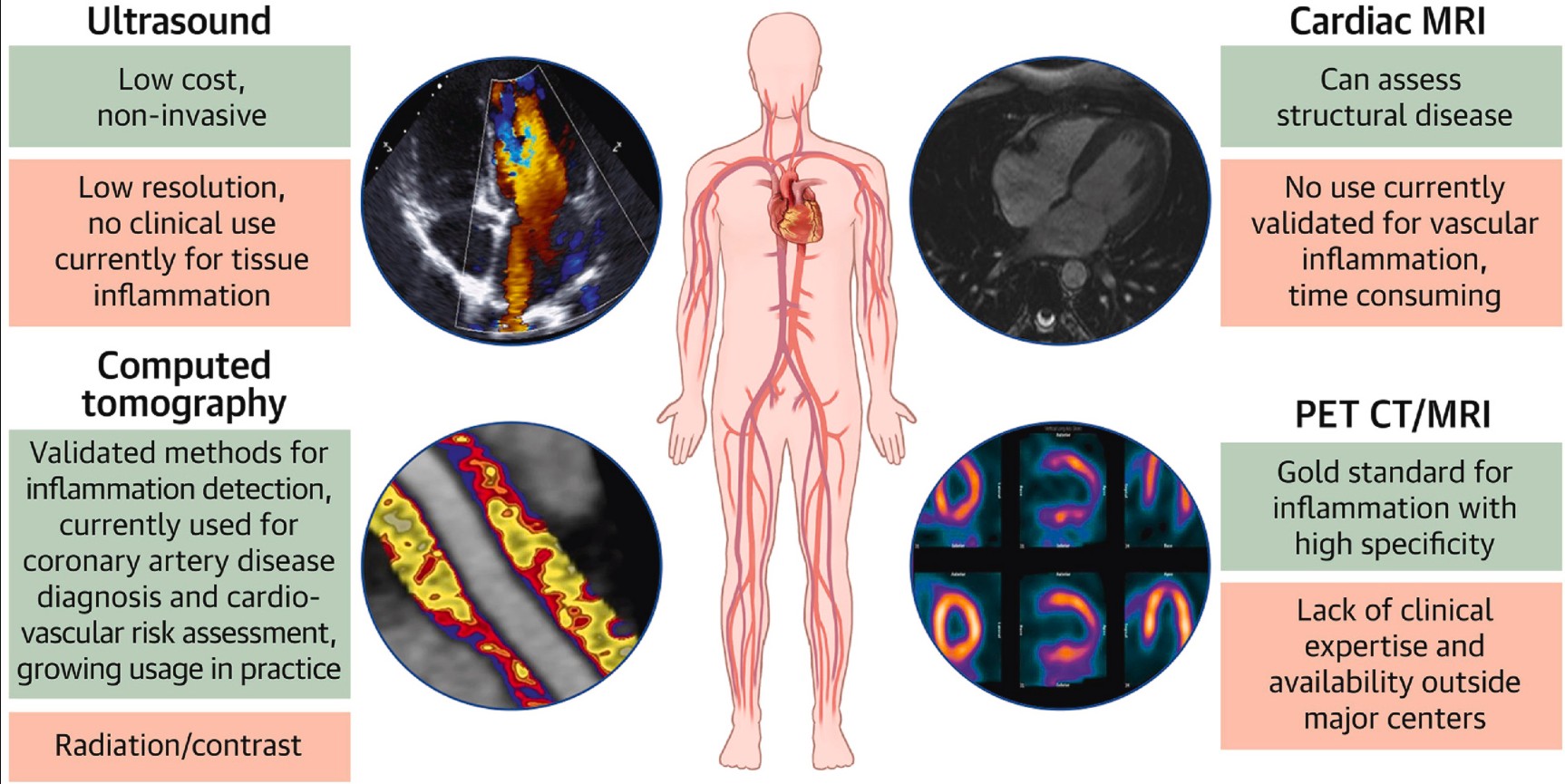
Noninvasive imaging techniques for assessing local vascular inflammation might represent a valuable approach to enhance risk prediction and even guide the management of patients with residual inflammatory risk in the future. To date, there are several imaging modalities, including computed tomography, cardiac magnetic resonance, ultrasound, and positron emission tomography imaging with fluorodeoxyglucose (Figure 3),30 that might help to identify inflamed atherosclerotic plaques and perivascular inflammation. Both conditions are known to drive the progression of atherosclerosis and plaque rupture.30 These modalities, however, have unique advantages and limitations29-31 and currently are mainly used in research. A recently introduced and promising noninvasive computed tomography–derived imaging biomarker may directly identify both inflamed coronary arteries without atherosclerosis and vulnerable atherosclerotic plaques prone to rupture by using perivascular fat phenotyping.32 Named perivascular “fat attenuation index,” this method has been already shown to predict future coronary events independently of the calcium score and traditional cardiovascular risk factors.33 Although imaging biomarkers might represent a promising research tool for the integration of vascular inflammation into personalized cardiovascular risk stratification, there are several issues to be addressed, such as a better understanding of the interplay with circulating inflammatory biomarkers, effects of anti-inflammatory treatment on plaque progression, and local arterial inflammation. Although preliminary, results of the small EKSTROM (Effect of Colchicine on Progression of Known Coronary Atherosclerosis in Patients With Stable Coronary Artery Disease Compared to Placebo) trial34 showed that low-dose colchicine therapy modestly reduced total plaque volume in stable patients with coronary heart disease (CHD) compared with those taking placebo after 1 year are of interest and consistent with trial data demonstrating efficacy of low-dose colchicine in patients with established atherosclerotic cardiovascular disease (ASCVD).Figure 3Consensus recommendation: imaging biomarkers
▪ Imaging biomarkers to detect vascular inflammation are promising in research but should not be used in routine clinical settings.hsCRP screening and inflammation inhibition in primary prevention
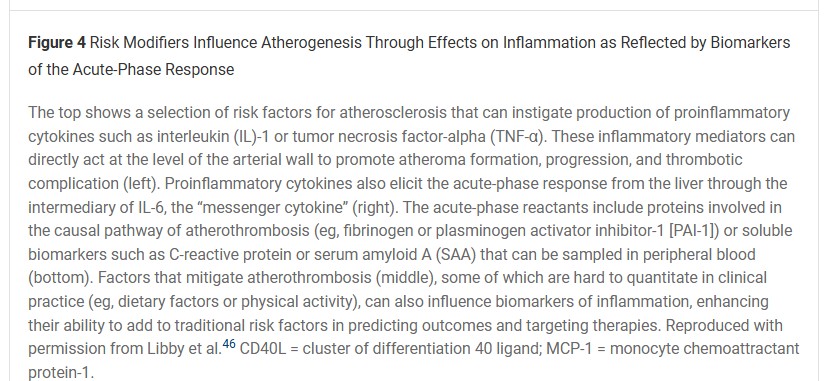
The seminal Physician’s Health Study35 in 1997 initiated a series of epidemiological studies in primary prevention, providing unequivocal evidence that elevated hsCRP concentration might serve as a robust predictor of future ASCVD events among apparently healthy individuals, independent of conventional risk factors. A comprehensive meta-analysis of 54 studies that included 160,309 individuals without a history of ASCVD has further supported these findings, showing that a 1-SD increase in hsCRP concentration was associated with a 37% increased risk of CHD and a 55% increased risk of cardiovascular death.36 Interestingly, the magnitude of association between elevated hsCRP (per 1-SD increase) and incident CVD was largely comparable with that found for systolic blood pressure36 and appeared to be stronger than the associations observed for conventional lipids (total, non–high-density lipoprotein, or LDL cholesterol)26,36 or lipoprotein(a).26,37 Elevated hsCRP also predicts incident CHD among individuals without standard modifiable risk factors (SMuRFs) at baseline, thereby extending its utility beyond traditional risk categories.38,39In general, the prevalence of a moderate to higher risk hsCRP levels ≥2 mg/L in adults in the primary prevention setting may vary from approximately 30% to 35% in Europe37,40 to 50% in the United States.41,42 This could become an important public health issue in the near future, especially due to the obesity epidemic, because body mass index (in combination with smoking) is currently considered an important determinant of longitudinal hsCRP changes.43 More importantly, already 15% of U.S. adolescents aged 12 to 19 years have reported increased hsCRP concentrations.44 Considering that treatment of lifestyle risk factors such as increased body weight, smoking, physical inactivity, and unhealthy diet have a strong