I remind occasional visitors that these posts are basically my study notes (peripheral brain). The software’s great search function allows me to rapidly find any topic I’m interested in.
Here are two great podcast resources on pediatric urinary tract infection from Emergency Medicine Cases:
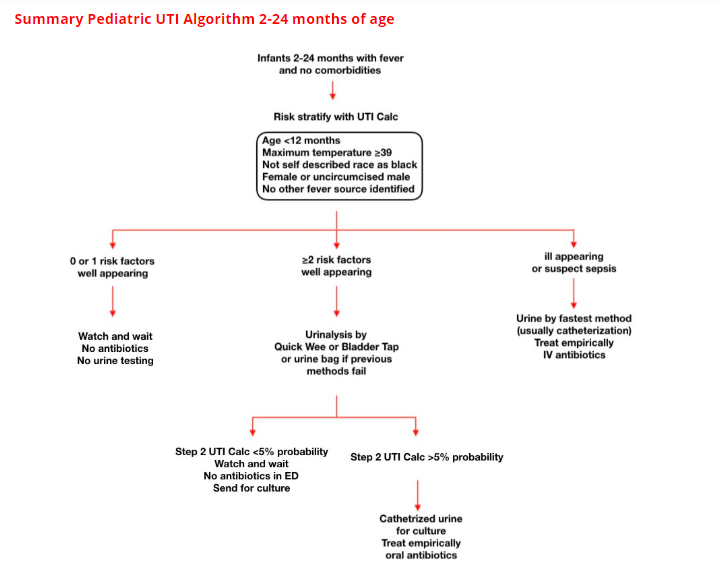
It is important to remember that everything on Pediatric UTI in these podcasts applies only to those less than two years old but greater than 8 weeks old who who do not appear to be sick.
That is, these patients are alert and acting appropriately, are taking fluids well, have a non-worrisome physical exam (and a normal capillary refill).
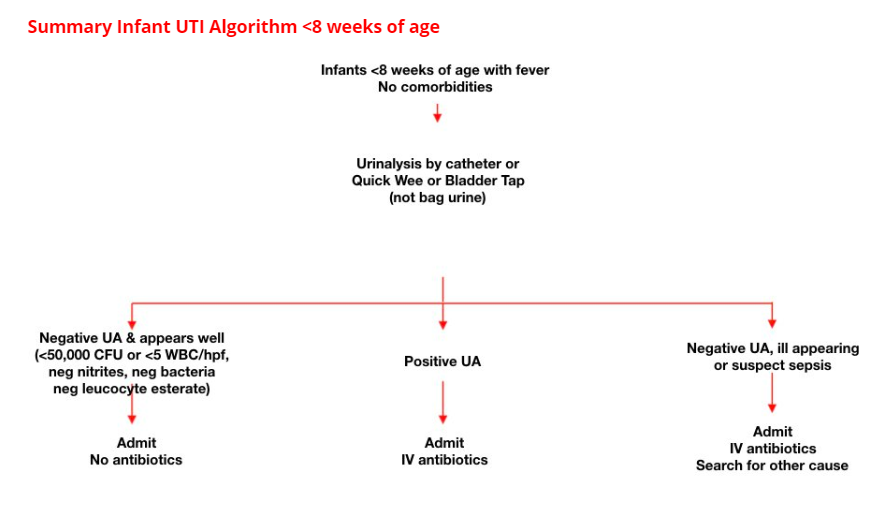
For newborns to eight weeks with fever, even if well-appearing, be very wary.
