In addition to today’s resource, I have reviewed and link to*
*Note to myself: I didn’t find this resource that helpful.
- Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Clinical Infectious Diseases, Volume 73, Issue 5, 1 September 2021, Pages e1029–e1044, https://doi.org/10.1093/cid/ciab549
Published: 14 June 2021
Today, I review and link to the show notes from C difficile infection – what ED docs need to know from EM Quick Hits 52.*
*Helman, A. Ostrow, O. Long, B. McLaren, J. Mullally, J. Petrosoniak, A. Morgenstern J. EM Quick Hits 54 – Button Battery Ingestion, C. difficile, ECG in Tox, Bed Bugs, Fibrinogen in Trauma, Cold Air for Croup. Emergency Medicine Cases. January, 2024. https://emergencymedicinecases.com/em-quick-hits-january-2024/. Accessed January 25, 2024.
All that follows is from the above resource.
C difficile infection – what ED docs need to know (19:15 – 26:30)
Clostridioides difficile is an anaerobic Gram-positive, spore-forming, enterotoxin-producing bacterium that causes watery diarrhea. About 10% of patients presenting to the ED with diarrhea have c difficile infection (CDI).
Risk factors for CDI may include:
- Antibiotic use: Fluoroquinolones, beta-lactam and beta-lactamase inhibitors, third- and fourth-generation cephalosporins, carbapenems, and clindamycin. Even a single dose can cause c diff.
- Health care exposure.
- Patient health factors including inflammatory bowel disease, HIV, recent GI surgery, tube feedings, malnutrition, obesity, female sex, low albumin, and older age.
- PPI use is also considered a risk factor, but this is controversial due to poor data.
- Up to 40% of patients with CDI don’t have a prior antibiotic risk factor, and up to 18% have no prior healthcare exposure.
Suspect CDI in the following patient presentations:
- Ill-appearing patient with diffuse, watery stools and recent antibiotic use and/or hospitalization.
- Abdominal pain (6-90%), fever (21-50%), bloody stools (5-21%) and watery diarrhea (55-84%). Diarrhea is often not an isolated symptom; nausea and vomiting can occur in up to 30%.
- Patients with acute onset of 3 or more unformed stools without explanation.
- Patients with GI symptoms plus constitutional symptoms, as well as a pertinent history of antibiotic use, comorbid conditions, and/or recent healthcare visits.
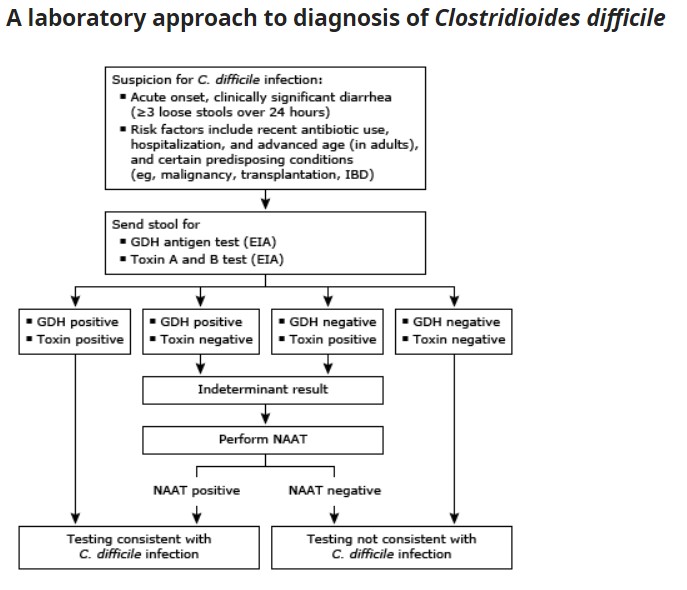
CDI testing centers on detection of the organism itself or the production of toxin A or B. Culture is not as feasible in the ED. The most common tests in the ED include toxin assay and nucleic acid amplification.
- Toxin assay is specific but has a sensitivity of only 50%-60%.
- NAAT is very sensitive, but it can’t distinguish infection from asymptomatic colonization, so only order the test if the patient has symptoms.
- IDSA guidelines emphasize using a two or three step algorithm based on laboratory capabilities and institution.
Treatment of c. difficile diarrhea depends on illness severity:
- Non-severe
- First episode: vancomycin 125 mg 4x per day for 10 days or fidaxomicin 200 mg 2x per day for 10 days. If these aren’t available, use metronidazole 500 mg 3x per day.
- Severe CDI includes WBC > 15,000 or creatinine > 1.5 mg/dl.
- Use vancomycin or fidaxomicin as above.
- Fulminant CDI includes signs of shock, vasopressor requirement, elevated lactate, or toxic megacolon (peritonitis, severe pain or tenderness, distension, and guarding. Imaging will show a significantly dilated diameter of the colon > 6 cm).
- Speak with GI and surgery early and use enteral vancomycin 500 mg 4x per day. This can be given orally and rectally. If ileus is present use vancomycin rectally.
- Recurrent infection is defined by 3 or more CDI episodes.
- If previously treated with oral metronidazole should be treated with oral vancomycin or fidaxomicin.
- Prevent the spread by washing hands with soap and water with these patients; the alcohol-based sanitizer does not kill the spores.