anti-inflammatory effect,45,46 hsCRP is an easily measurable clinical biomarker that should be broadly used as a tool to identify and monitor those with an inflammatory burden, especially in the case of primordial prevention (Figure 4).46Figure 4The initial evidence that inflammation might become a valuable therapeutic drug target came from statin trials, which showed that statin administration reduces both LDL cholesterol and hsCRP, with reductions in both parameters contributing to beneficial effects on outcomes. A post hoc analysis of AFCAPS/TexCAPS (Air Force/Texas Coronary Atherosclerosis Prevention Study)47 revealed that the reduction in major adverse cardiovascular events observed in subjects treated with lovastatin was not limited to those with elevated LDL cholesterol levels (≥149.1 mg/dL): similar risk reduction was also seen in individuals with normal LDL cholesterol but elevated hsCRP (>1.6 mg/L) levels (47% and 42% relative risk reduction for 5 years, respectively).47 The subsequent JUPITER (Rosuvastatin to Prevent Vascular Events in Men and Women With Elevated C-Reactive Protein) study16 was the first randomized placebo-controlled trial to investigate the effect of 20 mg of rosuvastatin in individuals with LDL cholesterol levels <130 mg/dL who also had hsCRP concentrations of ≥2 mg/L. The study was prematurely terminated, showing a 47% reduction in the primary endpoint (Figure 5).16 Further analyses from the JUPITER study demonstrate considerable efficacy of rosuvastatin compared with that of placebo among trial participants who had no SMuRFs but who were only at risk due to elevated hsCRP, a group described as “SMuRF-less but inflamed.”48 Recent studies have further indicated that bempedoic acid might also possess anti-inflammatory properties, with a reported 20% to 30% reduction in hsCRP, which was comparable with the extent of LDL cholesterol lowering seen with this treatment.49 Although a potentially larger overall cardiovascular benefit has been seen in the primary prevention cohort of the CLEAR (Cholesterol Lowering via Bempedoic Acid, an ACL-Inhibiting Regimen) Outcomes trial,49 it is still unknown whether the reduction of hsCRP in individuals without ASCVD taking bempedoic acid would result in a favorable outcome.Figure 5Figure 5 Cumulative Incidence of Cardiovascular Events in the JUPITER Primary Prevention Trial of Patients With Low Levels of LDL Cholesterol But Elevated hsCRPPanel A shows the cumulative incidence of the primary endpoint (nonfatal myocardial infarction, nonfatal stroke, arterial revascularization, hospitalization for unstable angina, or confirmed death from cardiovascular causes). The HR for rosuvastatin, as compared with placebo, was 0.56 (95% CI: 0.46-0.69; P < 0.00001). Panel B shows the cumulative incidence of nonfatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes, for which the HR in the rosuvastatin group was 0.53 (95% CI: 0.40-0.69; P < 0.00001). Panel C shows the cumulative incidence of arterial revascularization or hospitalization for unstable angina, for which the HR in the rosuvastatin group was 0.53 (95% CI: 0.40-0.70; P < 0.00001). Panel D shows the cumulative incidence of death from any cause, for which the HR in the rosuvastatin group was 0.80 (95% CI: 0.67-0.97; P = 0.02). In each panel, the inset shows the same data on an enlarged y-axis and on a condensed x-axis. Reproduced with permission from Ridker et al.16 hsCRP = high-sensitivity C-reactive protein; JUPITER = Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin; LDL = low-density lipoprotein.Consensus recommendations: hsCRP screening and inflammation inhibition in primary prevention
▪ Measurement of hsCRP (>3 mg/L) can be used in routine clinical practice to identify primary prevention individuals at increased inflammatory risk as long as the patient is not acutely ill.▪ In individuals with increased inflammatory burden, an early initiation of lifestyle interventions is recommended to reduce inflammatory risk.▪ In primary prevention, the finding of a persistently elevated hsCRP level should lead to consideration of initiation or intensification statin therapy, irrespective of LDL cholesterol.hsCRP screening and anti-inflammatory approaches in secondary prevention