- BCE 79 Pediatric UTI – Choosing Wisely
- “In anticipation of EM Cases Episode 123 Pediatric UTI Myths and Misconceptions, Dr. Olivia Ostrow, Pediatric Emergency Physician at Hospital for Sick Children, Assistant professor at the University of Toronto and a Medical Safety Leader with an academic focus in quality improvement, discusses a case that exemplifies how indiscriminate work up of pediatric UTI can lead to over-testing, over-treating and even worse outcomes. In the upcoming main episode podcast we will discuss risk stratification, who to test, how to test, urinalysis interpretation, indications for blood tests, antibiotics of choice, which children require imaging and much more…”
- Ep 123 Pediatric UTI Myths and Misperceptions
- “On the one hand, UTI is one of the most common bacterial infections in children younger than 2 years of age and could lead to sepsis acutely and theoretically renal failure in the long run. On the other hand, it is important not to over-diagnose UTIs because we know that overuse of antibiotics increases costs, side effects and leads to antibiotic resistance. The first principles questions very much apply here: who to screen, how to screen, and what to do with the screen results. There are risks associated with not having a standardized approach to diagnosing pediatric UTIs. In this EM Cases main episode podcast with Dr. Olivia Ostrow and Dr. Michelle Science we discuss an approach to diagnosing pediatric UTIs whilst revealing some common pediatric UTI myths and misperceptions….”
Here are some excerpts from Ep 123 Pediatric UTI Myths and Misperceptions [but go ahead and review the entire show notes as they have much more in them – note to myself]:
Clinical presentation of pediatric UTI
While the presentation in infants is very non-specific and can include vomiting, poor feeding, lethargy, failure to thrive, jaundice, or isolated fever, older children who are toilet trained are more likely to present with the classic symptoms of UTI including dysuria, frequency, hematuria, incontinence, back pain, and abdominal pain. Observational data reveal that 7% of children 2-24 months of age presenting to the ED with isolated fever without a source have a UTI [6].
Urinalysis interpretation in pediatric UTI
Dipstick urinalysis is commonly used in the ED to support the diagnosis of a UTI, but it has poor specificity, especially when nitrates are negative. This can lead to over diagnosis of UTIs; 49% of patients with presumed UTI based on urine dipstick had negative urine cultures in a recent study [10].
No single element of a urinalysis is sensitive enough to rule in or out UTI.
Nitrites are highly specific but not sensitive for UTI.
Leukocyte esterase is sensitive but not very specific for UTI.
A recent study from the PECARN group [11] looked at accuracy of urinalysis in 4147 febrile infants <60 days old. The prevalence of UTI was 7% in this cohort. Urinalysis was highly accurate in predicting a final diagnosis of UTI with a sensitivity of 94% and specificity of 91% for colony counts >50,000, and for predicting bacteremia with a sensitivity of 100% and specificity of 91%.
If urinalysis of fresh (less than 1 hour since void) urine yields negative leukocyte esterase and nitrite results, then it is reasonable to monitor the clinical course without initiating antimicrobial therapy (watchful waiting), recognizing that a negative urinalysis does not rule out a UTI with certainty.
Disposition for pediatric UTI
Infants up to 28 days of age with a fever should be admitted to hospital but disposition is more controversial for older infants. There is good evidence to suggest that well-appearing children >2 months of age with a diagnosis of UTI who are tolerating oral fluids and have stable vital signs can be discharged home on oral antibiotics [15].
Factors to consider for hospital admission:
- Patients who are toxemic or septic
- Patients with signs of urinary obstruction or significant underlying urologic disease or other comorbidities
- Patients unable to tolerate adequate oral fluids or medications
- Infants younger than 2 months with febrile UTI (presumed pyelonephritis)
- All infants younger than 1 month with suspected UTI, even if not febrile
Resources:
(1) Ep 123 Pediatric UTI Myths and Misperceptions Helman, A. Ostrow, O. Science, M. Pediatric UTI Myths and Misperceptions. Emergency Medicine Cases. April, 2019. Accessed 4-25-2019.
(2) Urinary Catheterization in Infants: When It’s Knot so Simple [PubMed Abstract] [Full Text HTML] [Full PDF]. Clin Pract Cases Emerg Med. 2018 Jan 11;2(1):55-57. doi: 10.5811/cpcem.2017.11.36438. eCollection 2018 Feb.
(3) Urinary tract infection: Clinical practice guideline for diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Pediatrics. 2011 Sep;128(3):595-610. doi: 10.1542/peds.2011-1330. Epub 2011 Aug 28.
(4) Urinary Catheterization Of The Infant May 2011