As described previously for primary prevention, there are abundant contemporary data in secondary prevention that measurement of hsCRP effectively identifies individuals at high risk for recurrent cardiovascular events. In a contemporary overview inclusive of 31,245 statin-treated patients participating in the PROMINENT (Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Diabetic Patients), REDUCE-IT (Evaluation of the Effect of AMR101 on Cardiovascular Health and Mortality in Hypertriglyceridemic Patients With Cardiovascular Disease or at High Risk for Cardiovascular Disease: Reduction of Cardiovascular Events With EPA – Intervention Trial), and STRENGTH (Effect of High-Dose Omega-3 Fatty Acids vs Corn Oil on Major Adverse Cardiovascular Events in Patients at High Cardiovascular Risk) trials, hsCRP proved to be a stronger predictor of recurrent myocardial infarction, stroke, and cardiovascular death than that of LDL cholesterol (Figure 6A).51 Moreover, risks for recurrent events were quite high for those with hsCRP >2 mg/L despite having LDL cholesterol levels <70 mg/dL, demonstrating the unmet clinical need for anti-inflammatory approaches in contemporary practice (Figure 6B).51 The strongest association for hsCRP was for the endpoint of cardiovascular death, suggesting that untamed inflammation is indicative of major life-threatening events. Very similar data have been reported in a contemporary study of 13,970 high-risk individuals with statin intolerance.52 In a 2024 prospective registry inclusive of 84,399 patients with atherosclerosis undergoing hsCRP testing in Sweden, 60% had hsCRP >2 mg/L despite aggressive contemporary care and again experienced poor clinical outcomes.53Figure 6Figure 6 Residual Inflammatory Risk as Assessed by hsCRP andResidual Cholesterol Risk as Assessed by LDL Cholesterol as Predictors of Future Cardiovascular Events and Death(Top) Following statin therapy, risks of cardiovascular death are greater for individuals with increasing levels of high-sensitivity C-reactive protein (hsCRP) (black) than for individuals with increasing levels of low-density lipoprotein (LDL) cholesterol (white). (Bottom) Following statin therapy, risks of cardiovascular death are high among those with elevated hsCRP and low LDL cholesterol, but conversely low among those with low hsCRP and elevated LDL cholesterol. Reproduced with permission from Ridker et al.51
Hazard Ratio Interpretation: The results of a Google search on the meaning of Hazard Ratio
Broad screening of almost all secondary prevention patients for hsCRP and “residual inflammatory risk” represents a major clinical opportunity.29 As demonstrated in CANTOS (Canakinumab Anti-Inflammatory Thrombosis Outcomes Study),3 targeted inhibition of the interleukin-1 (IL-1) to IL-6 to CRP pathway of innate immunity reduced recurrent vascular events among stable statin-treated patients by 15% to 17%, an effect as large as that anticipated from proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibition,54,55 yet a benefit achieved without any change in LDL cholesterol or apolipoprotein(b) concentration. Although additional benefits of canakinumab in CANTOS were observed for anemia, gout, large-joint arthritis, and lung cancer, adverse effects included small but statistically significant reductions in neutrophils and a small increase in risk of infections. Whereas CANTOS provided proof of principle for the inflammation hypothesis of atherothrombosis, canakinumab is not available for cardiovascular use, because its primary role remains as an orphan drug used for rare individuals with IL-1 overexpression syndromes and its experimental role has shifted to the treatment and “interception” of lung cancer.56
Fortunately, the inexpensive anti-inflammatory agent low-dose colchicine (0.5 mg daily) has now been shown in COLCOT (Colchicine Cardiovascular Outcomes Trial)13 and the LoDoCo2 (Low Dose Colchicine) for secondary prevention of CVD17 randomized trials to reduce recurrent cardiovascular events among patients with chronic stable atherosclerosis by 25%. A comparable 16% reduction in recurrent cardiovascular events has been observed with colchicine in a recent trial of those with prior stroke, although that effect was not statistically significant.57 By contrast, in the CLEAR-SYNERGY (Colchicine and Spironolactone in Patients with MI/SYNERGY) Stent Registry, which was a 2×2 factorial trial of colchicine and spironolactone, colchicine was not effective when initiated in the setting of acute STEMI.12 Interpretation of CLEAR-SYNERGY, however, has proven to be complex. First, acute STEMI is a time where proven therapies largely relate to reperfusion and restoration of blood flow suggesting that the “timing of taming of inflammation” will be important in clinical practice.58 Second, the COVID-19 pandemic markedly impacted trial results; prior to COVID-19, the hazard ratio for colchicine in CLEAR-SYNERGY indicated a 22% reduction in cardiovascular risk (HR: 0.78; 95% CI: 0.60-1.02), data consistent with the preceding COLCOT and LoDoCo2 trials. Yet, after the onset of COVID—a time of global inflammation when access to care changed radically and clinical trials were difficult to monitor and conduct—no benefit of colchicine was observed raising concern about study drug adherence and compliance during the pandemic. This issue may help explain why the spironolactone arm of CLEAR-SYNERGY also failed to show benefit. Third, although 120 global sites participated in CLEAR-SYNERGY, more than a third of the total trial participants (2,589 patients) were enrolled from 4 sites in 1 small Eastern European country. Although extensive commentary has been made regarding these limitations,59-63 it is important to recognize that CLEAR-SYNERGY is also the largest colchicine trial conducted to date. On the other hand, updated meta-analyses inclusive of the neutral CLEAR-SYNERGY data indicate an overall 25% relative risk reduction in major adverse cardiovascular events (HR: 0.75; 95% CI: 0.56-0.93).64
Currently, low-dose colchicine (0.5 mg daily) is approved by the U.S. Food and Drug Administration to reduce the risk of myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with established atherosclerotic disease or with multiple risk factors for CVD. Because colchicine is renally and hepatically metabolized, use should be limited to those with preserved renal and hepatic function and temporarily stopped if concomitant therapies that may alter colchicine metabolism are being used, such as clarithromycin, ketoconazole, fluconazole, or cyclosporin.65 Despite significant evidence of efficacy and safety, the use of inexpensive low-dose colchicine in the Unites States and globally remains infrequent.66
Consensus recommendations: hsCRP screening and anti-inflammatory approaches in secondary prevention
▪ Among individuals with known cardiovascular disease both treated and not treated with statins, hsCRP is at least as powerful a predictor of recurrent vascular events as that of LDL cholesterol, demonstrating the importance of “residual inflammatory risk” in contemporary practice.▪ Among individuals taking statin therapy, consideration should be given to increase dosage into the higher intensity range if hsCRP levels remain >2 mg/L, irrespective of LDL cholesterol.▪ Low-dose colchicine reduces cardiovascular events among individuals with chronic stable atherosclerosis and is the first U.S. Food and Drug Administration–approved anti-inflammatory agent for this purpose.▪ Low-dose colchicine is intended to be used as an adjunct to lipid lowering; however, it has not proven effective when initiated at the time of acute ischemia and should be avoided among individuals with significant liver or renal disease.▪ Several novel anti-inflammatory agents are now being evaluated in ongoing randomized trials in the settings of chronic kidney disease, dialysis, HFpEF, and acute coronary syndrome.Inflammatory pathways in behavioral and lifestyle risks
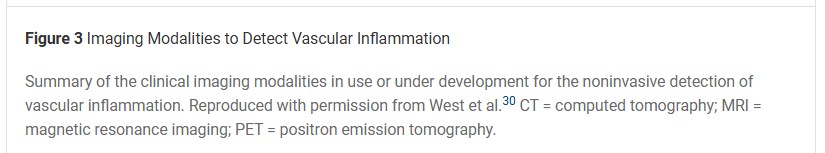
Recent evidence from 3 prospective cohorts, including >200,000 participants, indicates that proinflammatory dietary patterns are associated with increased risk of CVD.69 Conversely, the PREDIMED (Primary Prevention of Cardiovascular Disease With a Mediterranean Diet Supplemented With Extra-Virgin Olive Oil or Nuts)* randomized controlled trial showed that adherence with a calorie-restricted Mediterranean diet supplemented with extra-virgin olive oil or nuts reduced inflammation and major cardiovascular events compared with a low-fat diet in high-risk patients.19 Furthermore, lifelong intake of fish has been associated with a lower risk of CVD events in 24 prospective studies with 714,526 individuals from several countries.70,71 Plasma levels of EPA and docosahexaenoic acid (DHA), the polyunsaturated fatty acids in fish, may account for the benefit.In the prospective Cardiovascular Health Study of 2,692 U.S. adults free of coronary artery disease in 1992, higher plasma levels of omega-3 fatty acids were associated with a 27% lower rate of total mortality due to fewer CVD deaths at 16-year follow-up (HR: 0.73; 95% CI: 0.61-0.86; P-trend = 0.008).72 In the prospective MESA (Multi-Ethnic Study of Atherosclerosis) trial, the highest quartiles of plasma EPA and DHA levels were associated with HRs of 0.49 and 0.39, respectively, for incident CVD compared with the lowest quartile at 8 to 10 years of follow-up.73 In 19 international studies of 45,637 individuals free of CHD, the highest quintiles of EPA and DHA were associated with 29% and 23% lower rates of nonfatal myocardial infarction (relative risk: 0.71; 95% CI: 0.56-0.90) and fatal CHD (relative risk: 0.77; 95% CI: 0.64-0.89), respectively.74 Moreover, total mortality was 18% lower in 17 prospective studies (P < 0.003).75 It should be noted that a meta-analysis of 7 randomized controlled trials involving 81,210 subjects found that long-term marine omega-3 fatty acid supplementation was associated with an increased risk of atrial fibrillation.76 In analyses stratified by dose, the risk was greater in trials that used doses >1 g/d (HR: 1.49 [95% CI: 1.04-2.15]; P = 0.042) and the risk rose by 11% for each additional gram per day compared with those using ≤1 g/d (HR: 1.12 [95% CI: 1.03-1.22]; P = 0.024; P for interaction <0.001); however, no increased risk of atrial fibrillation was noted in the long-term prospective studies of dietary intake of fish.A 2021 meta-analysis of 40 randomized controlled trials reported a dose-dependent effect of EPA+DHA for CVD events and myocardial infarction.77 It was estimated that every 1 g/d EPA+DHA corresponded with a 9% and 7% lower risk of myocardial infarction and total CHD, respectively, and to a 5.8% lower risk of CVD events. The dose-response benefit may explain why randomized controlled trials with low or moderate doses of omega-3 fatty acids found no significant CHD risk reduction. The benefit from fish consumption may be attributed to SPMs, the downstream products of EPA and DHA that help resolve acute inflammation by halting neutrophil recruitment to inflamed tissues. Additionally, SPMs promote the efferocytosis of apoptotic neutrophils and debris, which is crucial for resolving and preventing chronic inflammation.78,79 SPM levels have also been shown to predict regression and progression of coronary plaque in the setting of low levels of hsCRP.74Other behaviors and lifestyles, including smoking and physical activity, have effects on inflammation. Chronic physical activity reduces resting C-reactive protein levels by multiple mechanisms, including a decrease in cytokine production by adipose tissue, skeletal muscles, endothelial and blood mononuclear cells: improved endothelial function, and insulin sensitivity.80 Regular exercise also reduces inflammation by increasing SPM production in humans and stimulating the catabolism of inflammatory lipid mediators, leukotrienes, and prostaglandins,81-83 and is associated with a reduction in CVD events.84 Smoking is a major source of inflammation in the body, leading to an increase in proinflammatory cytokines and reduced production and function of resolvins, making them less effective at resolving inflammation.81 Implementing these lifestyle interventions can lead to significant reduction in inflammatory burden and lower CVD risk.Consensus recommendations: inflammatory pathways in behavioral and lifestyle risks
▪ Focus on anti-inflammatory patterns like the Mediterranean or Dietary Approaches to Stop Hypertension diet.○ Emphasize consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil.○ Increase dietary intake of omega-3 fatty acids; 2-3 fish meals/week are recommended—preferably fatty fish high in EPA+DHA.○ Minimize red and processed meats, refined carbohydrates, and sugary beverages.▪ Engage in ≥150 minutes per week of moderate or 75 minutes of vigorous aerobic exercise to help reduce chronic low-grade inflammation.▪ Quit smoking to reduce chronic low-grade inflammation to lower the risk of ASCVD.▪ Maintain a healthy weight to attenuate systemic inflammation and decrease the risk of ASCVD.Inflammation in HF and other CVD
HF is characterized by systemic and local activation of the noncellular and cellular components of the immune system that lead to pathological tissue remodeling and disease pathogenesis.5,85-87 Immune system activation occurs as a chronic low-grade inflammatory response to ongoing tissue injury (ie, parainflammation88) induced by factors such as excessive neurohormonal activation and ongoing mechanical load.85 In chronic HF, this parainflammatory response is marked by increased elaboration of inflammatory cytokines and chemokines, expansion of resident and infiltrating innate immune cells (eg, macrophages), and adaptive immune cells (eg, T cells). Augmented immunoinflammatory responses have been linked with increased mortality and morbidity in chronic HF.89,90Hematopoietic factors that augment inflammatory responses, such as clonal hematopoiesis of indeterminate potential, have been shown to predict risk in HF.91 Specific cell types have unique functional, spatial, and temporal profiles in the failing heart and systemically, linked with disease stage and acuity.86 Interestingly, immune cells such as macrophages also contribute to atrial and ventricular arrhythmias in HF through direct coupling with cardiomyocytes and indirect effects on the microenvironment.92,93 The observations that specific immune cells, and their inflammatory profiles, can play causal roles in the pathogenesis of HF and CVD have led to rapid expansion of the field of cardioimmunology, which provides a broader understanding of the links between the immune system and heart disease, and helps identify therapeutic targets to suppress detrimental inflammatory and immune responses.87,94Phase 3 clinical trials (reviewed by Adamo et al85 and Mann87) that have targeted inflammation in ischemic and nonischemic HF can be categorized as anti-cytokine approaches (ATTACH [Anti–Tumor Necrosis Factor (TNF) With Infliximab])8 and etanercept (RENEWAL [Randomized Etanercept Worldwide Evaluation]),21 anti–IL-1β with canakinumab (CANTOS),10 pleotropic anti-inflammatory therapies (prednisone,20,22 rosuvastatin in CORONA [Controlled Rosuvastatin Multinational Study in Heart Failure] and rosuvastatin and omega-3 polyunsaturated fatty acids in GISSI-HF [Effect of Rosuvastatin in Patients With Chronic Heart Failure],14,15,95 oxypurinol in OPT-HF18 [Oxypurinol in Patients With Symptomatic Heart Failure]), and immunomodulatory strategies (celacade in ACCLAIM9 [Advanced Chronic Heart Failure CLinical Assessment of Immune Modulation Therapy]).To date, most of these trials have not demonstrated improvements in primary clinical endpoints such as cardiovascular death or HF hospitalizations, although significant improvements in left ventricular (LV) remodeling (improved LV ejection fraction, smaller LV volume) were observed in the TIMIC (Immunosuppressive Therapy in Patients With Virus-Negative Inflammatory Cardiomyopathy) trial in subjects with chronic postmyocarditis HF treated with prednisone and azathioprine for 6 months,22 and reductions in cardiovascular hospitalizations were observed in older subjects (>60 years of age) with ischemic cardiomyopathy in the CORONA trial.14 Moreover, the omega-3 polyunsaturated fatty acid arm of the GISSI-HF trial demonstrated that 1 g daily of EPA+DHA modestly reduced both all-cause mortality and the composite of all-cause mortality and cardiovascular hospitalization in subjects with NYHA functional class II-IV HF, irrespective of cause or LV ejection fraction.95 A meta-analysis of 19 randomized controlled anti-inflammatory trials with 1,341 subjects with HF with reduced ejection fraction also indicated that immunomodulation improved LV ejection fraction and reduced LV size, albeit with a nonsignificant decrease in all-cause mortality.96 Most recently, a prespecified, exploratory analysis of the CANTOS trial indicated that canakinumab, a monoclonal antibody against IL-1β, resulted in a dose-dependent reduction in hospitalization for HF and composite of HF hospitalization and HF mortality in subjects with prior myocardial infarction and hsCRP >2 mg/L (Figure 7).10 This was the first trial to indicate potential benefit for anticytokine therapy in HF.Figure 7Figure 7 Incidence of Hospitalization for Heart Failure (A) and Hospitalization for Heart Failure or Heart Failure–Related Mortality (B) Among Participants in the CANTOS TrialIncidence of hospitalization for heart failure (A) and hospitalization for heart failure or heart-failure related mortality (B) among participants in the CANTOS Trial. The number at risk for each year is in the table below each figure. Reproduced with permission from Everett et al.10 CANTOS = Canakinumab Anti-Inflammatory Thrombosis Outcomes Study.Blood hsCRP and IL-6 are commonly elevated in patients with HF and, especially in HFpEF where it portends a poorer clinical status and higher risk outcomes.98-102 Although not directly immunomodulatory, incretin agonists such as semaglutide and tirzepatide consistently reduced hsCRP while improving health status and exercise tolerance in obesity-related HFpEF (STEP-HF [Effect of Semaglutide 2.4 mg Once Weekly on Function and Symptoms in Subjects with Obesity-related Heart Failure with Preserved Ejection Fraction] trial and SUMMIT [A Study of Tirzepatide in Participants With Heart Failure With Preserved Ejection Fraction (HFpEF) and Obesity]).103,104 These observations raise the possibility that directly targeting inflammatory mediators may also be of clinical benefit in HFpEF. The ongoing HERMES (Effects of Ziltivekimab Versus Placebo on Morbidity and Mortality in Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction and Systemic Inflammation) trial of ziltivekimab is evaluating the potential efficacy of IL-6 inhibition in subjects with HFpEF and hsCRP >2 mg/L.97Beyond proinflammatory cytokines, several preclinical studies have raised consideration for directly targeting specific immune cell populations in HF. Nonetheless, the choice of specific immune-cell population; timing, duration, and approach of intervention; and appropriate biochemical and imaging markers needed for follow-up are currently unclear and the focus of intense study. Potential approaches include blocking the CC-chemokine receptor or ligand 2 axis to prevent the infiltration of proinflammatory monocytes into the failing myocardium, and the CXC-motif chemokine receptor 3–CXC motif chemokine ligand 9–CXC motif chemokine ligand 10 signaling axis to prevent the recruitment of T cells.85 Although not being currently trialed in HF, T-cell activation blockade with abatacept, which binds cluster of differentiation 80/cluster of differentiation 86 costimulatory molecules on antigen-presenting cells, and ruxolitinib, a Janus kinase inhibitor, is being tested in patients with steroid-resistant immune checkpoint inhibitor–induced myocarditis.105,106 Whether similar approaches can be used in chronic HF remains to be determined.Consensus recommendations: inflammation in HF and other CVD
▪ Inflammatory and immune markers such as hsCRP and IL-6 may be used as risk predictors in chronic HF.▪ EPA+DHA may be considered as part of the management of patients with NYHA functional class II-IV HF, irrespective of etiology or LV ejection fraction.▪ Statins may be considered as a part of management for patients with ischemic HF and age >60 years.Anti-inflammatory therapy for recurrent pericarditis
Anti-inflammatory therapy is standard of care for acute and recurrent pericarditis. For most patients, pericarditis of idiopathic or viral cause can be effectively treated with a short course of high-dose nonsteroidal anti-inflammatory drugs with doses tapered as C-reactive protein levels normalize. Based upon the ICAP (Investigation on Colchicine for Acute Pericarditis) trial6 where systemic anti-inflammatory therapy reduced recurrent pericarditis by 50%, a 3-month course of daily low-dose colchicine is recommended in current guidelines.107,108 Similarly, the COPPS-2 (Colchicine for Prevention of the Post-Pericardiotomy Syndrome and Post-Operative Atrial Fibrillation) randomized trial of patients undergoing cardiac surgery demonstrated a reduction in postoperative pericarditis from 29.4% to 19.4% with use of 1 month of low-dose colchicine initiated 48 to 72 hours before surgery.109Until recently, the only pharmacological option for high-risk patients with persistent and recurrent pericarditis was corticosteroids; however, randomized trial data have demonstrated considerable efficacy for IL-1 blockade among selected patients with multiple recurrent episodes of pericarditis who are resistant to colchicine and steroids and who have hsCRP levels >10 mg/L. In the AIRTRIP (Anakinra Treatment of Recurrent Idiopathic Pericarditis) trial of patients with idiopathic corticosteroid-dependent pericarditis and ≥3 prior recurrences, IL-1 blockade reduced recurrent event rates from 90% to 18%.110 In RHAPSODY (Study to Assess the Efficacy and Safety of Rilonacept Treatment in Participants With Recurrent Pericarditis) patients with ≥2 episodes of recurrent pericarditis, 6.7% had a recurrence on continuation of rilonacept as compared with a recurrence rate of 74% among those who discontinued therapy.7 In a third small trial, allocation to goflikicept resulted in a 90% reduction in recurrent pericarditis compared with those randomly allocated to drug withdrawal111 (Figure 8).Figure 8 Time to Pericarditis Recurrence in Anti–Interleukin-1 Agents Randomized Withdrawal TrialsTime to recurrent pericarditis in anti–interleukin-1 agent randomized withdrawal trials. Reproduced with permission from Klein et al.112These randomized trial data for the prevention and treatment of recurrent pericarditis demonstrate that targeted anti-inflammatory therapy has a clearly established role in cardiovascular medicine. It is not recommended to use any of these novel therapies in regions where tuberculosis is the most common cause of pericarditis.Consensus recommendations: anti-inflammatory therapy for recurrent pericarditis
▪ IL-1 blockade may be considered among select patients with multiple recurrent episodes of colchicine- and steroid-resistant pericarditis, with hsCRP levels >10 mg/L, in the absence of tuberculosis.▪ Novel anti-inflammatory therapies for recurrent pericarditis represent an important therapeutic advance for high-risk patients.Evidence gaps and future directions
Several recent seminal clinical trials support the recommendations summarized in Table 2.2,3 Nevertheless, significant gaps remain in the evidence needed to fully inform comprehensive detection, evaluation, and clinical management of CVD. The underlying molecular and cellular mechanisms for these findings often remain incompletely elucidated.In primary and secondary prevention of CVD where the most compelling evidence exists for the role of anti-inflammatory strategies in clinical practice, there remains an important gap in dissemination and implementation research. For example, strategies are needed to boost the sustained uptake of hsCRP measurement in routine clinical practice to identify individuals at increased inflammatory risk.Call to action: inflammation and CVD
The evidence linking chronic, low-grade inflammation to the initiation and progression of ASCVD is robust, and several seminal randomized controlled clinical trials demonstrate that targeting inflammation reduces cardiovascular risk independent of lipid lowering. We have thus entered an era when the evidence linking inflammation with ASCVD is no longer exploratory but is compelling and clinically actionable. Yet, clinicians will not treat what they do not measure. Therefore, the time has come for clinical practice guidelines to implement broad screening of primary and secondary prevention patients for hsCRP, in combination with LDL cholesterol, and to embrace anti-inflammatory interventions in patients with established ASCVD and evidence of residual inflammatory risk, regardless of LDL cholesterol level. The time is also ripe for the development of strategies to promote increased physician awareness of the crucial role of inflammation in CVD and accelerate the adoption of evidence-based, guideline-directed anti-inflammatory therapy through dissemination and implementation research. Because weight reduction, exercise, and smoking cessation can reduce hsCRP, endorsement of inflammation biology will further promote primordial and primary prevention. Inflammation is also strongly implicated in diverse cardiovascular conditions, including pericarditis, HF, and acute coronary ischemia; there is strong need for further research into the inflammatory and immune mechanisms underlying these conditions so that new anti-inflammatory or immunomodulatory treatment strategies can be identified and developed for translation to humans. The time for action has arrived.